Cardiac Cirrhosis - Peripheral feature of AR; Austin flint murmur
Etiology of AR
Acute:
- Infective endocarditis
- Acute rheumatic fever
- Ascending aortic dissection
- Failure of prosthetic valve
Chronic:
- Rheumatic Heart disease.
- Bicuspid valve disease: Commonest cause: young. | aortic sten/Mitral regurge
Aortic dilatation:
- Connective tissue disease (Marfan’s syndrome, Ehlers–Danlos syndrome).
- Vasculitis.
- Rheumatoid arthritis; Ankylosing spondylitis.
- SLE; Reactive arthritis.
- Late-stage syphilis (very rare).
- Thoracic aortic aneurysm.
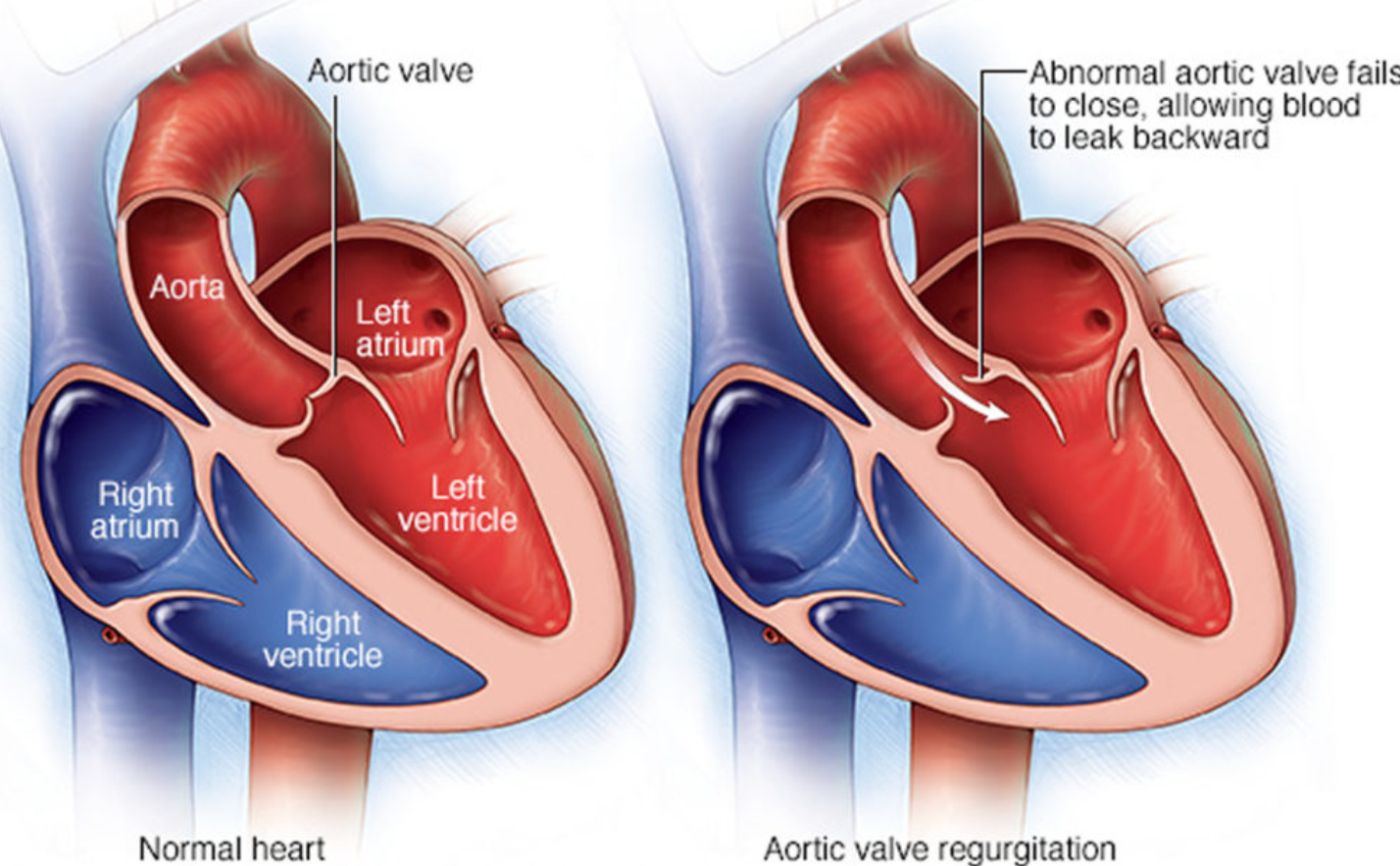
Aortic Regurgitation
Aortic regurgitation results from an incompetent aortic valve causing a regurgitant flow of blood in diastole.
