INTRODUCTION
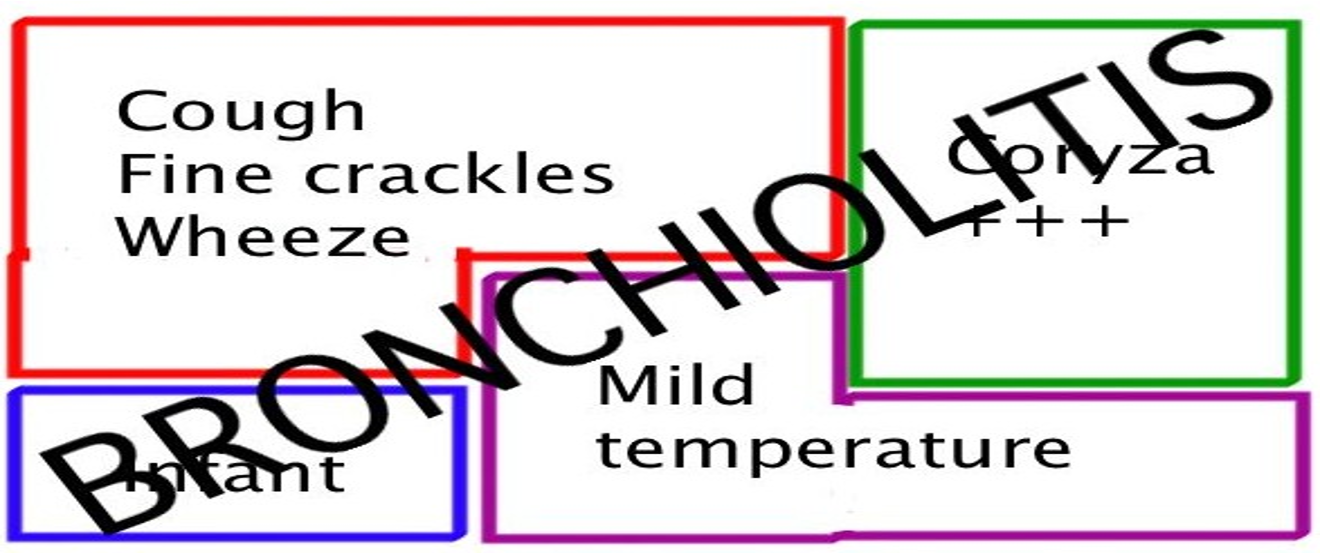
Bronchiolitis is a lower respiratory tract infection that occurs in children younger than two years old, with peak incidence at around 6 months.
Usually caused by a virus → inflammation of the small airways (bronchioles).
Bronchiolitis can cause serious illness in some children (very young infants, born early, lung or heart disease).
ETIOLOGY
- Bronchiolitis is typically caused by a virus.
- Respiratory syncytial virus (RSV) is the most common cause in ˃ 50% of cases.
- Common in winter and early spring.
- First 2 years of life, more in males and in non-breastfed.
- Children who are older than two years typically do not develop bronchiolitis, but can be infected with RSV.
- RSV infection is common in children older than two years. It usually causes symptoms similar to those of the common cold or mild wheezing and at times the illness is significant enough to require evaluation by a healthcare provider.
