Case Studies
Patient Brief Record / Brief Scenario
Information for Student about the Case
- Patient Name: Mohammad
- Age: 40 years
- Occupation: Car Mechanic at Om Al-Hamam Workshop Centre
- Not known to have any chronic illness
- Today:
- BP: 120/80 mm Hg
- Temperature: 37 °C
Mr. Mohammad is a 40-year-old, presented today with the complaint of low back pain.
Tasks (What is expected from a student?)
- Take a focused history from this patient to arrive at the most likely diagnosis.
- Perform the relevant clinical examination.
- Inform the patient about the diagnosis.
- Manage the patient appropriately.
- Explain to the patient the management plan.
Patient Brief Record / Brief Scenario
Information for the Simulated Patient
- Patient Name: Mohammad
- Age: 40 years
- Occupation: Car Mechanic at Om Hamam Workshop
- Married, with 2 children (10 and 5 years old).
Opening Scenario
I have severe low back pain this afternoon (You will admit only this).
Tell your doctor about the following information only if specifically asked about:
- You have experienced low back pain when you were holding some heavy object in your workshop. The pain appeared sudden, very sharp, and severe.
- You just sat down, pain gradually reduced, but still pain is there, but not severe as before.
- You have taken Brufen (the red tablet) which reduced the pain but caused a severe burning sensation in the stomach. You took it from your friend, on an empty stomach.
- You are a smoker (20-30 cigarettes per day).
- No chronic problems in the past.
- You have a very stable family life.
- Your idea: it could be disc prolapse.
- Your concern: that you could not return to work, as you have to take bed rest for one to two weeks. This will affect your income.
- Your expectations are:
- That your doctor will do an X-ray to find out if it is disc prolapse.
- A strong injection to relieve the pain.
- Referral to the Orthopaedic clinic.
Ask your doctor about:
- An X-ray, insist if he refuses as you want to find out if it is disc prolapse, and referral to the Orthopaedic clinic.
- If he convinces you about it in an appropriate way, agree with him.
The doctor will examine your back by exposing it. Ask you to do different movements at the back and other joints. You will act naturally. If the doctor asks you to bend forward or backward, you will say: “AHH, there is pain at the lower back above your buttock.”
Candidate Should Cover the Following
Introduction
- Introduce yourself
- Confirm the patient’s details