- Usually presents 4th-6th decades of life.
- Affects males 3 times more commonly than women.
- Severe disease is seen in < 1% of the population.
- The most common causes are degenerative disease & congenital bicuspid valve.
Chronic Aortic Regurgitation
Primary valvular defect:
- Calcific aortic valve disease: Most common cause of AR in older patients in high-income countries.
Aortic dilatation:
- Connective tissue disorders (e.g., Marfan syndrome, Ehlers-Danlos syndrome).
- Chronic hypertension.
- Aortitis of any etiology (e.g., tertiary syphilis).
- Thoracic aortic aneurysm.
Pathophysiology Y
General: Regurgitation of blood from the aorta into the left ventricle (LV) leads to:
-
Water hammer pulse: Widened pulse pressure → ↑ systolic BP and ↓Diastolic BP (collapsing pulse). Seen in hyperdynamic circulation.
- Stroke volume increased → (high Systolic BP).
- Regurgitant volume increased → (Low Diastolic BP).
-
Acute AR:
-
LVED pressure ↑ rapidly → pressure transmits backward into pulmonary circulation → pulmonary edema and dyspnea.
-
↓ CO if severe → cardiogenic shock and myocardial ischemia.
-
-
Chronic AR:
-
Compensatory ↑ SV & adequate CO despite regurgitation (compensated HF).
-
↑LVED volume → LV enlargement and eccentric hypertrophy → left ventricular systolic dysfunction → decompensated heart failure.
-
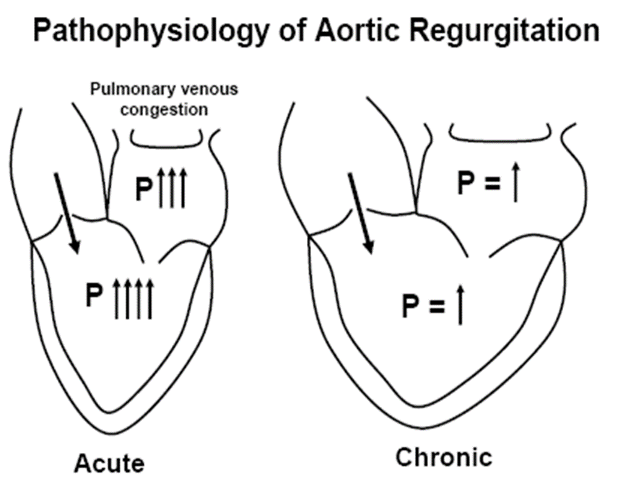
Blood flows back into the left ventricle from the aorta, meaning that the left ventricle has to overcome the increased volume in its subsequent contraction. A sharp increase in end-diastolic volume with a relatively non-compliant left ventricle causes an increase in heart rate and contractility to counteract the increasing preload. In acute aortic regurgitation, the left ventricle is of normal size and unable to compensate, leading to shortness of breath and pulmonary edema due to backward transmission of pressure through the pulmonary system. In chronic aortic regurgitation, there is compensation and ventricular remodeling, which leads to improved compliance. This eventually fails to provide adequate cardiac output, and heart failure symptoms ensue.
