WIPER
Exposure | position | privacy | Ask for vitals
- W ash hands (before and after)
- I ntroduce yourself to the patient and seek his or her consent
- P osition the patient correctly.
- E xpose the patient as needed (e.g. ‘Please take off your shirt for me now, if that is all right’)
- R ight side of the bed
- Vital sign & Growth parameter
General Appearance
ABCDEFG
General Exam
Hands
- finger clubbing
- palmar erythema (hypothenar for liver)
- Sweating
- Pallow
- Flapping tremors
- Capilarry refill
- Volume/Rate pulse
Face
- Dysmorphic
- Pallor
- central cyanosis
- nasal polyps
Growth Parameters
Pallor
Pericordium
- Deformoties
- Scars
LNS
Lower limbs
Back
Focused Examination
inspection and ausculation done to <2 years - ask instructor if to do palpation percussion
Inspection
- Deformity
- Scars
- Asymmetry/movement
- respiratory distress - accessory muscles
- Strenocleidomastoid
- Scalene
- Pectoralis major and minor
- Trapezius
- Abdominal muscles
- Cautery marks suggest previous illness
Auscultation
start with auscultation immediately after inspections] Zig zag method front and back.
1- Comment on Air Entry
Reduced in lung diseases, pulmonary collapse, pneumothorax
2- Comment on Breath sound
Bronchial:
Heard over the trachea and mainstay bronchi (2nd-4th intercostal spaces either side of the sternum anteriorly and 3rd-6th intercostal spaces along the vertebrae posteriorly). The sounds are described as tubular and harsh. Also known as tracheal breath sounds. 2nd / 3rd intercostal normal continuous
Broncho-vesicular:
