Medical Case Notes
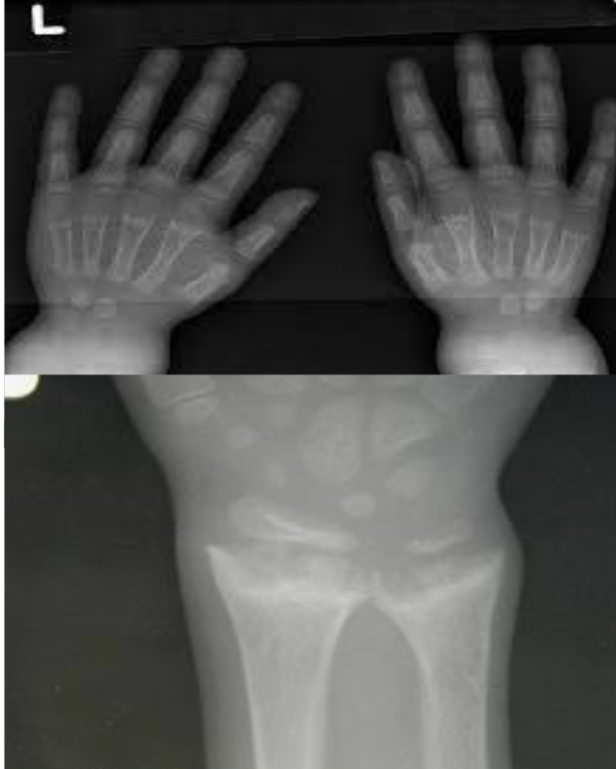
Nutritional Rickets
What are the clinical findings? 23-month-old with bowing legs, not growing properly, and exclusively breastfed until 11 months.
What are the X-ray findings? Widening, cupping, and fraying of metaphyseal regions, osteopenia, and widened and irregular epiphyseal plates.
What are the relevant investigations? Serum levels of calcium, phosphorus, alkaline phosphatase, and PTH.
Respiratory Alkalosis
What are the blood gas findings? pH 7.48, pCO2 2.9 kPa, pO2 15.5 kPa, Cl- 100 mM, Na+ 142 mM, K+ 3.2 mM, HCO3- 17 mM.
What is the likely diagnosis? Respiratory alkalosis.
What are the possible causes? Early pneumonia, asthma, mechanical ventilation, psychogenic causes, and drugs like salicylate poisoning.
Case: Infant with Poor Weight Gain
- 9-month-old infant with poor weight gain, recurrent chest infection, and cardiac murmur
- Write 2 abnormalities in the X-ray
- Differential diagnosis
- More likely right-left shunt, boot-shaped heart
- TOF if cyanosis

Child Abuse
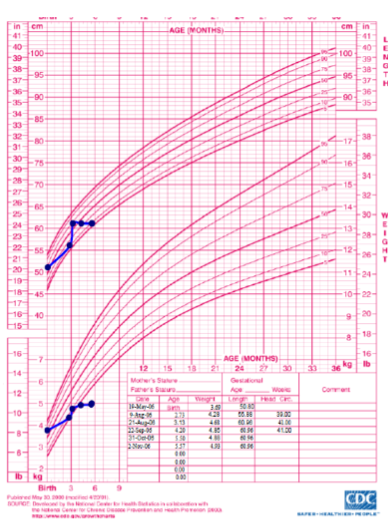
What is observed in the growth chart? Both height and weight lines cross two centile charts twice, indicating intermittent failure to thrive.
What is the likely diagnosis? Child abuse.
Case: ABG Interpretation
- 7.49 pH
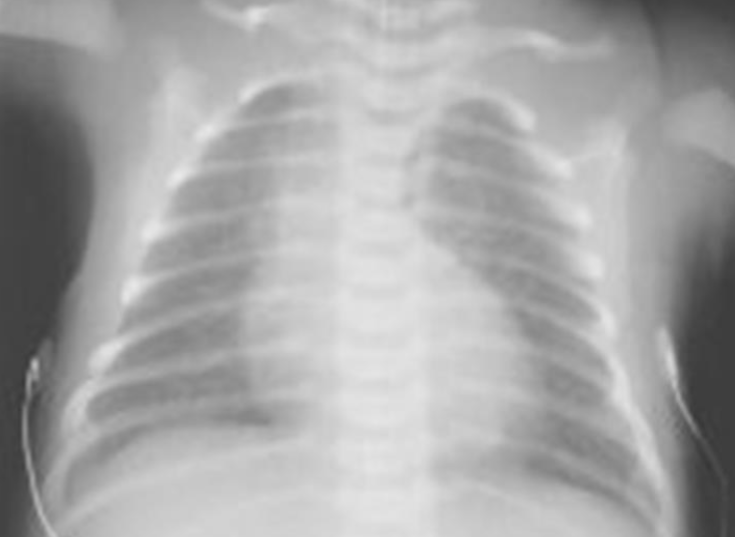
Case: Preterm Infant with Respiratory Distress
- Preterm 29 weeks gestation C/S delivery showed severe respiratory distress soon after birth - RDS
- Air bronchograms


