Sys = Cardiac output & Rate Diastolic = Peripheral ± Vasoconstriction and less perfusion to organs
- Na+ potentiates Catecholamines & angiotensin stimulation ⇒ increased Ca+ = Vasoconstriction
- P+
- Resetting of Baroreceptors to a higher level
- Anxiety
Drug induced hypertension
Oral contraceptives, corticosteroids,, cyclosporine, clonidine withdrawal , carbenoxolone, cocaine , sympathomimetic agents (Cold medications) , NSAIDs, liquorice,, erythropoietin
systemic hypertension:
Persistent or recurrent elevation of systemic blood pressure greater than or equal to 140/190 mmHg. even after period of rest
Blood pressure is a characteristic of each individual like weight and height, with marked inter-individual variation.
Diagnosis of hypertension should be made only after finding an elevated blood pressure on three readings on different occasions. However, patients with very high blood pressure reading should be started on therapy immediately. Ambulatory 24 hours –blood pressure (monitoring) reading in may be helpful in evaluating in patients with (white coat hypertension)
Epidemiology
Hypertension is a condition that affect almost 1 billion people worldwide and is a leading cause of morbidity and mortality.
More than 20% of Americans are hypertensive, and one-third of these Americans are not even aware they are hypertensive. Therefore, this disease is sometimes called the “silent killer“ or The Silent Enemy! Up to 26.3% of adults in Egypt have hypertension.
Measurement is the only way to know if you have hypertension — you will not feel it until it is too late!
Categorization Of Hypertensive Patient
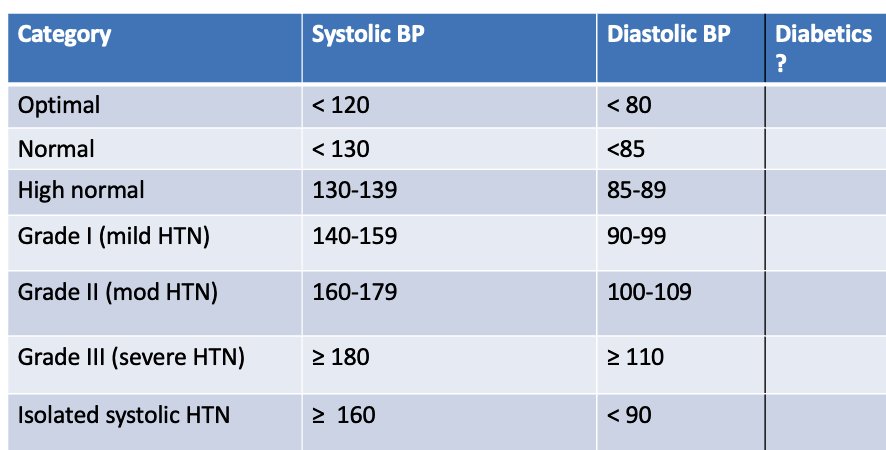
Types of Hypertension
- Isolated systolic HTN
- Systolic & Diastolic HTN
Etiology
A- Essential (Primary hypertension): In more than 95%of cases, an underlying cause cannot be found.
B- Secondary Hypertension: In about 5% of cases an underlying cause can be found:
C) According to persistence:
- *Labile hypertension: occasionally elevated.
- *Persistent hypertension: continuously elevated.
D) Benign or malignant hypertension:
-
*Benign means affection of medium and large sized arteries.
-
*Malignant: it affects arterioles and small arteries with endarteritis obliterans and necrosis which lead to organ damage.
E- Renal: It accounts for 80% of the cases of secondary hypertension.
Complications of untreated hypertension(Target organ damage)
1-Blood vessels: Wide spread atheroma formation leading to coronary and or cerebrovascular disease, particularly if other risk factors (e.g. smoking, dyslipidemia, diabetes) are present.
2-Central nervous system:
- Stroke (due to hemorrhage or thrombosis and transient ischemic attacks (TIAs) are more common in hypertensive patients.
- Subarachnoid hemorrhage
- Hypertensive encephalopathy: a condition of high blood pressure and neurologic symptoms, usually reversible if hypertension is controlled.
- Symptoms include disturbances of speech and vision, disorientation, fits and loss of consciousness.
3-Retina:
- Papilledema is common.
