Therapeutics
-
Pharmacokinetics classification:
a) Lipophilic: propranolol (Anti-arrhythmic) (good absorption –high first pass metabolism in liver –less bioavailability-pass BBB-liver elimination -short duration)
b)Hydrophilic: Atenolol (less absorption-less first pass metabolism-high bioavailability-not pass BBB-renal elimination -long duration 24 hours)
c)Balanced: Bisoprolol
d)Short acting: Esmolol act for 8 min (hydrolyzed by plasma esterase)
Mechanism of Action classification:
A- Beta blocking action: block beta receptors
B) B blocker with intrinsic sympathomimetic activity (ISA): e.g Pindolol-acebutalol ( has less cardio-depression and bronchospasm) Used in patient with low resting heart rate ISA treat/helpful with bradycardia
C) B blocker with membrane stabilizing activity (Na channel blockers): e.g. propranolol (preferred in arrhythmia) may be called Anti-arrthymic effect or Local anaesthetic or quinidine-like action. (primarily used for arrhythmia’s )
- May result claudication, erectile dysfunction
D) Vasodilator B blockers: (due to blocking of αlpha receptor): e.g. carvidelol, labetalol, bucindolol, celiprolol, dilevalol
E) CNS depressant action. (for those passing CNS) Not all beta-blockers have the above-mentioned actions but they differ in their mechanism of action.
Receptor selectivity classification
- NON SELECTIVE BETA-BLOCKERS (1s Gen)=
- block B1, B2, B3
- Liable to cause side effects.
- propranolol , Nadolol
- Beta-1 selective blockers “cardioselective” (2nd gen)=
- block B1 only
- Atenolol ,Metoprolol ,Bisoprolol
- BETA-BLOCKERS WITH V.D. ACTION (3rd Gen)
- e.g carvidelol, labetalol, bucindolol, celiprolol, dilevalol
Prop-nada ⇒ Met-Ate-Biso ⇒ Dile Buci Labe Celi Cervi
Pharmacological Effects
