IM
HEPATITIS C
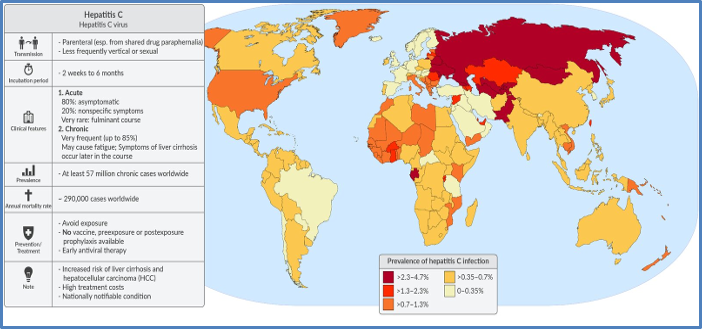
Epidemiology
- Occurs worldwide but very common in Africa and Egypt.
- Prevalence in KSA: 1%
Mode of Spread (Parenteral)
- IV drug use (West)
- Blood transfusion (developing countries)
- Contaminated needles and instruments (surgical, dental)
- Sexual transmission is very low (<1%)
- Perinatal transmission: <1%
- Contact with infected blood (razors, cuts)
Subtypes There are 7 subtypes of Hep C (1 to 7).
What Happens After Infection
- Few patients (10-20%): Develop mild acute hepatitis that resolves, and the infection clears.
- Most patients: Develop chronic hepatitis.
Chronic Hepatitis C
- Usually asymptomatic and detected by chance on routine blood tests (slightly high AST & ALT). LFTs often fluctuate.
- Often presents as cirrhosis after many years.
- Mild jaundice and fatigue may occur.
Diagnosis (Hepatitis C)
- Hep C antibody (Anti-HCV Ab):
- Initial screening test.
- Can be detected in the blood about 2 months after infection.
- This antibody is NOT protective (opposite of Hep B).
- Hep C RNA levels (by PCR):
- Measures the actual virus level in the blood.
- Can be detected in blood after 1-2 weeks of infection (earlier than the antibody).
- Liver Biopsy: Not done routinely for diagnosis, only before treatment to assess disease severity.
Treatment (Hepatitis C)
- Offered to most patients.
- Response to treatment depends on the genotype (1 to 7) and other factors (type 2 and type 3 Hep C have a very good response to treatment).
- Latest treatments are mainly oral drugs. Sometimes interferon can be added.
Drugs Used in Hepatitis C Treatment
- Ribavirin: Used in combination with other drugs to avoid resistance
- Direct-acting antivirals (DAAs):
- Ledipasvir
- Simeprevir
- Sofosbuvir
- Interferon: Sometimes added to the above.
Treatment duration is generally 3 months.
Other Aspects of Management (Hepatitis C)
- Patient Counseling:
- Do not donate blood or tissue.
- No IV drugs, no needle/razor sharing.
- Explain the small risk of sexual transmission.
- Avoid alcohol (can worsen the disease).
- Check for Hep B & Hep A and vaccinate if negative.
- Check for HIV.
Vaccine (Hepatitis C)
No vaccine or immunoglobulins are available yet.
Outcome (Hepatitis C)
Without treatment, Hep C can lead to cirrhosis and hepatocellular carcinoma (liver cancer).
Pregnancy and Breastfeeding in Hepatitis C
- Hep C in the female does not have any adverse effects on pregnancy.
- 1-2% chance of perinatal transmission.
- Breastfeeding is safe, but if the nipples are cracked or bleeding, do not breastfeed.
Rapid Fire Questions (Hepatitis C & E)
- Mode of transmission of Hep C? parental
- Is sexual & perinatal transmission very common like Hep B? no
- After Hep C infection, most patients develop acute or chronic hepatitis? chronic
- Which 2 diagnostic tests are used for Hep C? *anti, pcr *
- Which one will you do first as a screening test? antibody
- Are the LFTs always very high? little high, fluctuate
- A person gets infected with Hep C today. Which test will be positive first? PCR in 2wk then antibodies
- Anti-HBc antibody can kill the virus, true or false? false
- Name some drugs for Hep C treatment. RASUL + Interferon
- In a patient with chronic Hep C, which 2 vaccines should you give? no vaccines which you give?
- If a patient gets infected with Hep C today, you can give immunoglobulins for treatment, true or false? False
- What is the effect of Hep C on pregnancy? minuscule risk
- How to counsel a Hep C lady about breastfeeding?
- Hep E is more common in pregnant ladies, true or false?
- Mode of transmission of Hep E?
- Effects of Hep E on pregnancy?
Thera
Infection persists because the production rate of new mutant virions exceeds the production rate of host antibodies.
UpToDate: vertical transmission or during birth (mode of delivery does not affect the incidence). (in 5-15%)
Breast feeding does not transmit the virus.
WHO: HCV can also be transmitted sexually and can be passed from an infected mother to her baby; however these modes of transmission are much less common. Higher in MSM; anal sex.