OTHERS:
- Parainfluenza virus, adenovirus, influenza virus, mycoplasma
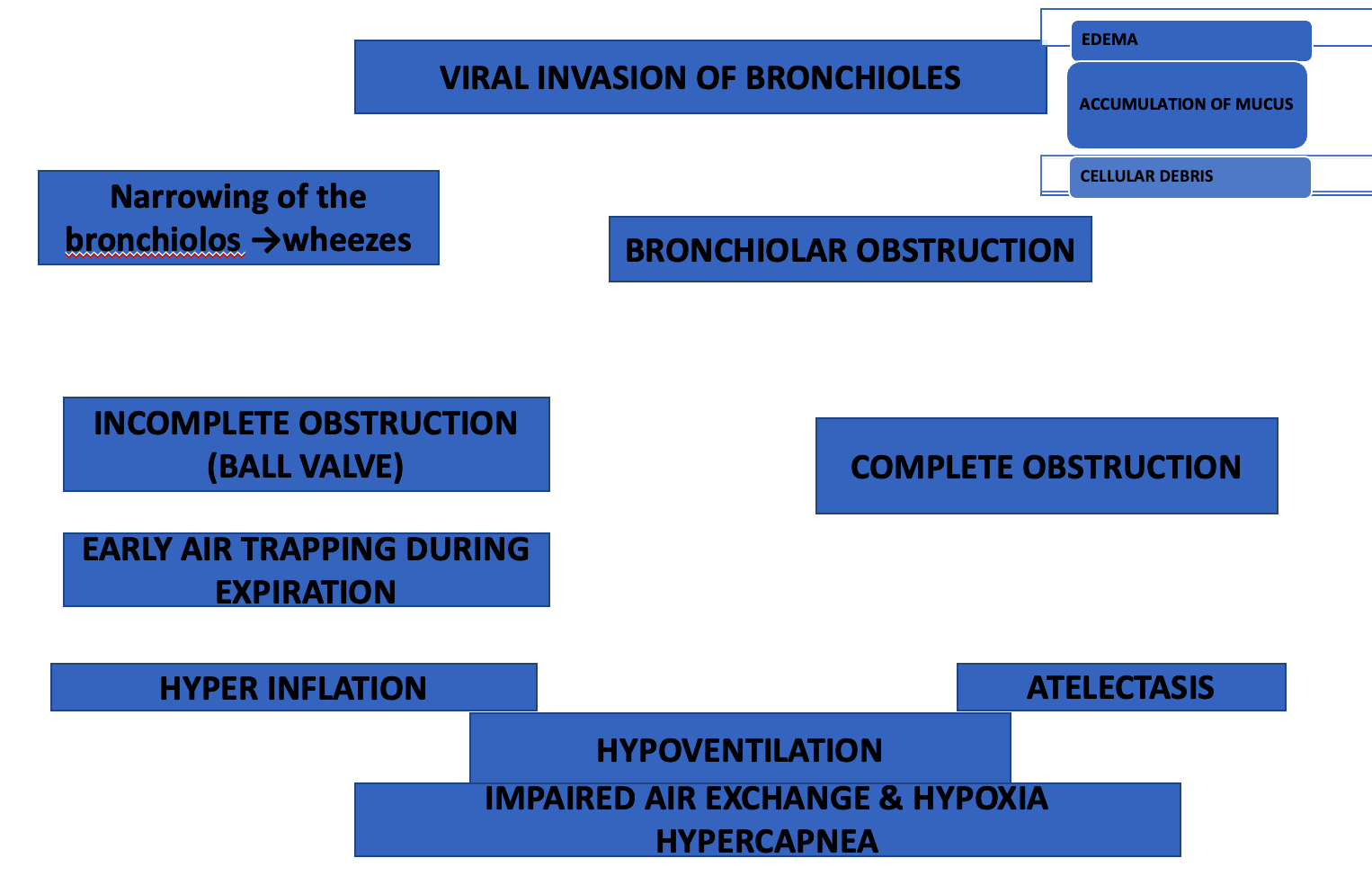
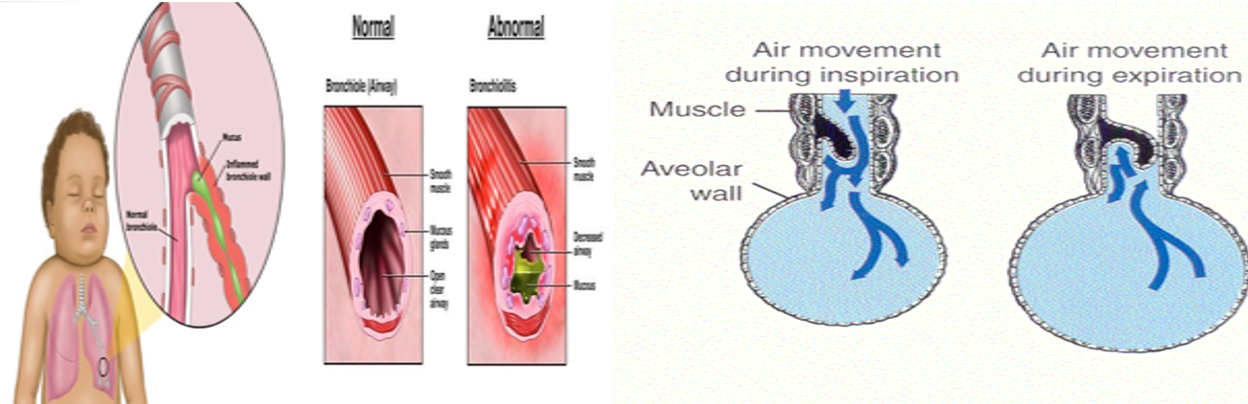