- Changes are associated with hypertension include retinal ischemia or infarction and also central retinal vein thrombosis.
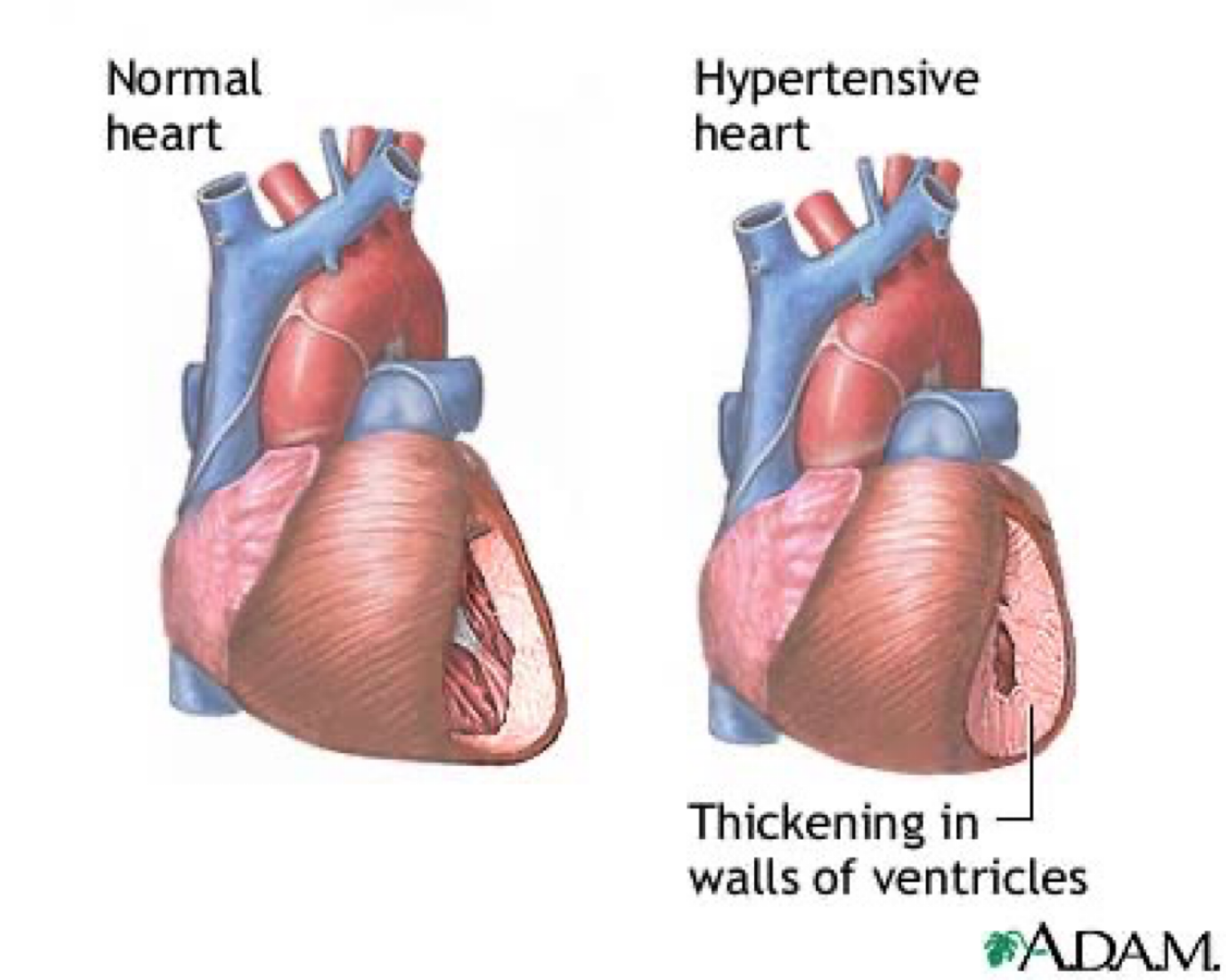
4-Heart:
- Higher incidence of coronary artery disease
- Left ventricular hypertrophy (forcible apex and S4, ECG and echocardiographic evidence)
- Left ventricular failure in severe hypertension even in the absence of coronary artery disease.
5-Kidneys:
Long standing hypertension may lead to proteinuria and renal failure due to damage of renal vasculature.