Prior infection with HCV does not protect against later infection with the same or different genotypes of the virus.
Clinical Features:
Acute Infection:
- Asymptomatic in 80% of cases
- Symptomatic (20%): Malaise, fever, myalgias, arthralgias, RUQ pain, tender hepatomegaly, nausea, vomiting, jaundice, pruritus.
Chronic hepatitis:
- (up to 85%)
- Liver cirrhosis (25%) within 20 years of infection.
- Extrahepatic features of HCV (common):
- Hematological: Mixed cryoglobulinemia, lymphoma (especially B-cell lymphoma)
- Glomerulonephritis
- Sjogren Syndrome (Sicca syndrome).
Transfusion risk after PCR is less than 1 per 2 million units transfused. The newer assays have decreased the window after infection to 1-2 weeks. Needle-stick injuries in the healthcare setting result in a 3% risk of HCV transmission.
Monoclonal IgM and polyclonal IgG antibodies or polyclonal IgM and polyclonal IgG antibodies. In vivo, these cryoglobulins form immune complexes→ vasculitis. In vitro, these cryoglobulins precipitate slowly on cooling. Mixed cryoglobulinemia is associated with infections (especially hepatitis C), and autoimmune diseases (especially Sjogren's disease and SLE).
Symptoms of dry eyes or dry mouth, otherwise known as sicca symptoms, are not always present in patients with Sjögren's syndrome.
Diagnosis of HCV:
- Anti-HCV antibodies.
- HCV RNA by rt-PCR.
Treatment:
- Combination therapy of:
- Direct-acting antivirals or
- Interferon PLUS ribavirin
Prevention:
No available vaccine.
Self-limited in 15-50%.
SVR: The absence of hepatitis C virus RNA after 12 weeks of therapy with direct-acting antivirals. A patient in this state is considered to be cured of hepatitis C virus infection.
Recurrence after liver transplant is universal.
HCV patient can donate their liver and other oragns even to those who are HCV negative
New drugs; Direct-Acting Antiviral Agents: protease inhibitors, polymerase inhibitors
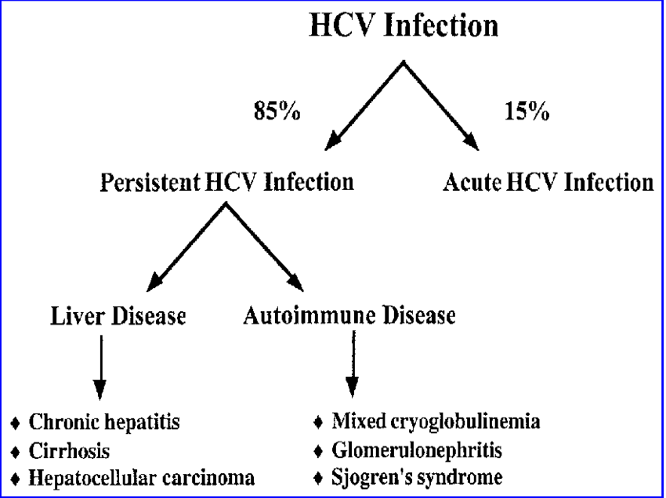
•Risk factors for chronic disease: Being male, Being age >50 years, Consuming alcohol, fatty liver disease, hepatitis B, or HIV coinfection, Receiving immunosuppressive therapy
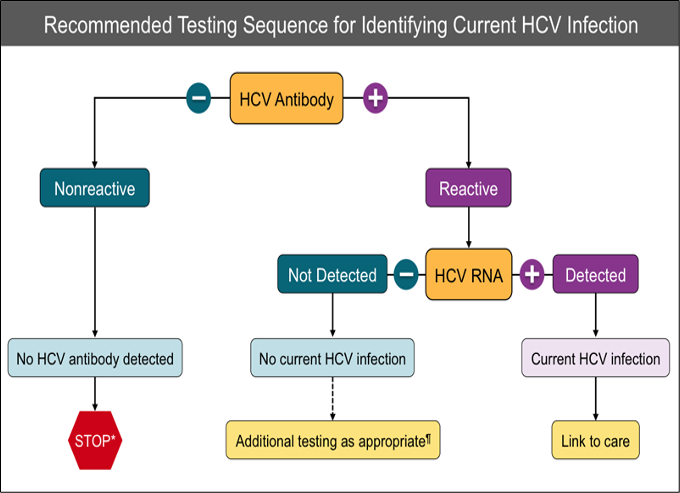 For persons who might have been exposed to HCV within the past 6 months, testing for HCV RNA or follow-up testing for HCV antibody is recommended. For persons who are immunocompromised, testing for HCV RNA can be considered.
For persons who might have been exposed to HCV within the past 6 months, testing for HCV RNA or follow-up testing for HCV antibody is recommended. For persons who are immunocompromised, testing for HCV RNA can be considered.