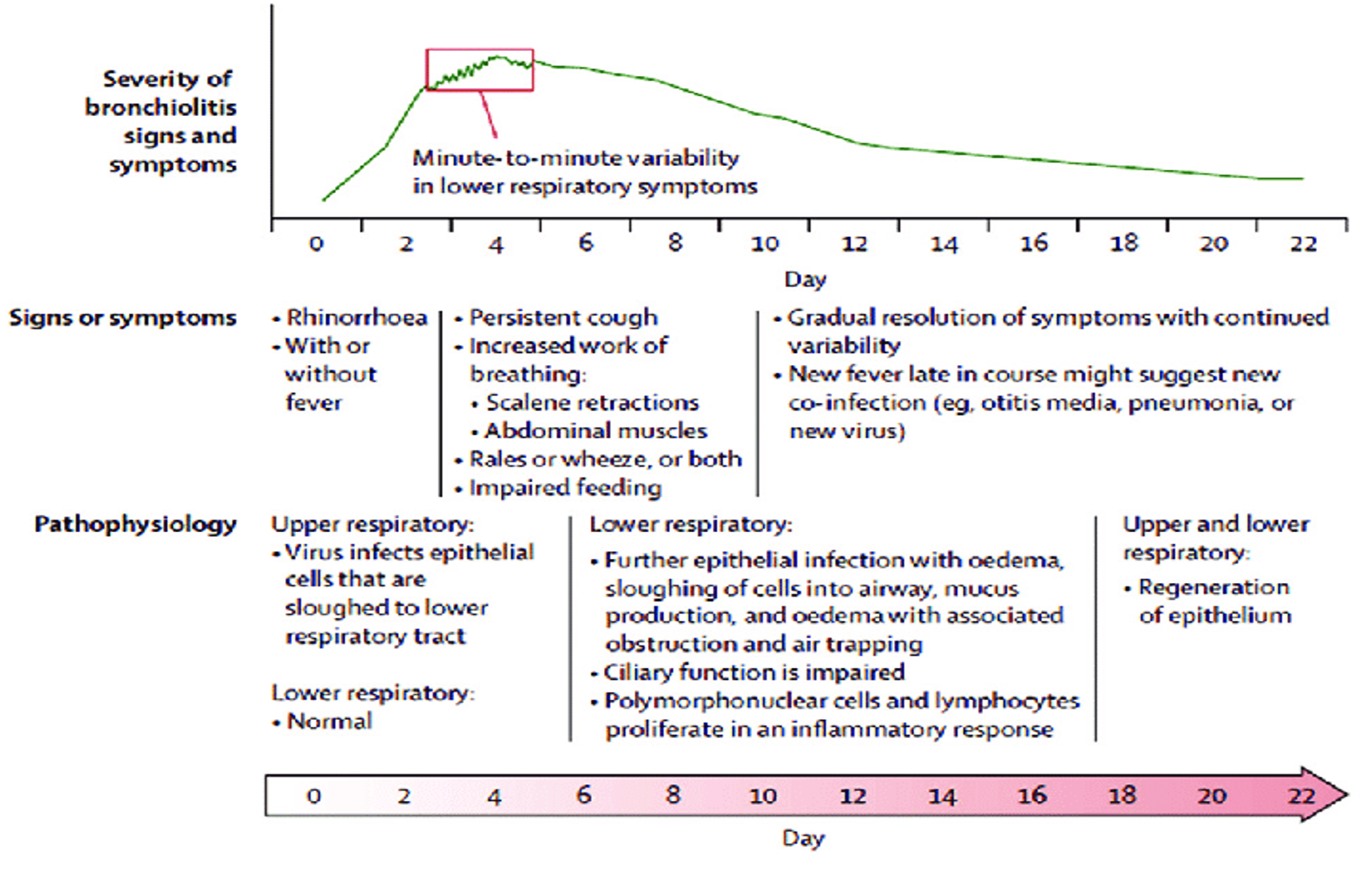
PATHOGENESIS
- Acute infection → respiratory obstruction of the small airways.
