Assess
- Review physician’s order and understand purpose of inserting catheter
- Assess client (last urination, level of awareness, understanding)
- Palpate bladder
- Identify meatus and assess skin integrity
- Identify potential difficulties (i.e enlarged prostate)
Implement
- Wash hands thoroughly before and after insertion
- Provide privacy
- Raise bed, stand on left side of bed if right handed (right side if left handed)
- Arrange equipment
- Water proof pad under client
- Position & drape client
- Use smallest catheter possible to help prevent trauma
- Female: dorsal recumbent (supine with knees flexed) or Frog-leg position (hips externally rotated slightly flexed, and knees bent) or lithotomy position.
- Male: supine position
- With disposable gloves, wash perineal areas
- Wash hands
- Open tubing with collection bag (attach to bed frame and
- have tubing positioned to easily connect to catheter once inserted
- organize sterile field – add catheter, lubricant, syringe and sterile water, test balloon, pour cleaning solution over cotton balls
- Apply sterile gloves
- Lubricate catheter (2.5 to 5 cm for women) and 12.5 to 17.5 cm for men)
Note: there may be an order for lubricant containing local anaesthetic
Apply sterile drapes keep gloves sterile - women: under buttocks and fenestrated over perineum - men: over thighs and fenestrated over penis
-
Place sterile tray and contents between legs
-
Cleanse meatus:
-
Women: with nondominant hand, expose meatus, maintain Position of hand, cleanse with forceps, wipe from front to back, new cotton ball each swipe, far labial fold, near, and directly over meatus
-
Men: retract foreskin, hold penis below glans, maintain position of hand, with forceps clean in a circular motion from meatus down to base of glans, repeat three more times
-
Hold end of catheter loosely coiled in dominant hand, place end of catheter in tray
-
Insert catheter:
-
Women: insert 5 to 7.5 cm until urine flows, then advance another 2.5 to 5 cm
-
Men: hold penis perpendicular, catheter to the hilt (bifurcation)
-
Collect specimen if indicated
-
Allow bladder to empty unless policy restricts
-
Inflate balloon with amount indicated
-
If client complains of pain, aspirate solution and advance catheter further and inflate
-
Gently pull to feel resistance
-
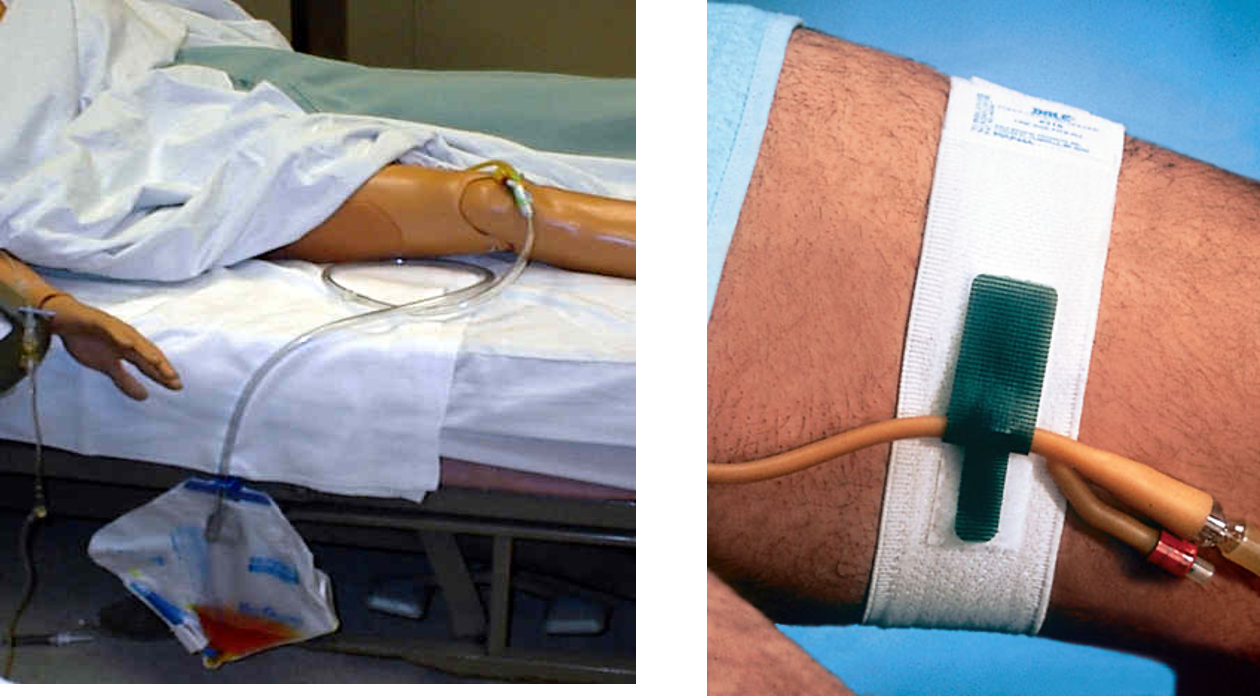
Attach catheter to collection bag and attach to bed frame below bladder
-
Anchor catheter (thigh if appropriate and coil tubing on bed and attach to mattress)
Evaluate
- Palpate bladder
- Assess comfort
- Characteristics and amount of urine
CATHETER MAINTENANCE
- Assess need for Foley daily
- Daily AM Care: Cleanse around catheter and meatus with soap and water daily and Limiting manipulation of the catheter reduces infection.
- Secure the catheter with a leg band: Leg bands help keep the catheter in place and decrease pulling and twisting.
- Avoid bladder irrigation unless obstruction has occurred.