-
There is a homogeneous opacification of both lungs with white-out lungs - (1 .field (grounds glass appearance) and air bronchogram bilaterally
-
.The diagnosis is Acute Respiratory Distress Syndrome (ARDS) - (2
-
**;The most common causes of ARDS are **
- .A- Bacterial or viral pneumonia
- .B- Sepsis
- .C- Major trauma
- .D- Major surgery
- .E- Massive aspiration pneumonitis
- .F- Severe poisoning and intoxication
- .G- Severe envenomation (snake bite and scorpion sting)
- .H- Severe and prolonged hypoxia
- .I- Massive blood transfusions Preterm 29-weeks gestation C/S delivery showed severe respiratory distress soon after birth. This chest x-ray was taken at the age of 6 hours.
- Q1: Write 2 abnormalities in the X-Ray?
- Q2: What is the likely diagnosis?
- Q3: Write 2 management steps.
Answers:
- Q1: Ground glass appearance, wide intercostal space.
- Q3: Mechanical ventilation, give Surfactant for lungs maturation.
What are the possible diagnoses? Congenital pneumonia or respiratory distress.

Case: High Anion Gap
- pH 4.21
- High anion gap + Acidic and hx DKA metabolic acidosis hyperglycemia
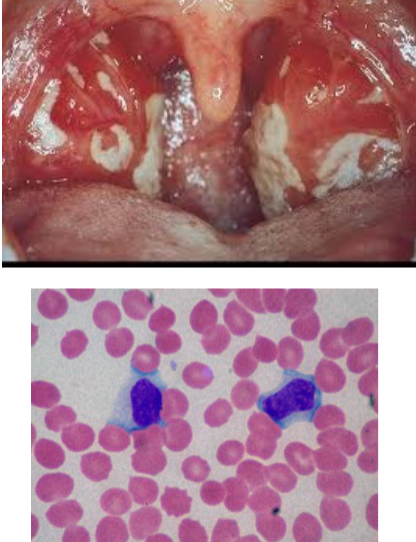
A 3-year-old child with fever for 8 days
-
Lymphadenopathy, splenomegaly, and numerous reactive or atypical lymphocytes on peripheral blood smear. The monospot test is negative.
-
A likely cause of this clinical picture is infection with? Epstein-Barr virus
-
Streptococcal, EBV, or diphtheria, white tonsil more in first two
-
Atypical lymphocytes
-
6.9 pH
-
Mixed acidosis
-
25.2 pO2
-
Respiratory mixed acidosis
Case 11: Celiac Disease
- Duodenum biopsy
Case 12: Edward Patau Syndrome
- 3rd below Edward head circumference
Case: Infant with Cyanosis

- Diagnosis: Transposition of great arteries TGA
- Description: EGG ON SIDE, generalized cardiomegaly, Narrow mediastinum
**2 Days old infant with cyanosis, tachypnea and grade 2 murmur. What is the likely diagnosis
Case: Aortic Coarctation
- Aortic root coarctation of aorta
Case 16: Genetic Syndromes
- William supravalvular stenosis
- Down syndrome VSD
Case 17: Heart Failure in Infant
- 4-month-old infant with heart failure, snowman figure of 8

