Fluid & Electrolyte Disturbance
Dr. Faten Zaidan
Fluid Content According to Age
Total body water (TBW) varies with age:
- Preterm: 80-85%
- Term: 75%
- Infant: 65%
- Older children & adult male: 60%
- Adult female: 50%
After birth, term infants lose approximately 5%-15% of their body weight in the first week of life. TBW decreases to 60% by the first year of life. Females have less fluid content because of more fat cells.
Regulation of Body Fluids
Body fluid homeostasis is maintained through:
A. Fluid Intake
Controlled by the hypothalamus.
B. Hormonal Regulation
- Antidiuretic hormone (ADH/vasopressin): Increases reabsorption of water and causes vasoconstriction, leading to increased intravascular volume.
- Renin-Angiotensin-Aldosterone Mechanism
- Natriuretic Peptides: Shut down thirst center, inhibit renin secretion, and inhibit aldosterone, leading to sodium and water loss (mimicking diuresis). ANB + BNP > shut down thirst centre, inhibits renin secretion, inhibits aldosterone , leading to sodium and water loss (mimicking diuresis)
C. Fluid Output
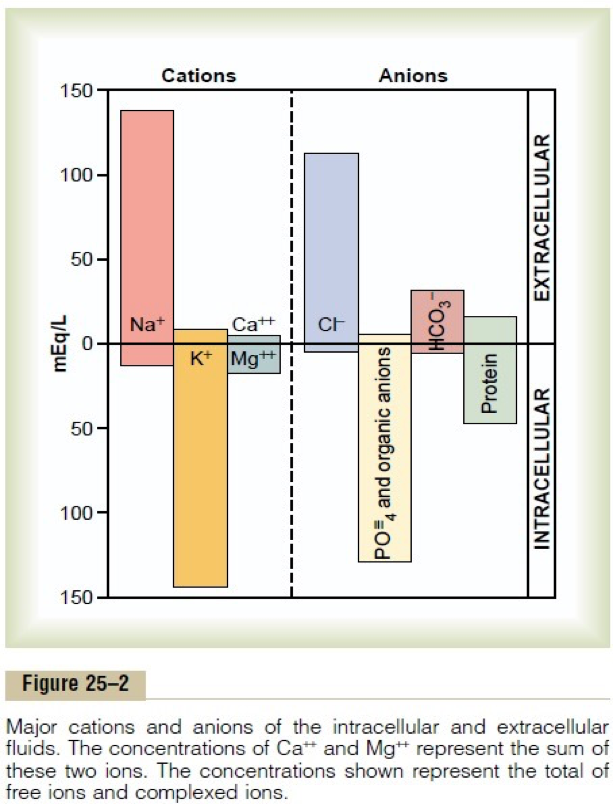
Electrolyte Distribution
Cations and Anions
- Extracellular Fluid: Main cation is Sodium (Na = 135 - 145 mEq/L), regulated by RAAS.
- Intracellular Fluid: Main cation is Potassium (K = 3.6 - 5.2 mmol/L), regulated by dietary intake and renal excretion.
Causes of Dehydration
- Most common: Gastroenteritis
- Other causes: Phototherapy, increased respiratory rate, fever, vomiting, drainage tubes, blood loss, burn.
Dehydration can be classified based on the degree of fluid loss:
- Mild: 5% in infants and 3% in children > 1 year
- Moderate: 10% in infants and 6% in children > 1 year
- Severe: 15% in infants and 9% in children > 1 year
Assessment of Dehydration Based on Clinical Signs
| Clinical Sign | Mild | Moderate | Severe |
|---|---|---|---|
| Skin turgor | Normal | Tenting | None |
| Skin (touch) | Normal | Dry | Clammy |
| Buccal mucosa/lips | Dry | Dry | Parched/cracked |
| Eyes | Normal | Deep set | Sunken |
| Tears | Present | Reduced | None |
| Fontanelle | Flat | Soft | Sunken |
| CNS | Consolable | Irritable | Lethargic/obtunded |
| Pulse rate | Normal | Slightly increased | Increased |
| Pulse quality | Normal | Weak | Feeble/impalpable |
| Capillary refill | Normal | ~2s | >3s |
| Urine output | Normal to decreased | Decreased | Anuric |
Early Detectable Signs
- Tachycardia
- Dry mucous membranes
- Cold peripheries
- Decreased urine
- Thirst
- Decreased activity
Laboratory Parameters
Hypoglycaemia is present in moderate to severe dehydration
- Increased plasma protein or albumin concentration
- Increased urine osmolality
- Elevated serum levels for sodium, creatinine, and urea as well as hematocrit
- Increased blood urea nitrogen/plasma creatinine ratio
- pH changes (metabolic alkalosis or acidosis)
- Increased plasma concentration of lactate
- Hypoglycemia is present in moderate to severe dehydration
Clinical Signs???? CC
- Hypotension, tachycardia, and reduced blood pressure amplitude
- Reduced jugular vein filling, reduced capillary refill
- Orthostatic signs (if bedridden in foot-down position)
- Dry skin and dry mucous membranes
- Pronounced skin wrinkles turgor
- Cold, possibly marbled extremities
- Increased secretion viscosity (saliva, sputum)
Approach to Dehydration
The general principle is to replace the deficit and ongoing losses and continue to provide maintenance fluid requirements.
-
In mild dehydration, initiate therapy with oral solutions.
-
If the patient shows clinical signs indicating moderate to severe dehydration, or oral therapy fails, intravenous therapy will be initiated.
-
Patients with hemodynamic instability characterized by severe dehydration, e.g., increased capillary refill time and low blood pressure, will need an initial fluid bolus with isotonic solutions, such as normal saline.