Cardiovascular system
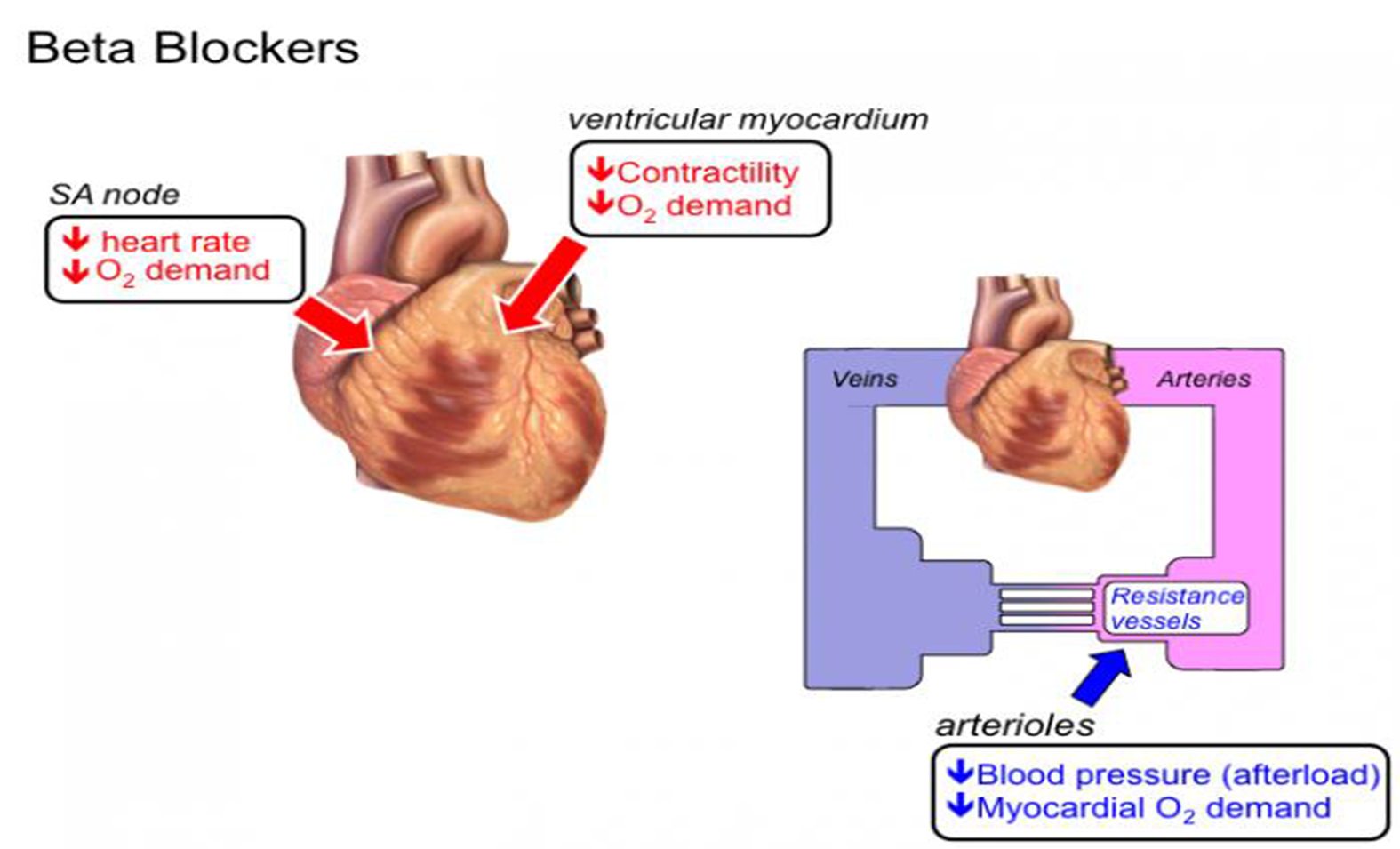
- *Decreases heart rate and myocardial contractility.(B1)
- Slow A-V conduction (B1).
- Quindine like action suppresses ectopic foci in the heart (antiarrhythmic effect).
- Decrease blood flow to most tissues by the unopposed alpha effect in response to reduced COP. (B2)
Lowers blood pressure by:
- Negative inotropic and chronotropic effects lead to decreased COP (B1)
- Decrease renin release(B1)
- Blocks presynaptic B2 receptors lead to decreased NE release.
- Decrease central sympathetic outflow.
- May act through vascular prostaglandins.
- Some B-blockers have vasodilator properties.
- resetting of baroreceptors downwards
Respiratory system: Bronchospasm and increased airway resistance in susceptible patients
Eye: Decreases aqueous humor formation and reduce intra-ocular pressure. Metabolic effects: (contraindication in diabetics)
- In normal individual : no effect on blood glucose. But: Augment hypoglycemic effects of insulin by blocking glycogenolsis and gluconeogenesis. Mask the hypoglycemic symptoms except sweating.
- Increase triglycerides and decrease H.D.L. CNS
- Anti-anxiety effect
- Insomnia, lethargy, night mares, vivid dreams and depression Others: Salt and water retention secondary to the decrease in COP.
Therapeutic Uses:
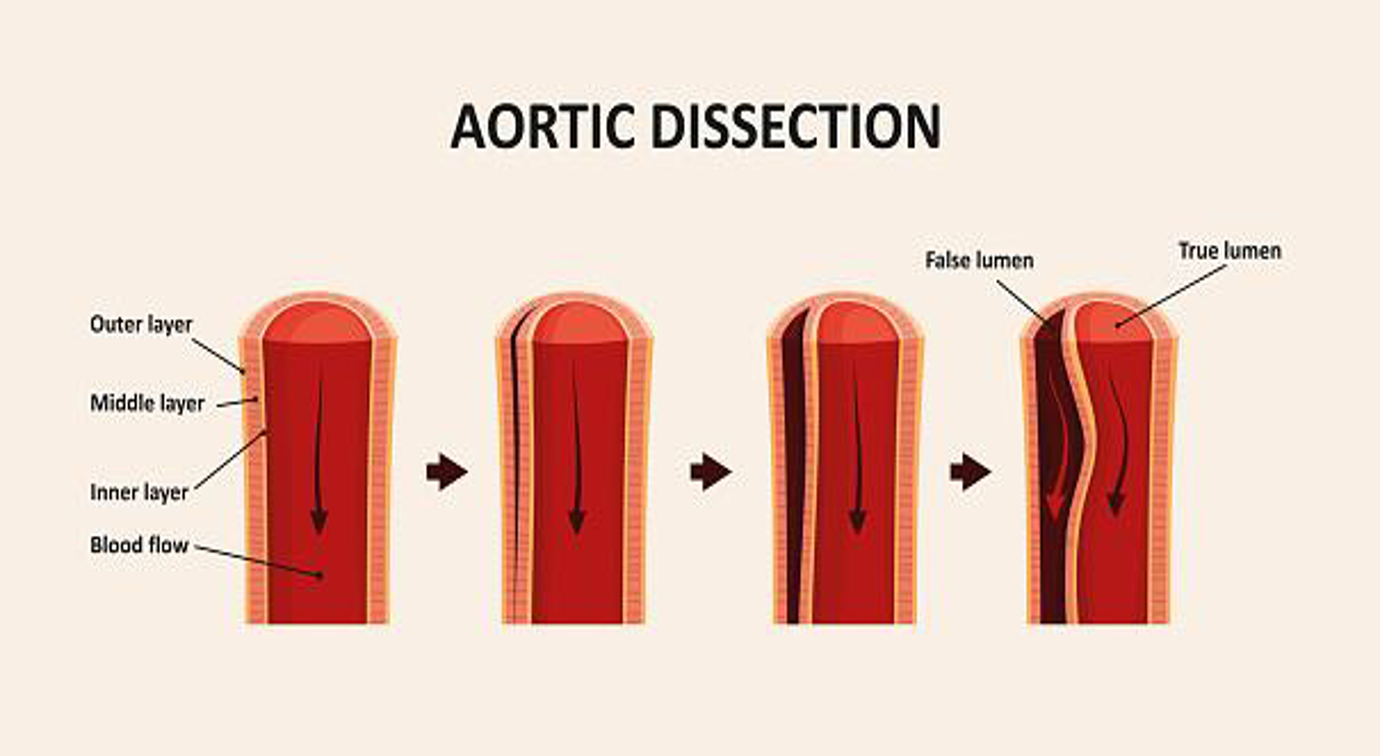
IHD, Arrhythmias, Hypertrophic Obstructive Cardiomyopathy, Stable systolic heart failure, Acute dissecting aortic aneurysm
A- Cardiovascular
-
Treatment of hypertension with a diuretic. Indications: It is of choice in younger patients < 55 y and not black.
-
Ischaemic heart diseases: (angina and infarction)
-
Cardiac arrhythmias:
- Supraventricular arrhythmias especially those produced by exercise, thyrotoxicosis and pheochromocytoma.
- Digitalis induced arrhythmias.
- Arrhythmias induced during surgery (I.V. esmolol).
-
Hypertrophic obstructive cardiomyopathy: by their negative inotropic action.???????? - used till surgery. In hypertrophic obstructive cardiomyopathy, the wall of the left ventricle and interventricular septum is much thickened leading to narrowing of the aortic outlet and obstruction of blood flow. This obstruction is increased by increasing contractility while decreasing contractility leads to decrease resistance to blood flow through the aortic outlet. `Nifedipine is contraindicated because it produces reflex tachycardia → worsening of the outflow obstruction.
-
Stable systolic heart failure (to avoid reflex sympathetic tachycardia and decrease long term exposure of heart to adrenaline . regulate B1 receptor to improve cardiac output) bisoprolol ,metoprolol or carvedilol in small dose)
-
Acute dissecting aortic aneurysm (labetalol)
Combined alpha and beta-blockers: labetalol
- It is selective(a1 blocker and non-selective beta-blocker).
- It has rapid onset of action.
- It is used to control severe hypertension associated with pheochromocytoma and hypertension in pregnant patient.
B-GIT
- Cases of gastrointestinal bleeding by decreasing COP and enhancing splanchenic vasoconstriction.
C-Endocrine
- Hyperthyroidism.
- Pheochromocytoma. (Must be combined with alpha-blockers). (++Labetalol)
D- Eye
- Open angle glaucoma. (Timolol)
E- CNS
- Prophylaxis of migraine
- Anxiety and essential tremors.
Adverse Effects
Reduced blood flow; ischemia, Decrease sexual function & K+, Masking Hypoglycemia
- Heart failure, bradycardia, hypotension.
- Bronchospasm in susceptible patients.