- Ensure privacy and take consent
- Explain the purpose of examination
- Proper exposure: the entire back including sacral area (if appropriate)
- Body Position: Standing/sitting
- Hand washing (before and after examination)
History
- Onset, duration, timing, character, Localization, radiation, Frequency, Precipitating factors and relieving factors, Associated symptoms:
- Lower limbs numbness or parasthesia
- Urinary and/or stool incontinence/saddle anesthesia
- Functional limitations
- Red flag: fever, unexplained weight loss
- History of trauma, Heavy lifting
- Past medical history: prior cancer diagnosis, history of osteoporosis, DM, TB, or HIV.
- Drug history/allergies: prolonged corticosteroid, IV drug abuse
- Past surgical history
- Family history
- Occupational history
- Psychosocial and lifestyle history (stress, Depression, sedentary lifestyle, smoking)
Examination
General Examination Principles
- Permission
- Explain
- Privacy
Preparation & Vitals
- Patient should be standing (or sitting) with the whole trunk exposed.
- Take Vital Signs.
- Note General appearance, BMI.
Examination Steps Overview
- Look ➔ Feel ➔ Movement ➔ Neurologic tests
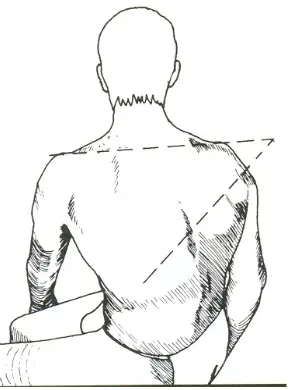
1. Inspection
- Gait
- Posture:
- Assess for scoliosis, Kyphosis, or lordosis.
- Check head/shoulders alignment, listing, flexion/extension posture, pelvic tilt.
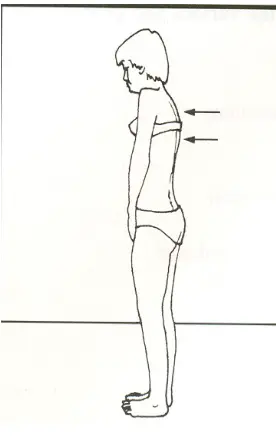
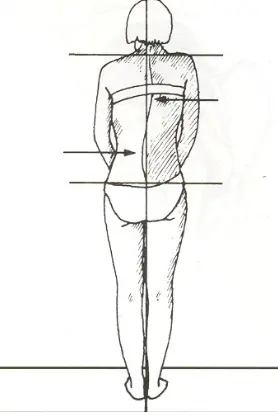
- Symmetry
- Skin: Look for swelling, scars, fat pads, erythema.
- Muscle: Note muscle balance, habitus, and any wasting.
- Alignment
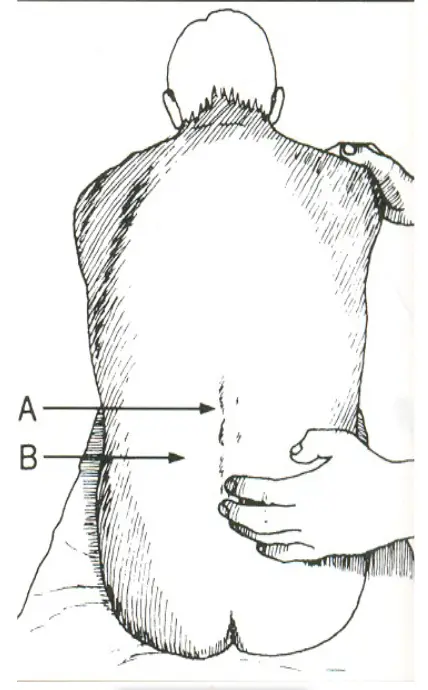
2. Palpation and Percussion
- Temperature
- Tenderness:
- Over spinous processes (Bone)
- Paraspinal muscles, paravertebral area (Muscles - check for tension and trigger points)
- Facet and sacroiliac joints (Joints)
- Coccygeal tip
- Anterior and posterior iliac spine
- Deformity: Over spinous processes.
- Masses
3. Range of Motion (Movement)
- Often very limited globally secondary to pain.
- Perform slowly with physical support if needed.
- Flexion (normal = 90 degrees)
- Extension (normal = 30 degrees)
- Narrows canal, loads facet joints
- Lateral Bending (normal = 45 degrees, hand to knee)
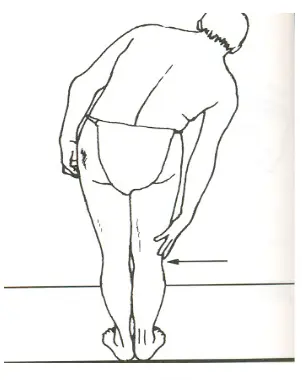
- Rotation / Twisting (normal = 90 degrees, stabilize hips)
4. Neurologic Examination
-
Focus on the L5 and S1 nerve roots (98% of disc herniation occurs at L4-5 and L5-S1).
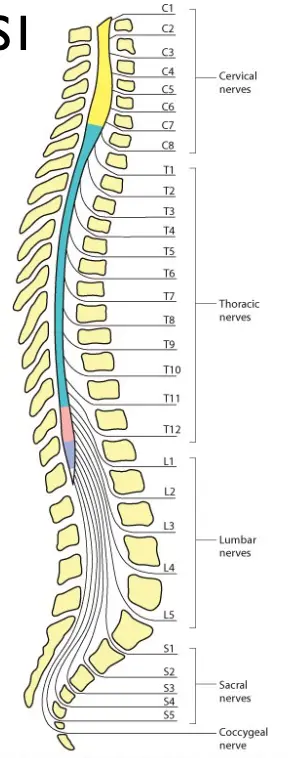
-
Reflexes:
- Knee reflex (L3-4 / L4)