- Viral invasion of the smaller radicles of the bronchial tree → edema + accumulation of mucus and cellular debris → bronchiolar obstruction.
CLINICAL PICTURE
SYMPTOMS
- History of exposure to an older person with minor respiratory distress.
- Mild upper respiratory tract infection (URTI) for 2-3 days.
- Followed by gradual onset of respiratory distress:
- Paroxysmal spasmodic cough, wheezes, dyspnea, irritability, feeding difficulty due to tachypnea, recurrent apnea
- In mild cases, symptoms resolve within 5-7 days.
- In severe cases, the course is more protracted.
SIGNS
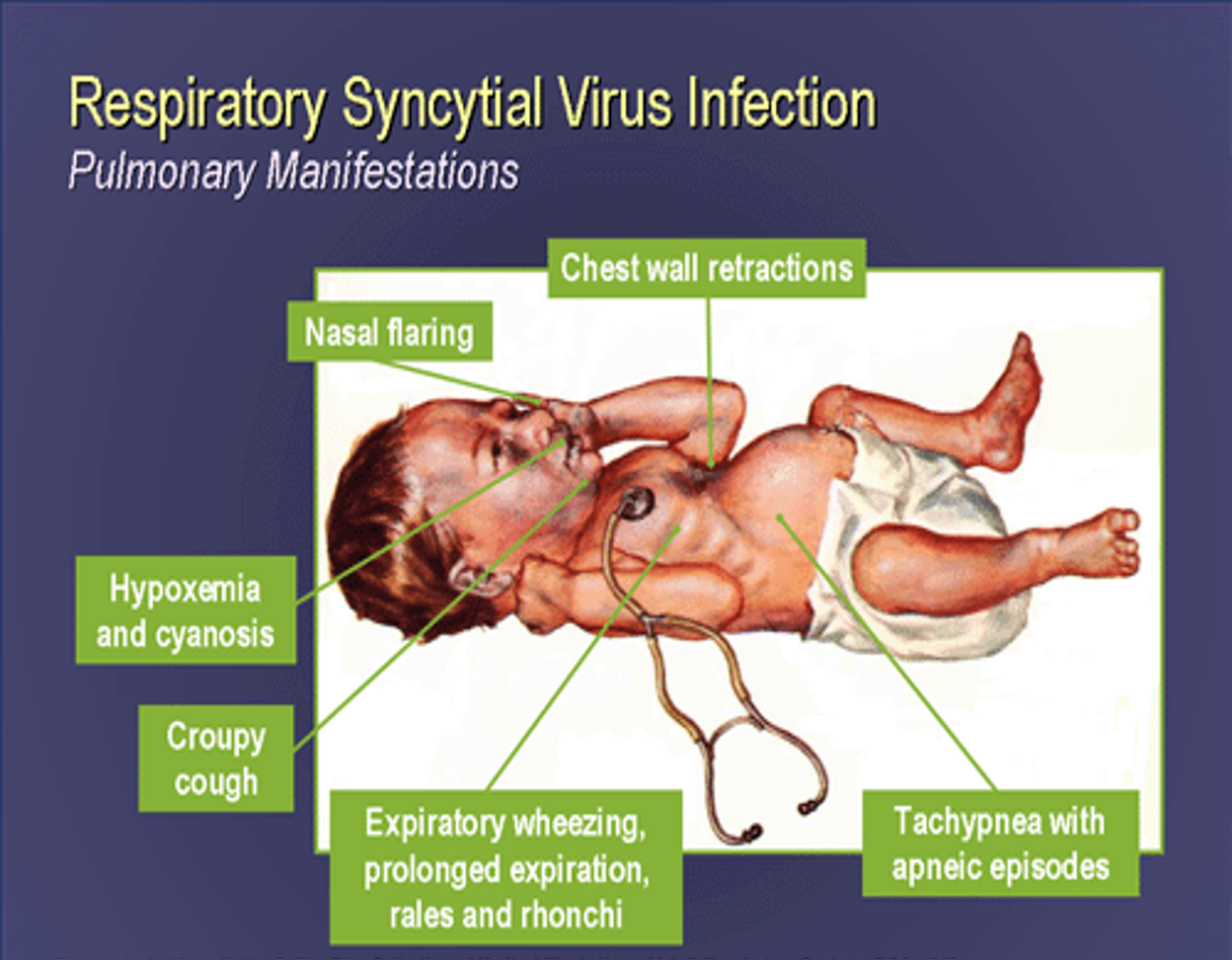
TACHYPNEA | RESPIRATORY DISTRESS | WHEEZES | HYPERINFLATION
INSPECTION:
- Fast, shallow respiration. - R.R. 60-80/minute.