De-musset’s sign
Corrigan’s sign
Capillary pulsation
Z
Clinical Features
Acute Aortic Regurgitation:
- Collapsing (water hammer) pulse.
- Wide pulse pressure: most accurate.
- Diastolic murmur.
- Florid pulmonary edema.
Signs and symptoms:
- Sudden, severe SOB.
- Rapid cardiac decompensation 2nd to LVF.
- Symptoms underlying disease (fever; infective endocarditis, chest pain; coartication).
Auscultation:
- Soft and short early diastolic murmur.
- S3.
- High-pitched, blowing, decrescendo early diastolic murmur; best left 3-4 ICS at the border (Erb point).
- AR (aortic root disease): best along RT sternal border.
- Worsens with squatting and handgrip SDL.
- Austin Flint murmur: Rumbling, low-pitched, mid-diastolic at the apex: premature closure of the mitral leaflets.
In more severe stages: harsh, crescendo-decrescendo mid-systolic murmur that resembles the ejection murmur heard. AV RUST
Austin Flint
Physical Findings
Chronic Aortic Regurgitation: Signs and symptoms:
- Asymptomatic with progressive LV dilation.
- Palpitations.
- Symptoms of LVF.
causes collapsing?
Eponymous signs are associated with AR (these relate to high stroke volume associated with this condition):
- Water hammer pulse: Rapid upstroke and downstroke.
- Corrigan’s sign: Carotid pulsation.
- de Musset’s: Head nodding with each heartbeat.
- Quincke’s: Capillary pulsation in nail beds.
- Duroziez’s: Diastolic femoral murmur.
- Traube’s: ‘pistol shot’ sound auscultated over femoral Art.
- Müller’s: Systolic pulsation of uvula due to regurgitant blood striking the anterior leaflet of the mitral valve, which leads to…
Physical Exam Findings of AR
- Wide pulse pressure.
- Hyperdynamic and displaced apical impulse.
Auscultation:
- Diastolic blowing murmur at the left sternal border.
- Austin flint murmur (apex). z
- Systolic ejection murmur: due to increased flow across the aortic valve.
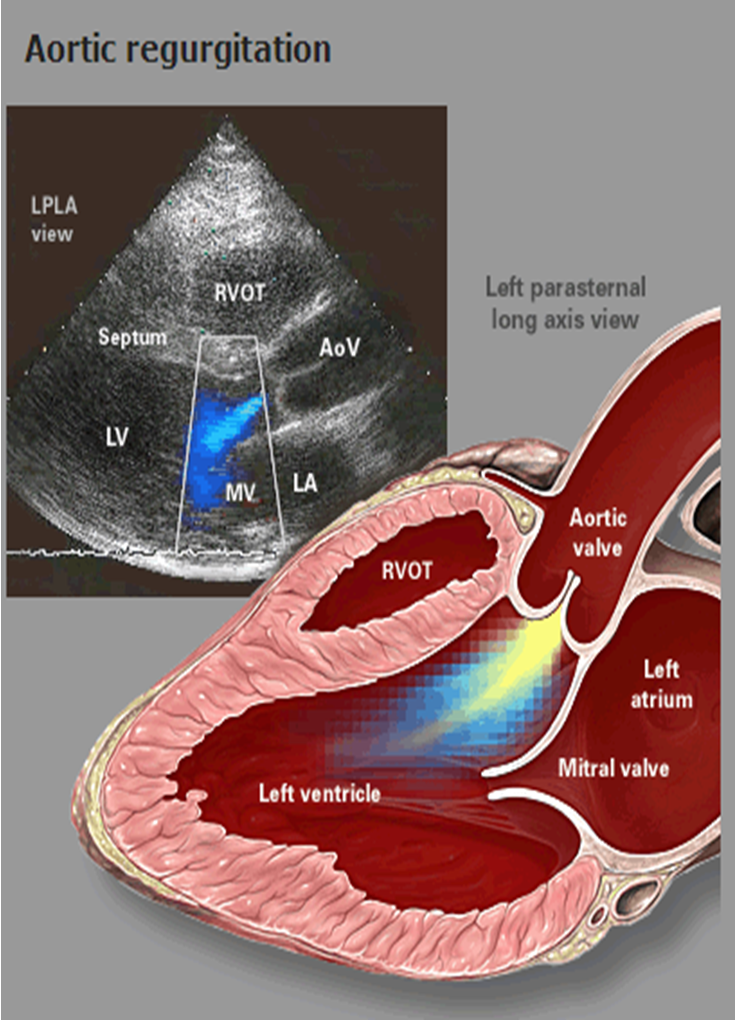
Investigations
- Echocardiography and Doppler (TTE): First-line diagnostic tool: assess the severity: LV dilatation.