- Potentiation of the hypoglycaemic effect of insulin and oral hypoglycemic drugs and masking of the hypoglycaemic symptoms.
- Peripheral ischaemia, intermittent claudication and cold extremities.
- Reduced blood flow to the liver and kidney reducing metabolism of drugs.
- Hyperkalaemia..
- Nightmares, vivid dreams and depression.
- Nausea, vomiting, diarrhea or constipation.
- Increased plasma triglycerides and decrease HDL.
- Allergic reactions (rash fever)
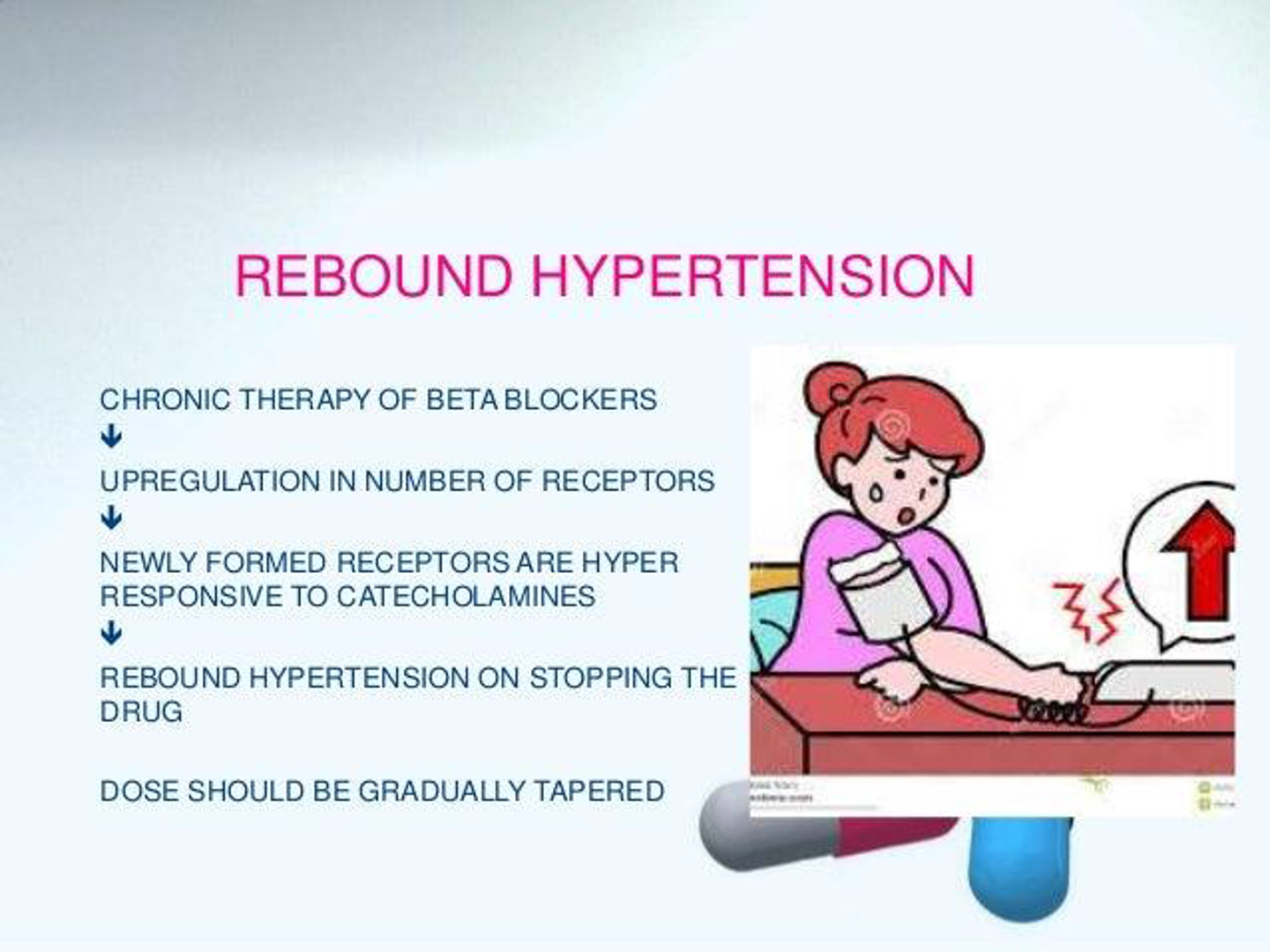
- Sudden withdrawal leads to aggravation of the disease under treatment due to up regulation of beta-receptors.