- Flaring ala nasi. - Chest indrawing. - Intercostal retraction.
- Air hunger. - Restlessness. - Cyanosis.
- Hyperinflation of the chest (prominent sternum, liver displaced downwards)
AUSCULTATION:
- ↓ air entry.
- Harsh vesicular breathing with prolonged expiration.
- Inspiratory and expiratory wheezes.
- Inspiratory widespread fine crackles.
PERCUSSION:
- Hyper resonant note due to over-inflated lungs.
DIAGNOSIS
Young infant with mild URI followed by: Respiratory distress + wheezes + over-inflated chest
LAB FINDINGS:
- The diagnosis of bronchiolitis is based upon a history and physical examination. Blood tests and x-rays are not usually necessary.
- Leukocytic count normal or mild increase.
- PO2, PCO2, and PH may be measured to assess the severity of the disease.
- RSV may be demonstrated in nasopharyngeal secretions by immunofluorescence or PCR
- Rising antibody titre to RSV in serum.
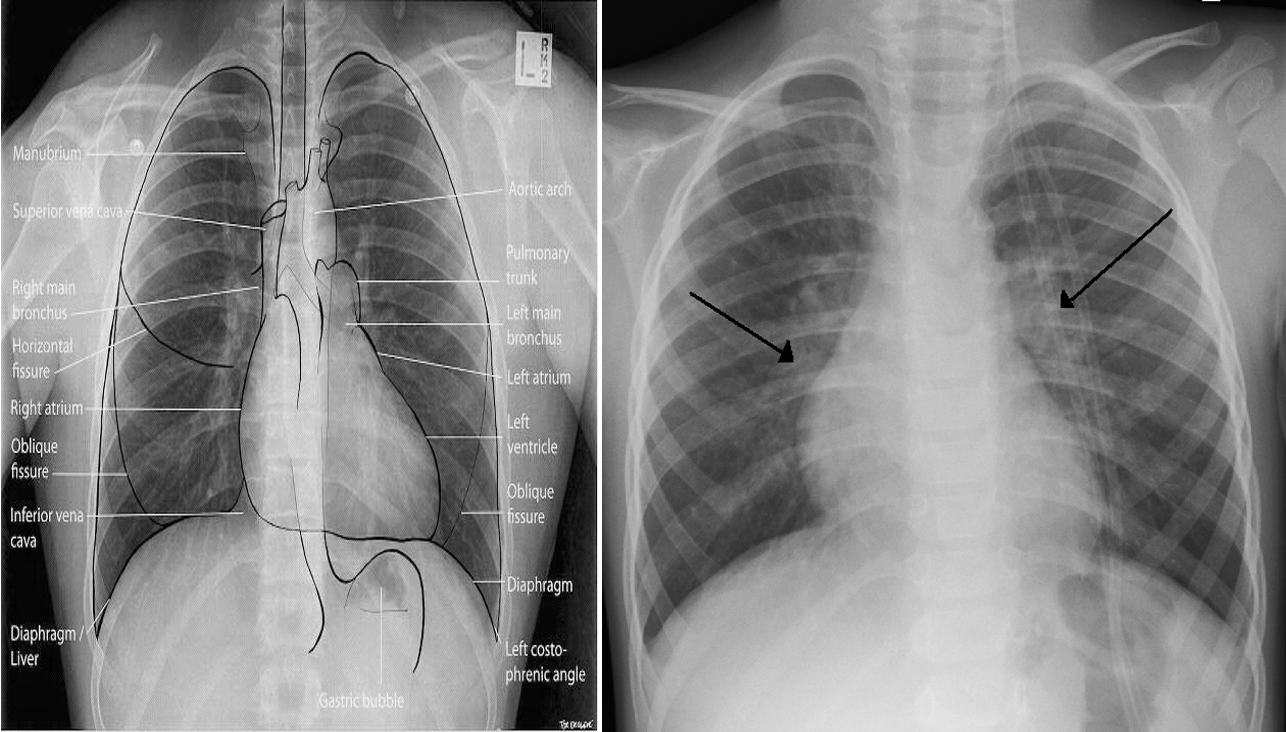
X-ray finding
- Hyperinflated lungs.