- CXR:
- Cardiomegaly: Dilating ascending aorta.
- Pulmonary edema (Acute AR) with normal cardiac size.; crepitation
- ECG: LV hypertrophy.
- CTA Chest (or TEE): Best diagnostic tool if aortic dissection.
- Cardiac MRI: Inadequate Echo (Evaluate Anatomy).
- Cardiac catheterization: Inadequate Echo (Evaluate hemodynamic).
- Exercise stress testing: Assess fitness.
- Other investigations: Blood culture, BNP.
Findings specific to acute AR: CXR
- Reduced cardiac output.
- Elevated end-diastolic left ventricular pressure.
- Early mitral valve closing.
- (Regurgitant jet is diagnostic).
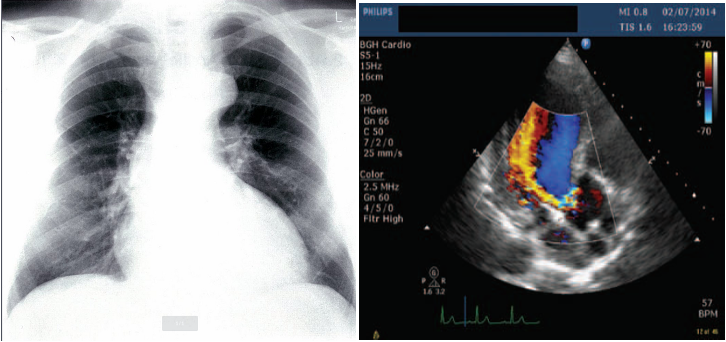
Imaging
A. Echocardiogram:
- Allows visualization of the origin of the regurgitant jet and its width, detection of aortic valve pathology and ventricular hypertrophy.
B. CXR:
- May demonstrate cardiomegaly.
- Dilated ascending aorta.
- Calcification may be seen.
Special:
- Cardiac MRI.
- Cardiac catheterization.
- ECG exercise stress testing.
Advanced Imaging
- Cardiac MRI:
- Indication: Moderate to severe AR (AR stage B–AR stage D) with inadequate echocardiographic imaging or a discrepancy between clinical presentation and echocardiographic findings.
- Objective: Precise evaluation of anatomy and hemodynamics.
- CTA chest:
- Acute AR: Indicated, especially if aortic dissection is suspected.
- Chronic AR: Not routinely recommended.
Cardiac Catheterization
- Diagnostic hemodynamic cardiac catheterization with aortography:
- Indication: Moderate to severe AR (AR stage B–AR stage D) with inadequate echocardiographic imaging or a discrepancy between clinical presentation and echocardiographic findings.
- Objective: Hemodynamic evaluation (e.g., severity of regurgitation, intracardiac pressures, cardiac function).
Coronary Angiography
- Indications: Preoperative cardiac risk stratification in patients with angina, reduced LVEF, signs of ischemia, or coronary risk factors.
Findings: Signs of CAD (e.g., coronary stenosis).