- Ankle reflex (S1-2 / S1)

- Hamstrings reflex (L5)
- Knee reflex (L3-4 / L4)
-
Motor Testing / Power:
- Ankle dorsiflexion / Resisted Foot dorsiflexion (L4)

- Resisted Big toe dorsiflexion (L5)
- Ankle plantar flexion / Resisted plantar flexion (S1)

- Walking on heels (L4/L5)

- Walking on toes (S1)

- Ankle dorsiflexion / Resisted Foot dorsiflexion (L4)
-
Sensory Testing:
- Assess distribution of the sciatic nerve (L4, L5, S1, S2).

- Specific areas:
- Medial side of foot (L4)
- Dorsum of the foot (L5)
- Lateral side of the foot (S1)
- Assess distribution of the sciatic nerve (L4, L5, S1, S2).
-
5. Vascular Examination
- Check pulses.
- Check capillary refill.
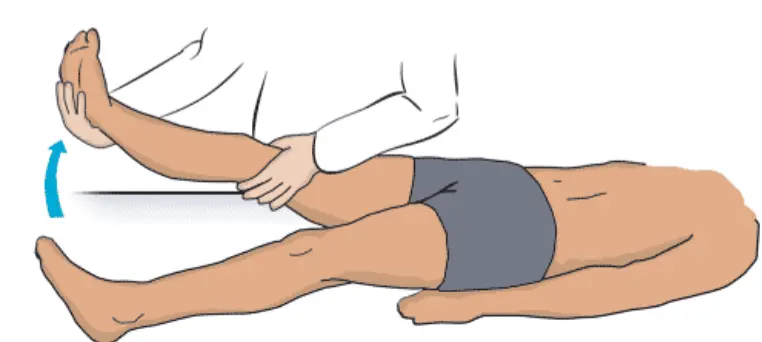
Special Tests Y
-
Straight Leg Raising (SLR) / Lasègue’s Test:
- Performed by lifting the patient’s extended leg with the ankle dorsiflexed, in the sitting (or supine) position.
- Normally 80 – 90 degrees with no pain.
- Pain radiating past the knee suggests sciatica. Limited by sciatica pain in lumbar disc prolapse (typically positive if pain occurs at <70 degrees, specifically between 30 to 70 degrees).
- Dorsiflexion of the ankle during the test increases sciatic tension and pain.
- Plantar flexion relieves sciatic tension and pain.
- Video: Straight Leg Raise or Lasègue’s Test for Lumbar Radiculopathy.mp4
-
Crossed Straight Leg Raising Test:
- Performed by doing a straight-leg raise test on the opposite (uninvolved leg).
- If this maneuver aggravates the sciatica pain in the affected leg, it is highly suggestive of sciatica.
-
Bragard Test:
- A straight leg raising is done; if positive, the leg is lowered just below the point of pain and then the ankle is dorsiflexed. Increased pain is further indicative of nerve compression.
-
FABER Test (Patrick’s Test):
- Performed by placing the hip and leg into the figure-4 position (Flexion, ABduction and External Rotation).
- This will aggravate sacroiliac joint pain.
-
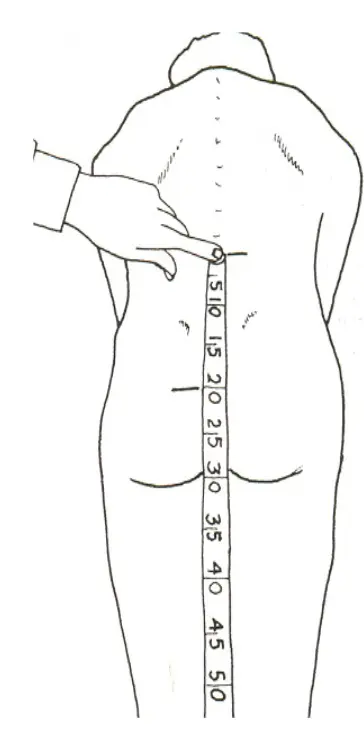
Modified Schober’s Test:
- With the patient in upright position, use a pin marker to determine the level of sacral dimples (approximates 5th lumbar spinous process).
- Draw two more marks: 10 cm above and 5 cm below the first mark (total distance 15 cm).
- Ask the patient to bend forward maximally and measure the distance between the top and bottom marks.
- Normally, the distance will increase from 15 cm to at least 20 cm with lumbar flexion.
- A difference of < 5 cm raises suspicion of Ankylosing Spondylitis.
- Reference Video: www.youtube.com/watch?v=QlExWyRBubE
Investigation
- CBC, ESR, CRP: if suspected infection or malignancy.
- X-ray: if suspected cancer, vertebral compression fracture, or ankylosing spondylitis.
- MRI or CT: if severe or progressive neurologic deficits, suspected cauda equina syndrome, or vertebral infection.
Management
- Education and advice
- Behavior therapy, exercise therapy
- Analgesia: Acetaminophen or (NSAID) and muscle relaxant.
- Consider referral to physiotherapy if indicated.
- Arrange follow-up.
- Consider referral if red flag symptoms are present.
Doctor/Patient Interaction / Effective Use of Consultation
-
Understanding the patient’s perspective: Ideas, Concerns, and Expectations.
-
Non-verbal behavior: eye contact, posture and position, movement and expression.
-
Demonstrates interest, concern, respect for the patient as a person (throughout the interview).
-
Encourages patient to talk.
-
Uses open-ended questions and closed questions as appropriate.
-
Listening: listens attentively, allowing patient to complete statements without interruption and leaving space for patient to think.
-
Facilitation: facilitates patient’s responses verbally and non-verbally e.g. use of encouragement, silence etc.
-
Internal summary: periodically summarizes to verify own understanding of what the patient has said; invites patient to correct interpretation or provide further information.
-
Uses concise, easily understood questions and comments, avoids or adequately explains jargon.
-
Promote informed decision making and attends to timing.
-
Back Examination Video: www.youtube.com/watch?v=DTXi1zI154