Clinical pictures of Hypertension
A- Uncomplicated: No symptoms ⇒ headache (occipital) ⇒ Diziness ⇒ Vertigo ⇒ Tinnitus ⇒ Palpitation
B- Complicated HTN: 1- CV complications: * LVH & Failure * CAD * Aortic dissection * Hemorrhage e.g epistaxis. 2- Cerebral: * TIA * Hypertensive encephalopathy * Cerebral thrombosis & Hge * Subarachnoid Hge. 3- Renal: * Proteinuria & microscopic hematuria * Nephro-sclerosis with RF in 10-20% esp. in malignant HTN.
4- Retinal complications: Hypertensive retinopathy * G 1⇒ Narrowing of retinal arteries & mild sclerosis. * G 2 ⇒ Marked sclerosis of retinal art. with compression of the veins at points of crossing (A-V nicking). * G 3⇒ Oedema, Hge & cotton-wool spots & markedly spastic arteries. * G 4⇒ Papilloedema ( malignant HTN).
Signs & Symptoms
1 - High blood pressure:
-
BP should be measured in the sitting or the supine position with the arm supported after 5 minutes resting.
-
Standing BP should be measured in the elderly and those suffering from positional hypotension (diabetics and patients on antihypertensive medications) to exclude orthostatic hypotension.
2- Signs of secondary hypertension:
- Radio-femoral delay (coarctation of the aorta)
- Enlarged kidneys (polycystic kidney disease)
- Abdominal bruits (renal artery stenosis)
- Moon face and trunkal obesity ( cushing syndrome)
3- Signs of other cardiovascular risk factors:
- Abdominal obesity (metabolic syndrome)
- Tendon xanthomas (hyperlipidemia)
4- Signs of end organ damage and complications:
- Retinopathy:
- Stage I arteriolar narrowing
- Stage II arteriolar irregularity
- Stage III hemorrhages and exudates
- Stage IV papilledema associated with severe life threatening disease. (Malignant hypertension)
- Cardiac: Left ventricular enlargement or failure.
- Peripheral vascular disease: weak or absent peripheral pulsation
- Carotid vascular disease (carotid bruit).
- CNS: Cerebrovascular disease (stroke).
Investigations
1- All hypertensives:
- Urine: for blood, protein and glucose
- Blood urea and serum creatinine. If elevated, more specific renal investigations are as creatinine clearance.
- Electrolytes (hypokalemia may occur in primary hyperaldosteronism or more commonly due to diuretic therapy)
- Blood glucose, lipid profile (total and high density lipoprotein cholesterol).
- ECG: Left ventricular hypertrophy (LVH) & Coronary artery disease (CAD).
2- Investigations In selected cases:
Imaging:
- Chest x ray: (cardiomegaly, heart failure, co-arctation).
- Ambulatory BP monitoring: (borderline or white coat hypertension).
- Echocardiography: left ventricular hypertrophy (L VH).
- Abdominal ultrasound (possible renal disease).
- Renal angiography, MR & CT angiography, renal arterial duplex (renal artery stenosis).
Laboratory:
- Urinary catecholamines e.g VMA, free metanephrins (pheochromocytoma).
- Urinary cortisol and Dexamethasone suppression test (Cushing’s syndrome).
- Plasma renin and aldosterone (primary aldosteronism).
- Sensitive thyroid-stimulating hormone level.
The pathogenesis of primary type is unknown but multiple theories and the most important is multifactorial theory: Z
Anxiety:
-
Increases catecholamine release.
-
If vasoconstriction is prolonged: renal ischemia occurs which stimulates rennin angiotensin system which leads to Na and H2O retention which leads to hypervolaemia with Na retention in SMF which sensitizes blood vessel wall to sympathetic stimulation and to circulating vasopressors (catecholamines and angiotensin) so, increases calcium in blood vessel which leads to vasoconstriction.
-
Resetting of baroreceptors to a higher level.
Others:
-
Hyperinsulinemia as part of metabolic syndrome: hyperinsulinemia , glucose intolerance, reduced levels of HDL cholesterol, hypertriglyceridemia and central obesity (all of which are related to insulin resistance).
-
Alterations in vascular endothelium resulting in reduction of vasodilators or increase in vasoconstrictors