Exercise Stress Testing
- Indication: May be used to provoke possible exertional symptoms or assess fitness in patients with severe AR.
Findings: Symptoms of aortic regurgitation (e.g., dyspnea, angina).
Management of AR
Acute AR: (Usually symptomatic):
- Surgical therapy: Immediate (AVR) is indicated. Z
- Medical therapy: Vasodilators and inotropes.
Chronic AR: (Usually asymptomatic):
- Surgical therapy: Aortic valve replacement (AVR).
- Symptomatic chronic severe AR.
- In asymptomatic with LVEF ≤ 50% (Serial Echo).
- Advanced left ventricular dilatation.
- Severe AR undergoing cardiac surgery for other indications.
- Medical therapy:
- Treat HTN: Vasodilators (ACE-I); contraindicated in aortic stenosis
- ACE inhibitors/ARBs: Severe symptomatic AR and/or LV dysfunction when surgery is C/I.
- SBE (Subacute bacterial endocarditis) Prophylaxis.
Predictors of prognosis include left ventricular size, systolic function, and ejection fraction.
- Asymptomatic with LVEF >50% with a dilated LV (end-diastolic dimension >70mm or systolic dimension >50mm).
- Symptomatic patients: Mortality rate is > 10% per year.
Monitoring
- Serial echocardiography: Regular follow-up imaging is indicated for asymptomatic patients to identify possible progression and indications for intervention.
- Mild regurgitation (AR stage B): Every 3–5 years.
- Moderate regurgitation (AR stage B): Every 1–2 years.
- AR stage C1 regurgitation: Every 6–12 months.
On-demand imaging is indicated for patients with any change in signs or symptoms.
Medical Management
Acute aortic regurgitation:
- Medical management is focused on stabilizing hemodynamics prior to surgery, e.g., via:
- Management of cardiogenic shock with inoconstrictors or inodilators (e.g., dobutamine or dopamine).
- Afterload reduction with vasodilators for acute heart failure (e.g., nitroprusside).
- Beta-blockers may be indicated in aortic dissection; avoid in other causes of acute AR.
Avoid beta-blockers in acute AR, unless due to aortic dissection.
Chronic aortic regurgitation:
All patients should be screened and treated for other cardiac risk factors. No medical treatments are known to influence the progression of the disease.
- Hypertension:
- Initiate treatment if systolic blood pressure is > 140 mm Hg and follow standard hypertension guidelines.
- Vasodilators (e.g., ACE inhibitors, ARBs) may be preferable to beta-blockers.
- Heart failure: Manage according to guideline recommendations (see “Treatment of heart failure”).
Prophylactic antibiotics:
- At-risk patients, e.g., with prosthetic valves or a history of infective endocarditis: Consider antibiotic prophylaxis prior to certain dental procedures (see “Prophylaxis for endocarditis”).
- Rheumatic heart disease: Long-term secondary prophylaxis (see “Prevention” in “Rheumatic fever” for details).
Surgical Management
The choice of procedure depends on the cause of the valve defect and comorbidities. All patients with severe aortic regurgitation being considered for intervention should be evaluated by members of a heart valve team if feasible.
Indications:
- Acute severe AR.
- Symptomatic chronic severe AR (AR stage D).
- Asymptomatic chronic severe AR (AR stage C) with one of the following:
- Reduced LVEF ≤ 55%.
- Consider if LVESD > 50 mm.
- Cardiac surgery for other indications.
Surgical aortic valve replacement: Standard procedure for acute and chronic AR (see “Prosthetic heart valve” for details).
Alternative procedures:
- Valve-sparing repair of aortic sinuses and ascending aorta: May be considered if AR is caused by aortic dilatation, and the valve itself is unimpaired.
- Primary valve repair: Not routinely performed, but may be considered in isolated minor leaflet damage.
- Transcatheter aortic valve replacement: Not recommended for treatment of isolated AR.