Heard over the major bronchi below the clavicles in the upper of the chest anteriorly. Broncho- vesicular sounds heard over the peripheral lung denote pathology. The sounds are described as medium-pitched and continuous throughout inspiration and expiration. Inspiratory high pitch = Low pitch Expiration
Vesicular:
Heard over the peripheral lung. Described as soft and low- pitched. Best heard on inspiration. inspiration long, expiration short
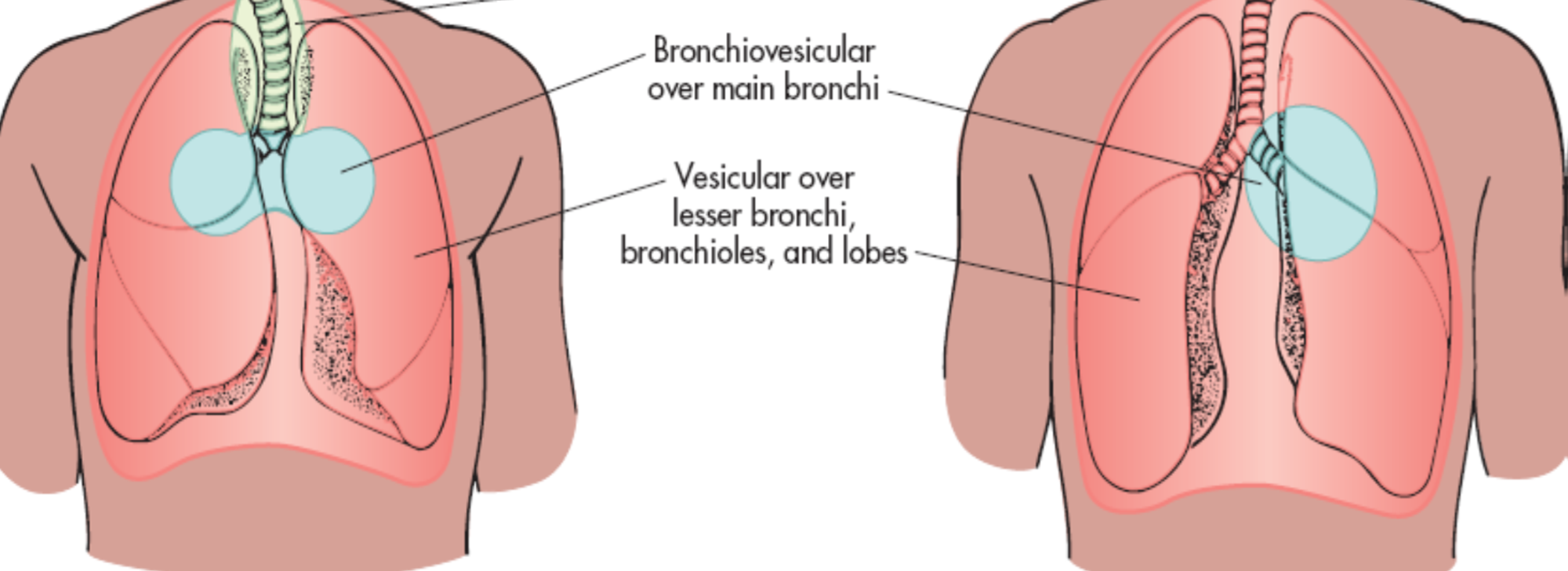
Diminished:
Heard with shallow breathing; normal in obese patients with excessive adipose tissue and during pregnancy. Can also indicate an obstructed airway, partial or total lung collapse, or chronic lung disease.
Abnormal bronchial breath sound (tubular breath sound)
Bronchial breath sound appears in supposed vesicular breath sound area where expiration inspiration are mostly equal
- Consolidation: lobar pneumonia (consolidation stage)
- Large cavity: TB, lung abscess
- Compressed atelectasis: hydrothorax, pneumothorax
Added Sounds
- Stridor - Wheezes: are continuous musical polyphonic sound, heard louder on expiration & can be heard on inspiration which may imply severe airway narrowing. It indicates airway obstruction. - Comment Is the wheezing biphasic or only expiratory. If biphasic it’s a warning sign and makes us concern - Ronchi
- Crackles: interrupted non-musical inspiratory sound - Crackles may be early, late or pan-inspiratory. - Fine, coarse or medium.
- Pleural Friction Rub
Fine fermentation suggest pneumonia in the left side, you can hear crackles without stethoscope from the patient’s nose and this is the transmitted sound not the real one, the real sound heard by stethoscope
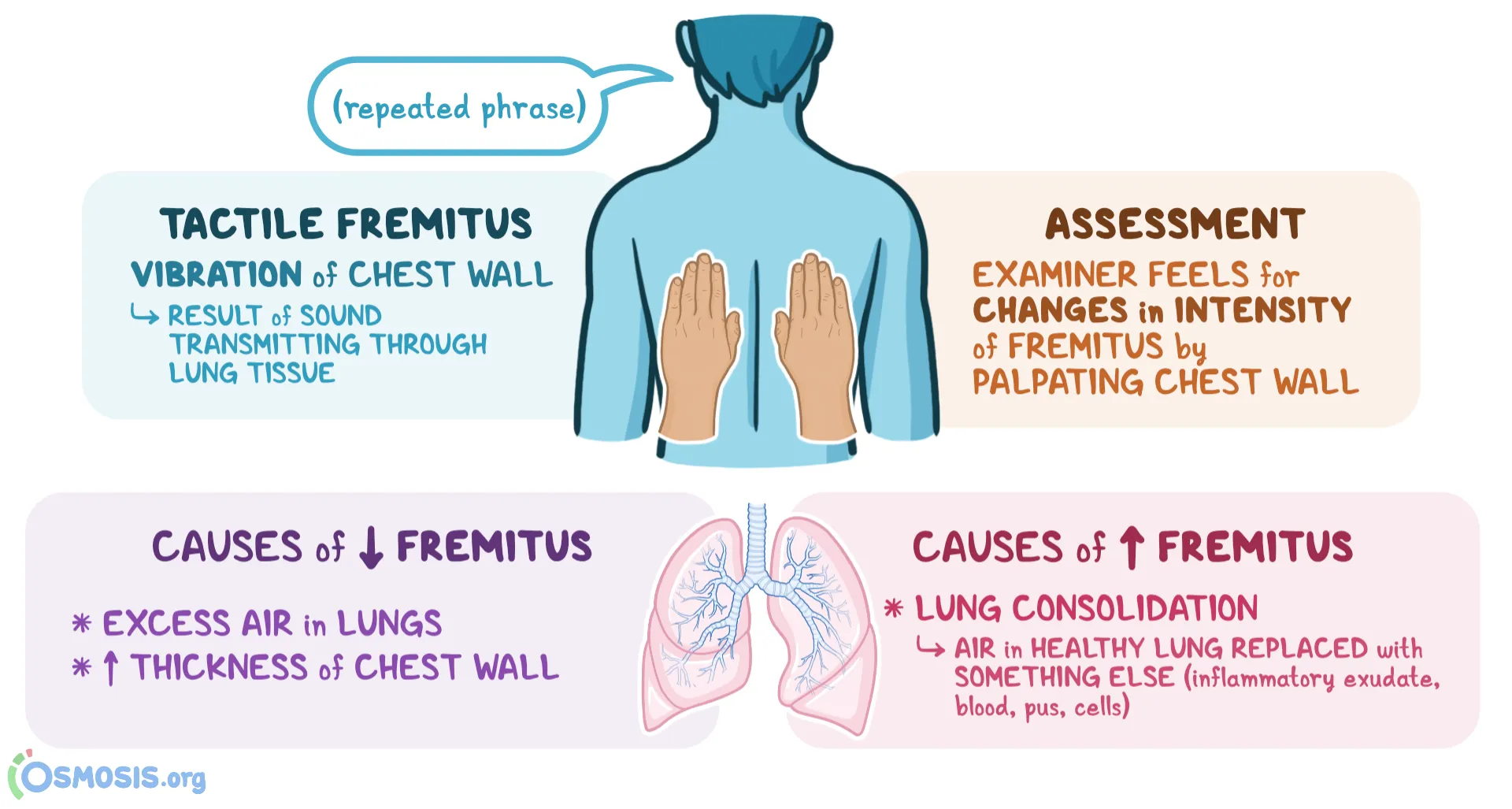
3- Comment Vocal resonance