- Keep Drainage Bag BELOW the Bladder: This prevents reflux back into the bladder, which can increase infection
- Keep Drainage bag OFF the Floor: To avoid contaminating the spout.
- Use individual graduated container for EACH Patient/label with name
- EMPTY the drainage bag before transport to avoid reflux
- Maintain a Closed System: -Take urine samples through the port -Always scrub the hub first before taking a sample
REVIEW AND REMOVE
-
“The duration of catheterization is the most important risk factor for development of infection.”
-
The necessity of a bladder catheter should be addressed by physicians daily as a part of rounds, and by nursing as part of their assessment.
Changing the catheter
-
Indwelling catheters as a rule should not be replaced routinely; they should not be changed if flow appears.
-
Changing an indwelling catheter at routine, fixed intervals is not recommended, and there is insufficient evidence to make a recommendation on long-term catheters ,However, catheters with mechanical problems (poor drainage, encrusted) need to be replaced.
Criteria for Removal
-
The patient is awake, alert and oriented and/or can verbally express that they had no trouble voiding before the catheter was placed.
-
Patient is able to resume their normal voiding position, or at least one that is presently comfortable.
-
If a Foley is present post invasive cardiac or radiological procedure, confer with physician to remove Foley unless there is a clear reason for not discontinuing the Foley.
-
Epidural catheter is removed.
In Males
- Greet patient, explain full procedure, take confirmation, nurse
- before starting make sure everything is prepared
-
- Open instrument and make it ready for use
-
- ready the catheter - bifidone - saline - gin
- Supine for males.
- Wear sterile gloves
- Apply Drape
- Non dominant hand will hold the skin, labia/penis
- Retract skin,
- after cleansing, inject lidocaine intro penile urethra
- Take cotton with bifidone then clean meatus, scrotum in circular motion, not return to same area - take another one with same motion - discard the cotton
- Keep holding with you non-dominant hand
- then inject lidocaine gel lubricant in urethra
- with your right hand, hold folly’s catheter then pull from non-dominant whilist holding penis.
- you can add extra lidocaine to catheter; Then insert with nondominant hand keeping it completely straight, then push catheter all the way until end - in females until urine flows
- Then drop your non domininant hand
- Inflate balloon, then pull catheter to hold it in place, then connect the bag.
- We keep bag below patient
In Females
- non dominant hand to hold
- then use cotton with your right hand to clean around and inside the labia
- If it goes inside vagina, then throw it out and change the catheter
- 5-7 cm insertion - then when you see urine come out - push it more 2 cm then inflate the balloon
- attach by side of thigh
- keeping the bag below the patient, by the side of the bed