- In 30% scattered areas of opacity due to consolidation or atelectasis.
- An X-ray of a child with RSV showing the typical bilateral perihilar fullness of bronchiolitis.
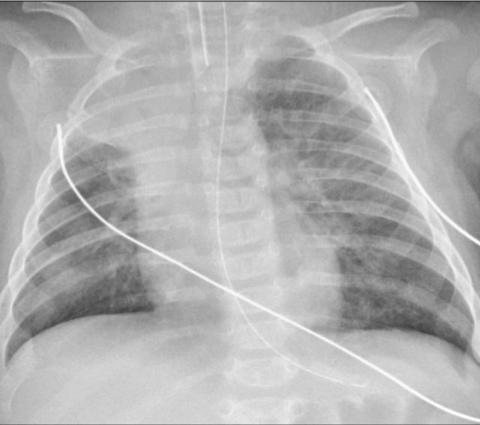
Chest radiograph of a 3-month-old infant with severe RSV bronchiolitis: demonstrating a collapsed right upper lobe, hyperinflated left lung and bilateral perihilar, peribronchial thickening. The patient is intubated and has a nasogastric tube in situ.
DIFFERENTIAL DIAGNOSIS
- Bacterial bronchopneumonia
- Cystic fibrosis
- Congestive heart failure
- Organophosphorus poisoning.
- Recurrent viral-induced wheeze
- Early asthma
- Pertussis
- Recurrent aspiration
- Foreign body in trachea
- Congenital lung anomaly
COMPLICATIONS
- Bacterial superinfection uncommon.
- Cardiac failure rare
- Death due to severe course
- Recurrent apnea is a serious complication especially in young infants.
TREATMENT
The healthcare provider must determine if the child’s illness is severe or if there is a risk of complications.
In these cases, hospitalization is generally recommended to closely monitor the child and provide intravenous fluids or supplemental oxygen.
Discharge to home:
- Most children who require hospitalization are well enough to return home within three to four days.
- Children who require a ventilator usually need to stay in the hospital for four to eight days or longer before they are ready to go home.
if less than <3m Always admit - make sure to check O2 if less than 92 admit if >3m if high risk patient admit - regardless of course
AT HOME
Give plenty fluids - prone to dehydration
There is no cure for bronchiolitis, so treatment is aimed at the symptoms (e.g., difficulty breathing, fever).
- Semi-sitting position (30-40 degrees) makes the infant more comfortable.
- Fever control: acetaminophen, Ibuprofen
- Nose drops or spray
- Encourage fluids
Other therapies:
- Such as antibiotics, cough medicines, decongestants, and sedatives, are not recommended.
- Monitoring at home involves observing the child periodically for signs or symptoms of worsening (increased rate of breathing, worsening chest retractions, nasal flaring, cyanosis, a decreased ability to feed or decreased urine output).
SUPPORTIVE TREATMENT
-
Semi-sitting position (30-40 degrees) makes the infant more comfortable.
-
Oxygen:
- Cool humidified oxygen by nasal cannula, or by placing a face mask over the nose and mouth. For infants, an oxygen head box (a clear plastic box) may be used.
- If a child is severely ill and unable to breathe adequately on his or her own, or if the child stops breathing, an endotracheal tube may be inserted and connected to a ventilator that breathes for the child at a regular rate.
- The use of an endotracheal tube and ventilator is a temporary measure that is discontinued when the child improves.
-
Fluids: Parental + oral.
-
In case of respiratory acidosis, suitable I.V. fluids are given to adjust PH and electrolytes.
-
Avoid sedatives.
-
Good nutrition
-
Antiviral (ribavirin) is given only to those with documented severe RSV disease or high-risk infants. It is given by continuous inhalation by aerosol generator 10-12hr/day for 3-4 days.