It’s the ability to transmit sounds.
Ask patients to say 44 (Arabic) or 99 (English)
Bronchophony Consolidation
Pectoriloqny Massive consolidation
Egophony Upper area of hydrothorax
Palpation
press, and compress to midline to check equality of finger movement.
Anterior & Posterior
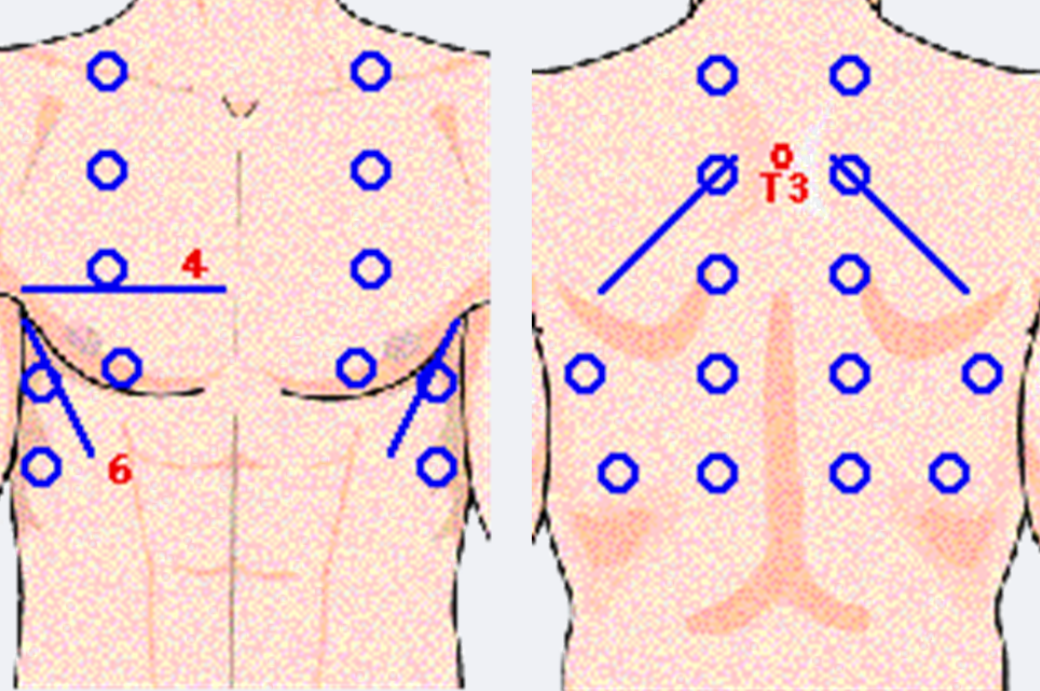
- Tactile Fremitus - three regions on front and back
- chest movement/Expansion - three regions on front and back
- Tracheal deviation
- Apex Beat
Percussion
tell patient to hug himself for scapular, and raise above head for axillary areas
Zigzag - same areas for auscultation
-
Anterior
-
Posterior
-
hyper ressonance - pneumothorax | Emphysema
-
normal - ressonance
-
Dullness - pneumonia | atelectasis
-
Stony Dullness - Pleural effusion
-
Tympany: Cavity or pneumothorax
Differential
Okay, here’s a table summarizing the requested information for pleural effusion, pneumothorax, cystic fibrosis, and bronchiectasis:
| Condition | Type of Lung Sound | Clinical Examination Findings | Most Common Site | Vocal Resonance | Airway Entry | Tactile Fremitus | Other Features |
|---|---|---|---|---|---|---|---|
| Pleural Effusion | Decreased or absent breath sounds over the effusion | Dullness to percussion, reduced chest expansion on the affected side | Dependent areas (e.g., lung bases) | Decreased | Decreased | Decreased | May have pleuritic chest pain, dyspnea; Large effusions can cause tracheal deviation away from the affected side |
| Pneumothorax | Decreased or absent breath sounds over the pneumothorax | Hyperresonance to percussion, reduced chest expansion on affected side, possible tracheal deviation away from affected side in tension pneumothorax. | Apical (if due to bleb rupture) | Decreased | Decreased | Decreased | Sudden onset of sharp chest pain, dyspnea, tachycardia. Tension pneumothorax is a medical emergency |