Oral Rehydration Therapy (ORT)
ORT is recommended as the initial therapy of choice (e.g., Pedialyte). It involves the frequent administration of small volumes on a regular schedule.
-
If the patient is performing ORT well, they can be discharged to continue fluid replacement at home.
-
Method: 10 mL of Pedialyte administered with a syringe over a 5-minute period is one method of ORT. The volume can be increased as tolerated, and the interval can be shortened.
-
Alternatively, give 50-100 mL/kg within 4 hours.
-
If the patient is experiencing emesis, Ondansetron may be used before oral intake.
ORT May Fail, Why?
- Patient refusal
- Parental noncompliance
- Persistent emesis
- Losses greater than the amount of fluid given
Therefore, we move into intravenous fluid therapy:
- Boluses should be made with isotonic fluids (normal saline or lactated Ringer).
- The bolus volume is 20 mL/kg.
Indications to Stop IVF Therapy and Encourage Oral Intake
- Normalizing vital signs
- Oral intake by the patient
- Resolving signs/symptoms of dehydration
- Discharge

Emergency Treatment
The presence of severe dehydration and shock requires aggressive fluid resuscitation.
- The clinician will initially give boluses of isotonic fluids, then provide maintenance.
- If there is no IV line secured, an intraosseous line should be inserted without hesitation.
- The maximum amount of fluid boluses allowed is 60 mL/kg.
- If there is hemorrhage or fluid boluses did not improve vital signs (decreased blood pressure, increased heart rate), blood products can be used to restore intravascular volume.
Considerations in Dehydration Management
- Boluses/Fluid deficit
- Maintenance
- Electrolyte (Sodium)
Fluid Calculations
-
Acute Resuscitation
- Normal Saline or Ringer Lactate 10-20 mL/kg boluses over 5-10 minutes in case of hypovolemia.
- In case of cardiogenic shock or distributive shock, fluids must be 5-10 mL/kg over 20 minutes.
-
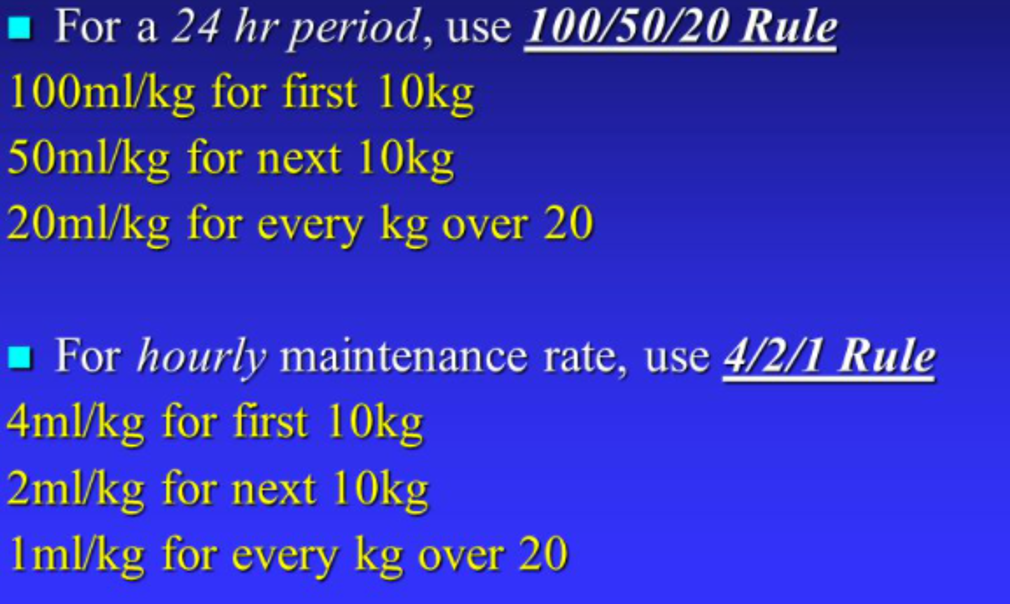
Calculate Maintenance Using the Holliday-Segar Rule.
-
Calculate Fluid Deficit
- Either calculate it through the decreased weight (not practical): pre-illness wt. (kg) − post-illness wt. (kg)
- Or calculate it through the percentage of dehydration present:
- 5% dehydration requires 50 mL/kg fluid replacement.
- 10% dehydration is 100 mL/kg.
-
Subtract Fluid Boluses Given in Resuscitation Phase from Fluid Deficit
-
Calculate Replacement Over 24 Hours
- First 8 hours: 50% Deficit + Maintenance
- Next 16 hours: 50% Deficit + Maintenance
-
Determine Sodium Concentration
- Hypernatremic dehydration (Na > 145)
- Hyponatremic dehydration (Na < 135)
- Isotonic dehydration (Na = 135-145)
-
Add Potassium Chloride to IVF After Patient Passes Urine
bolus 15-20 ml/kg 5-10 minutes
5-10ml /kg 20-30 minutes
Maximum amount 60 ml/kg for children Maintenance amount - 4. 100 - 2. 50 - 1. 20 per h. per 24h
Fluid deficit 50 ml/kg
100ml/kg
ex Q&A 6 yr child diarhea 3d ays polyugria dry mucus membrane palpaitation, moderate sevirity - given 2 bolus two kg… - substract
35 kg child given one bolus 20 ml/kg with moderate case
700 ml
moderate 100 X 35 = 3500 maintenance per 24hr = 100x 10 = 1000 50x10 = 500 20x15 =300 = 1800 + 3500 = 4300
Holliday-Segar Rule
Example
For a 35 kg, 11-year-old boy:
- 10 * 4 = 40
- 10 * 2 = 20
- 15 * 1 = 15
Total: 75 mL/kg/hr
75 * 24 = 1800 mL/day