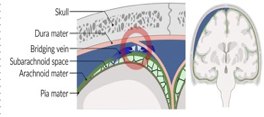
Tear of cortical bridging veins - Trauma, including minor falls, cerebral atrophy, and conditions that increase the risk of bleeding (e.g., coagulopathy, hypertension) are common etiologies of SDH
- Crescentic collection of blood along brain surface (Concave inner margin)
- Common in infants (child abuse) and in the elderly
- Can be acute , subacute or chronic.
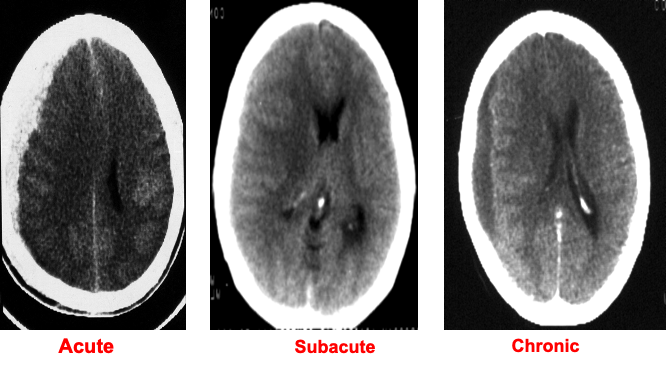
SDH Imaging
CT head without IV contrast :first-line imaging modality.
Characteristic findings:
- Crescent-shaped, concave, sharply demarcated extraaxial lesion
- Can cross cranial suture lines
- Does not cross the midline
- A large unilateral SDH can cause midline shift to the contralateral side.
- Radiodensity of the lesion depends on the length of time since the inciting event:
- Acute SDH: hyperdense
- Subacute SDH: isodense
- Chronic SDH: hypodense
- Acute-on-chronic SDH: hyperdense areas (recent hemorrhage) admixed with isodense or hypodense areas (older hematoma)

Acute subdural hemorrhage - CT head (without IV contrast; axial section; brain window)
There is a large, crescent-shaped, hypodense lesion over the lateral aspect of the left hemisphere. Mass effect of the lesion is visible as compression of the left lateral ventricle. These findings are characteristic of a large chronic subdural hematoma.

Acute on chronic subdural hematoma
Midline shift may be absent or less significant in bilateral SDH.

Subacute subdural hematoma
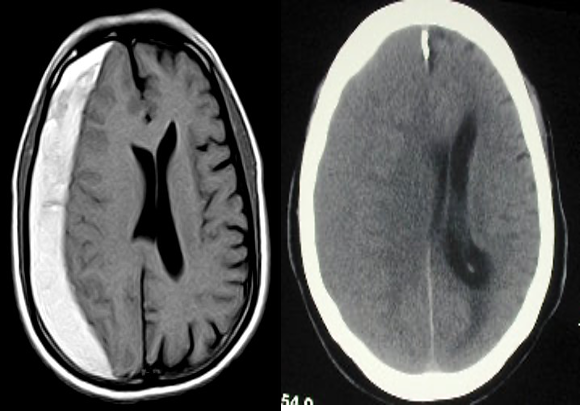 T1- Hyper in subacute
T2 - Hypo - Hyperintense also
T1- Hyper in subacute
T2 - Hypo - Hyperintense also