- Decrease sexual function.
Contraindications
- Congestive heart failure.
- Heart block.
- Variant angina. (why?????????)
- Hypotension.
- Peripheral vascular diseases.
- Bronchial asthma (B2 Action).
- Alone in pheochromocytoma (Severe hypertension).
- Never stopped suddenly (Especially in case of angina) (Rebound Hypertention)
- Diabetes mellitus. (masking of hypoglycemia and increased TAG)
Drug interactions:
A-Pharmacodynamic interactions:
- With calcium channel blockers (verapamil) cause bradycardia, heart block And heart failure
- Aspirin (NSAID) decrease antihypertensive effect as it decrease PGs and Causing salt water retention
- Non selective beta blockers ,Mask hypoglycemic symptoms and Prolong hypoglycemia induced with insulin and oral hypoglycemic drugs
- With epinephrine cause severe hypertension due to unopposed alpha vasoconstriction
B-Pharmacokinetic interactions:
- Enzyme inducers increase metabolism of lipophilic beta blockers
- Enzyme inhibitors decrease metabolism of lipophilic beta blockers
- propranolol decrease hepatic blood flow and decrease metabolism Of flow dependent drugs (lignocaine)
IHD
Reducing anginal episodes and improving exercise tolerance.
The only antianginal drugs proven to prevent reinfarction and to improve survival in patients who have sustained an MI.
Doses are usually tolerated to reduce the resting heart rate to 55-60 beat per minute.
Mechanism in angina:
-
Reduction of myocardial O2 demand through ↓ both heart work and systemic BP.
Bradycardia leads to ↑ diastolic filling time and improvement of myocardial perfusion
Redistribution of blood from normal to ischemic areas. -
Cytoprotective effect through improving glucose utilization by shifting tissue metabolism toward a greater use of carbohydrate and a lesser use of free fatty acids
Combination of BBs and nitrates ↑ their efficiency and ↓ their side effects:
Beta-blockers e.g (propranolol) are contraindicated in Prinzmetal’s (variant) angina (selective a1 receptor) because they block the β2-mediated coronary dilatation leaving the α1 receptors unopposed → ↑ coronary spasm.
ACS