Follow-up:
Complications of aortic valve replacement include arrhythmias, endocarditis, and thromboembolism.
Antithrombotic therapy for patients with prosthetic aortic valves depends on the choice of valve replacement (mechanical or bioprosthetic) and risk factors.
Case Study 1
A 62-year-old man presented with decreased exercise tolerance and progressive SOB. His pulse is 82/min, and BP: 155/53 mm Hg. Cardiac examination shows a high-pitched, decrescendo murmur immediately after S2 and is heard best along the left sternal border. There is an S3 gallop. Carotid pulses are strong. Which of the following is the most likely diagnosis?
- Mitral valve stenosis
- Mitral valve regurgitation
- Aortic valve regurgitation
- Aortic valve stenosis
Case Study 2
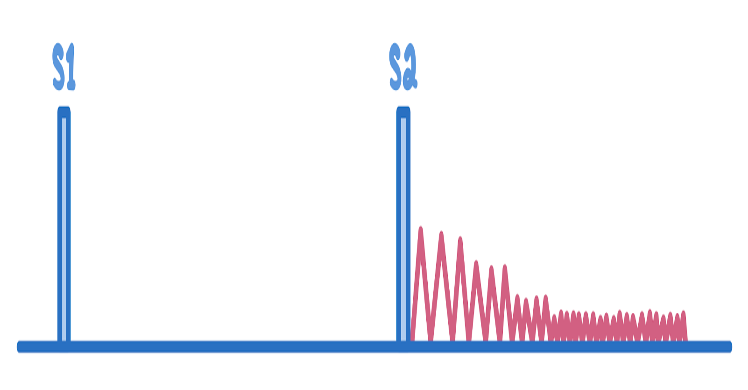
A 35-year-old man with Marfan syndrome presents with exertional dyspnea and pounding headaches for several months. His temperature is 37.0°C, pulse is 90/min, and blood pressure is 135/85 mmHg. On physical examination, the lungs are clear to auscultation. Cardiac auscultation reveals the murmur demonstrated below over the right sternal border. Palpation of the radial arteries shows a rapidly rising and falling arterial pulse. Which of the following is the most likely diagnosis?
- Patent ductus arteriosus
- Aortic regurgitation -
- Aortic stenosis
- Coarctation of the aorta -
- Mitral stenosis
Case Study 3
A 30-year-old woman presented with shortness of breath on exertion and occasional chest pain. Does not use tobacco, alcohol, or illicit drugs. She immigrated from Peru two years ago with her family. Her temperature is 36.4°C; pulse is 115/min, respirations are 24/min, and blood pressure is 130/60 mm Hg. Physical examination shows pulsations of the nail bed. Cardiac examination shows an abnormal heart sound over the left sternal border on auscultation (see image below). Which of the following maneuvers will likely decrease the intensity of this heart sound?
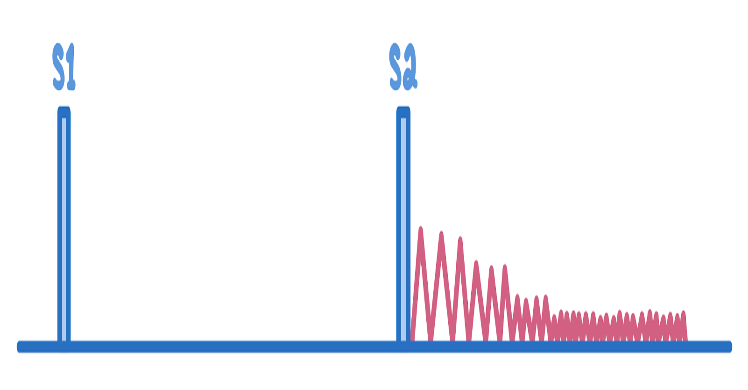
- Sustained hand grip
- Rapid squatting
- Passive leg raising
- Abrupt standing
SDL