- Description: snowman or figure of 8. Dilated vertical vein on the left and brachiocephalic vein on top + superior vena cava on the right form the head of the snowman. The body of the snowman is formed by the enlarged atrium.
- Diagnosis: Total Anomalous Pulmonary venous Drainage
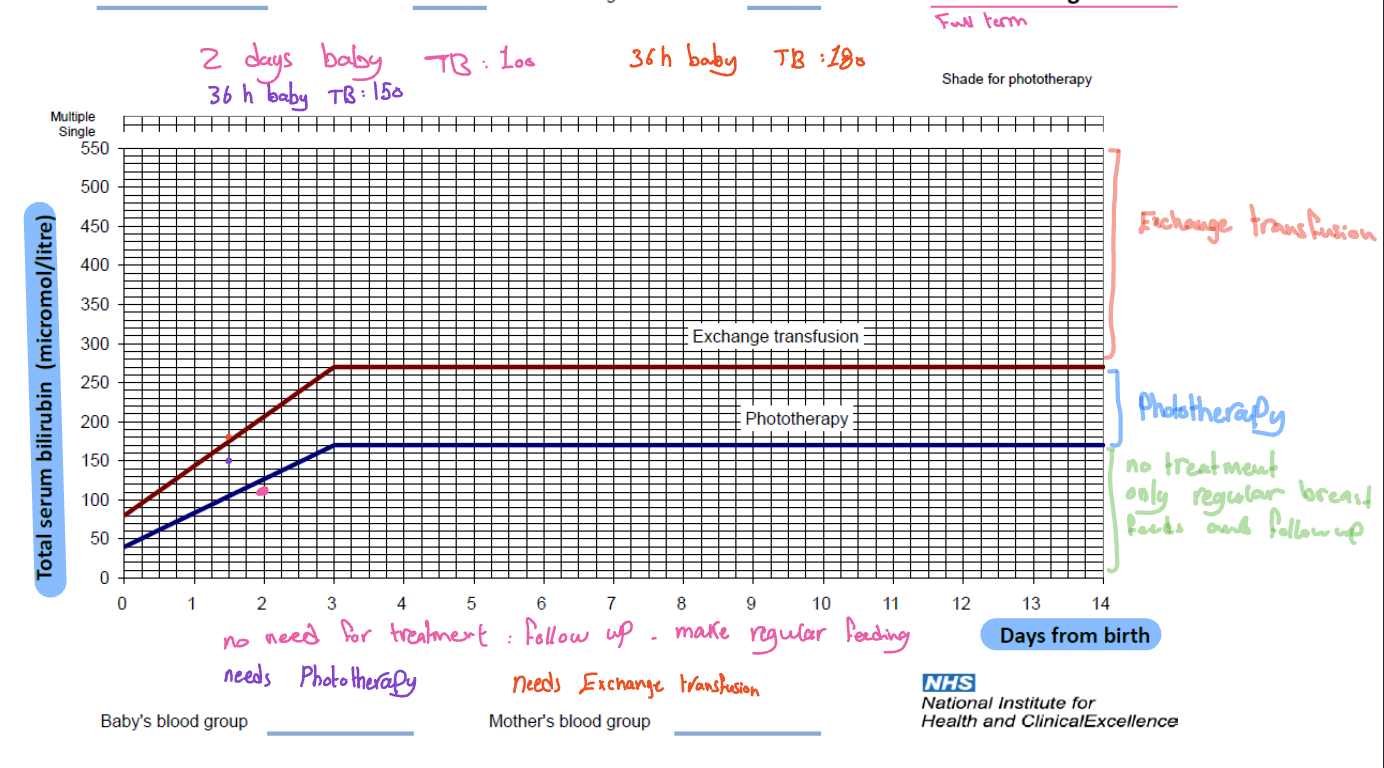
Case 22: Jaundiced Infant
- 3-week-old jaundiced infant referred to pediatric unit, birth weight 4 kg at term with hepatospleenomegaly no family hx of neonatal jaundice
- Total bilirubin 360, direct 230, ALP 480, ALP 467
- Cause of jaundice in this could be: hypothyroidism, breastfeeding, Gilbert syndrome, hepatosplenomegaly
- Neonatal hepatitis, cholelithiasis most likely