| Cystic Fibrosis | Crackles (rales), wheezes, rhonchi | Increased AP chest diameter, clubbing, use of accessory muscles | Widespread, but upper lobes often more severely affected | Variable | Variable | Variable | Chronic productive cough, recurrent infections, malabsorption, pancreatic insufficiency, salty sweat |
| Bronchiectasis | Coarse crackles (rales), rhonchi, wheezes | Chronic productive cough with large volumes of purulent sputum, clubbing, dyspnea | Lower lobes are commonly affected | Increased | Normal or decreased | Increased | Hemoptysis, recurrent infections, foul-smelling sputum, “tram-track” and “signet ring” signs on CT |
Normal sounds
Added Sounds
- Diminished - Stridor - Wheezes: are continuous musical polyphonic sound, heard louder on expiration & can be heard on inspiration which may imply severe airway narrowing. It indicates airway obstruction. - Ronchi
- Crackles: interrupted non-musical inspiratory sound - Crackles may be early, late or pan-inspiratory. - Fine, coarse or medium.
- Pleural Friction Rub
Investigations
Pleural Effusion
- Chest X-ray: To identify fluid accumulation in the pleural space.
- Ultrasound: To guide thoracentesis and assess the amount of fluid.
- CT Scan: Provides detailed images to help identify the cause.
- Thoracentesis: Fluid analysis for protein, LDH, cell count, and microbiology to differentiate between transudative and exudative effusions.
- Pleural Biopsy: If malignancy or tuberculosis is suspected.