B adrenoceptor blockers reduce heart rate, blood pressure and myocardial contractility and they stabilize heart electrically. These actions are limiting myocardial oxygen consumption, relieving ischemia, reducing infarct size, and preventing serious arrhythmias.
Early B-blockade is recommended for acute MI patients without severe L V failure or other contraindications.
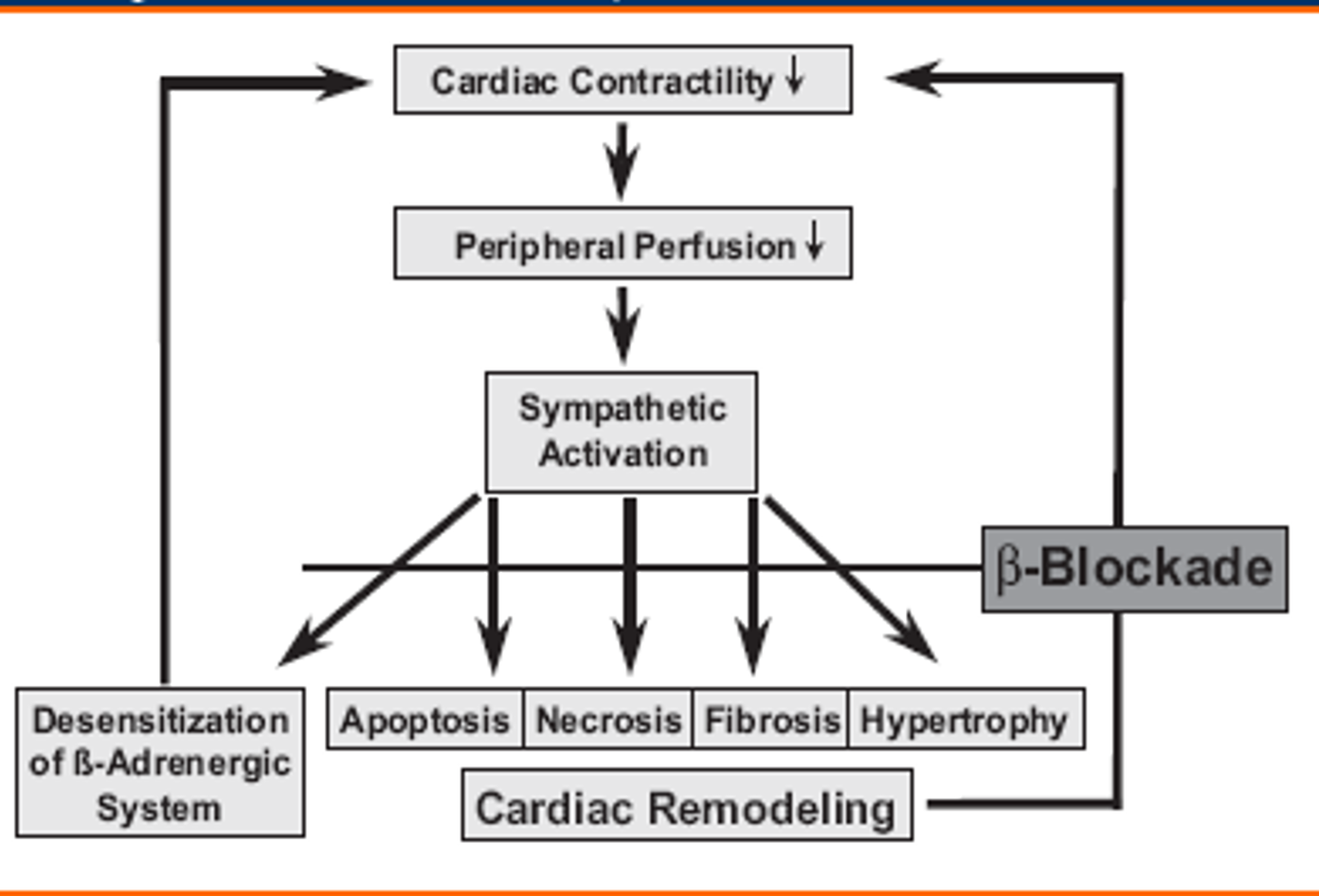
HF
Rational for use of β-blockers in heart failure:
β-blockers are generally not recommended in heart failure because they produce –ve inotropic effect and cardiac decompensation.
-
Specialist use only
-
Start at low dose and monitor for bradycardia -Beta Blockers therapy in chronic heart failure ( in NYHA II,III)
-
β-blockers ↓ cardiac remodeling through inhibition of the mitogenic activity of catecholamines and renin-ang-II system.
-
Carvedilol, Also, BISOPROLOL and METOPROLOL Beta blockers are used in selected patients (mild/moderate failure)
Beta-blockers are specially indicated in the following cases:
Used to prevent or partially reverse progressive left ventricular dilatation.
-
HF associated with ↑ sympathetic overactivity. Stable systolic heart failure (to avoid reflex sympathetic tachycardia and decrease long term exposure of heart to adrenaline so up regulate B1 receptor to improve cardiac output)
-
HF associated with pheochromocytoma.
-
HF associated with thyrotoxicosis. Beta-Blockers Thyroid
Ophthalmology
Beta Receptors
- Beta 1 receptors: located in the heart when stimulated cause tachycardia
- Beta 2 receptors: located in the bronchi and ciliary epithelium when stimulated cause bronchodilatation and increase in the aqueous production
Beta-Adrenergic Blockers
- E.g.
- Non-selective: timolol, levobunolol
- Selective: betaxolol (beta 1 “cardioselective”)
- Uses: glaucoma
- Mechanism: reduce the formation of aqueous humor by the ciliary body
- Side effects: bronchospasm (less with betaxolol), cardiac block

Beta Blockers Complications
- Dry eyes
- Bradycardia
- Hypotension
- Bronchospasm (may be fatal in asthmatic pts and pts with COPD)
- Impotence, lethargy, depression, may mask hypoglycemic attacks in diabetic pts.
Beta Blockers Contraindications
- Asthma
- COPD
- 2nd and 3rd degree heart block
- Congestive heart failure