Instrument name
- Transcutaneous bilirubin test
- Uses? Measure the yellow staining so it can be used for screening
- Instrument used to forehead

Questions
- What is this Tx (treatment)?
- Intensive phototherapy
- What are the complications?
- Retinal damage, dehydration
- Complications: arrhythmia, dry skin, dehydration, retinopathy, brown bronze syndrome
Hemolytic Anemia (ABO Incompatibility)
Investigations:
- Haemoglobin: 12.1 gm/dL (14-22 gm/dL)
- Reticulocytes: 12% (2%)
- Total Bilirubin: 560 mol/L
- Direct Bilirubin: 30 mol/L
- Baby’s blood group: A-ve
- Maternal blood group: O-ve
- Direct antiglobulin test: Positive
What is the likely cause of the baby’s jaundice? Hemolytic anemia due to ABO incompatibility.
Jaundice Case:
- A 4-day-old infant is referred to the hospital because of jaundice. The jaundice commenced within the first 24 hours of life. His birth weight was 3.70 kg at term. He is doing well, afebrile, and no hepatosplenomegaly.
- Q1: What is the cause of this baby’s jaundice?
- Hemolysis due to ABO incompatibility.
- Q2: What are the complications?
- Anemia, kernicterus.
- Q3: What is the treatment?
- Blood transfusion, Phototherapy, Exchange transfusion
- Q1: What is the cause of this baby’s jaundice?
Therapies indicated as such
for exchange transfusion, phototherapy, and others
Case 25: Diaphragmatic Hernia
Case Study

Questions
- A- most important test
- ABG
- B- what is the diagnosis?
- Congenital diaphragmatic hernia
- C- what is the definitive treatment?
- Surgery
- D- give one association
- Lung hypoplasia
DIAPHRAGMATIC HERNIA:
- A newborn with left congenital diaphragmatic hernia. Note the scaphoid abdomen and the barrel-shaped chest.
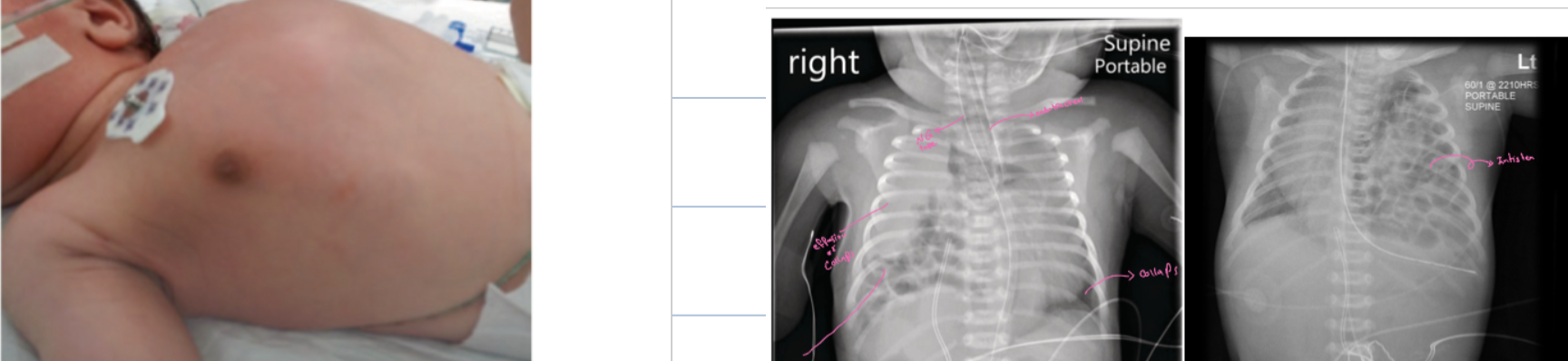