Clubbing
- Chest X-ray or CT Scan: To check for lung diseases such as lung cancer or interstitial lung disease.
- Echocardiogram: To evaluate for congenital heart disease or endocarditis.
- Blood Tests: To assess for liver disease or inflammatory bowel disease.
- Pulmonary Function Tests: To evaluate lung function if respiratory causes are suspected.
Nasal Polyps
- Nasal Endoscopy: Direct visualization of the nasal passages and sinuses.
- CT Scan of Sinuses: To assess the extent of polyps and sinus involvement.
- Allergy Testing: To identify potential allergic triggers.
- Biopsy: Rarely needed, but may be performed to rule out other conditions.
Cystic Fibrosis
- Sweat Chloride Test: The gold standard for diagnosis, measuring the concentration of chloride in sweat.
- Genetic Testing: To identify mutations in the CFTR gene.
- Pulmonary Function Tests: To assess lung function.
- Sputum Culture: To identify bacterial infections in the lungs.
- Chest X-ray or CT Scan: To evaluate lung damage.
Immunodeficiencies
- Complete Blood Count (CBC): To assess white blood cell counts.
- Immunoglobulin Levels: Measurement of IgG, IgA, IgM to identify deficiencies.
- Flow Cytometry: To evaluate lymphocyte subsets and function.
- Genetic Testing: For specific known genetic immunodeficiencies.
- Vaccine Response Tests: To assess the immune system’s response to vaccines.
History
Consangunity Siblings with same diseases failing to thrive (growth parameters)
nasal polyps Any diarrhea - how frequent.., foul smelling..
Recurrent infections - is he taking antibiotics?
common presentation bronchial asthma cystic fibrosis immune deficiencies bronchistas…
Respiratory distress
compensatory mechanism for hypoxia should be discovered early to save life, in prevention of cardiopulmonary arrest.
common cause in children is respiratory arrest, wheas in adults for cardiovascular arrest.
Grading
-
mild
-
moderate
-
severe
-
upper part - acute laryngothyacitis - croupp (connected just to the vocal cold)
-
Lower - Bronchitis, Asthma -
-
lung tissue diseasse
-
Local - Pneumonia, intistial lung diseases, tension pnneumothorax -
-
obstructive lung disease
ABC
- A- Airway - can talk?
- B- Breathing - RR, O2, Air entry bilateral; lung sounds, consillidartion, resonance. - needle compressed in 2ics for pneumothorax - abdominal breathing?, use of accessory muscles
- C- Circulation - HR, RR, BP, Capillary refill, pulses (central/peripheral) - pinkish
- D- GCS - Dextrose
- E- Exposure
10l oxygen, face mask respiratory distress in impending respiratory failure.
Paediatric Assessment Triangle (PAT)
Appearance
- Alert / Verbal / Pain / Unresponsive (AVPU): Does the child require stimulation to garner a response?
- Flat, poor/rigid muscle tone
- Not interacting with parents
- Absent or abnormal cry
- Non-blanching rash
Breathing
- Airway compromise
- Noisy breathing: grunting, gasping or stridor
- Respirations: absent, decreased, moderate or severe respiratory distress
Circulation
- Pale, cold peripheries, mottled skin, cyanosis
- Prolonged central capillary refill time (greater than 2 seconds)
- Fever in those under the age of 3 months
- Active bleeding
bronchoilitis peak by day 4/5 if worse by 3rd day dont dicharge if presented inn 5th day then its peak by then
Arterial assesment per child age
- …
Head to toe examinatoin
Upper airway tachypnea due
-
fever, anxiety
-
streptococcal, adeno, covid
-
trachitis (admit patient, start antibiotics, secure airway if in respiratory distress)
-
epiglotitis (use abdominal muscles)
-
sinusitis
-
Croup (mild/severe; stridor at rest) - managed with corticosteroids, epinephrine
Lower airway
-
Aspiration / chemical Pneumoni
-
consiledation
-
bronchoilitis
-
influenza
DKA quite tachypnea with no fever, may present as normal. - first presentation of DKA.