Full-term baby normal vaginal delivery
- Shows severe respiratory distress. Air entry impaired in the left side, and heart apex heard in the right side.
- What is the cause of this respiratory distress? Left side massive diaphragmatic hernia.
- Treatment: Surgical repair
Case 26: Anemia
- Central part decrease
- RBC different sizes, anisocytosis
- Iron deficiency anemia most likely
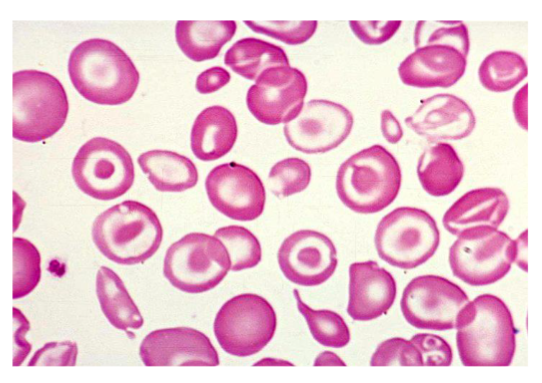
Case
Sign ? Target sign - hypochromic microcytic anisocytosis Diagnosis? Thalassemia/anemia
Case 27: CSF Sample Analysis CC
- CSF sample for 9-year-old boy with headache and fever
- Appearance clear
- WBC 500 cells/µL
- Type cell lymph 350
- Protein high 50 mg (20-40)
- Glucose slightly high
- RBC 5
- Write 2 abnormal findings
- Diagnosis
- Mention 2 other relevant investigations
- PMN 50
- Water two on floor?
- Interpretation of cerebrospinal fluid (CSF) bacterial
- Inv gram stain, CSF culture, PCR due viral - CT maybe for hepatic encephalitis
Case 28: Child Resuscitation
- Child resuscitates with single rescue CPR using ambu bag positive pressure???
cpr technique???
- CPR ambu bag and what??? 15-2? 3-2?
- Positive pressure ventilation & chest compression

Case 29: Rickets
- Rickets rosary on sides of chest X-ray may be child abuse
Case 30: Anemia
- Square graph showing microcytic microchromic anemia
Case 31: Pulse Oximeter
- Pulse oximeter
Case 32: Necrotizing Enterocolitis
- Necrotizing enterocolitis
- Give antibiotics
NECROTIZING ENTEROCOLITIS:
- (A) Dilated loops, Thickened bowel walls
- (B) Pneumatosis intestinalis (air in intestinal walls) because the distention
- Pneumoperitoneum
- Portal gas (present in the portal venous system)
- Pneumoperitoneum is an emergency requiring surgical intervention
- Portal gas represents air and is considered to be a poor prognostic sign.


X-ray finding
- Thick abdominal wall
- Dilated bowel loops
- Abnormal gas pattern
- Diagnosis? Necrotizing enterocolitis
- What is the most immediate action (therapy) you will provide? Broad-spectrum antibiotics
Case 33: Lumbar Puncture
| Indications for Lumbar Puncture | Contraindications for Lumbar Puncture |
|---|---|
| Suspected central nervous system (CNS) infections (e.g., meningitis, encephalitis) | Increased intracranial pressure (risk of brain herniation) |
| Diagnosis of subarachnoid hemorrhage (if CT is negative) | Local infection at the puncture site |
| Diagnosis of neurological conditions (e.g., multiple sclerosis, Guillain-Barré syndrome) | Coagulopathy or bleeding disorders |
| Measurement of cerebrospinal fluid (CSF) pressure | Severe thrombocytopenia (low platelet count) |
| Administration of intrathecal medications | Spinal cord mass or tumor |
| Therapeutic relief of increased intracranial pressure | Patient refusal or inability to cooperate |
Case 34: Toddler with Cough
- Toddler with cough
- Pneumonia
- Streptococcal pneumonia
Case 35: Pneumothorax
- Pneumothorax both lungs
Case 36: Fracture
- Ping pong fracture
- 4.9 girl fracture… right shoulder dystocia
Case 37: Transillumination
- Transillumination pneumothorax