BREAST DISEASES
DR. AHMED KHAN
Diseases of the Breast
Benign Disorders
Benign Neoplasms
Malignancy
Unusual Malignant Tumors
-
Paget’s disease (Nipple ulceration)
-
Inflammatory breast carcinoma
-
Malignant Phyllodes Tumor
-
Malignant lymphoma: Rare
Diagnosis (triple assessment)
I. Clinical evaluation – Breast History & Examination
II. Radiological evaluation:
- U/S
- Mammography
- MRI
- CT scan (for staging)
III. Cytological/ histological evaluation:
- FNAC
- Core biopsy (U/S or Mammography guided for non-palpable mass)
- Open biopsy- excision of the mass with surrounding healthy tissue.
Imaging for Breast Disease
-
Mammography
-
Ultrasonography
-
MRI
- High sensitivity for breast cancer.
- Used for screening high-risk women.
- Optimum method of imaging breast implants and detecting implant leakage or rupture
- Recurrent diseases
Biopsy
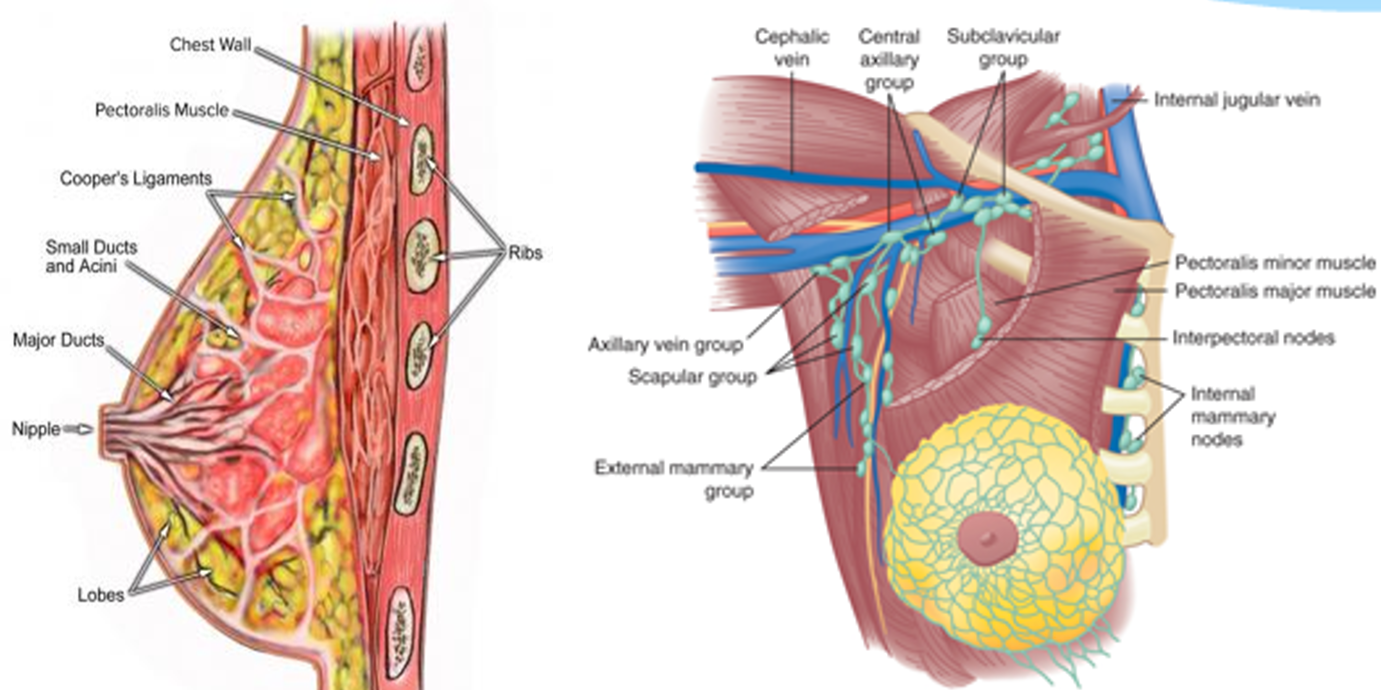
Anatomy of the Breast
-
Located between the subcutaneous fat and the fascia of the pectoralis major and serratus anterior muscles.
-
Extend to the clavicle above, laterally to axilla and latissimus dorsi, medially to sternum and inferiorly to the top of the rectus muscle (inframamry crease).
-
Axillary tail blends with axillary fat.
-
Made up of milk-producing glands.
-
Arranged into units known as lobules.
-
Glands connected via ducts that join to form a common drainage path, terminating at the nipple.
-
The nipple is surrounded by a ring of pigmented tissue- areola.
-
Fibro-elastic and fatty tissue provide support for the rest of the structure.
Lymphatics:
-
interlobular lymphatic vessels to a subareolar plexus (Sappey’s plexus), 75% of the lymph drains into the axillary lymph nodes.
-
Medial breast drain into the internal mammary or the axillary nodes.
Axillary Lymph Nodes
-
Level I: Lateral to the pectoralis minor muscle. Usually involved first.
-
Level II: Posterior to the pectoralis minor muscle.
-
Level III: Medial to the pectoralis minor muscle.
-
Rotter’s nodes: Between the pectoralis major and the minor muscles.
Physiology
- Composed of glandular tissue, fibrous supporting tissue and fat.
- Functional unit: Terminal duct, lobular unit.
- Secretion from lobular unit drain by 12-15 major subareolar ducts.
- Rest: Terminal duct lobular unit secrete watery fluid which is reabsorbed.
- Pregnancy: Lobules & ducts proliferate.
- Delivery reduces circulating estrogen and increases sensitivity to prolactin.
- Suckling stimulates prolactin & oxytocin- ejection of milk.
- Involution starts after 30- atrophy of glandular and fibrous tissue
Evaluation of Patients with Breast Disease
Common complaints:
- Lump (most common)
- Pain/ tenderness (Mastalgia)
- Change in the breast size/ skin (redness, Peau d’orange)
- Change in the nipple
- Discharge from the nipple
Hormone & Growth Factor Receptors
-
ER (estrogen receptor) +ve. tumors (75%) are estrogen-dependent for growth. Depriving estrogen stops its growth (Tamoxifen).
-
PR (progesterone receptor) +ve. are hormone-dependent.
-
ER & PgR negative tumor (20-25%)- no benefit of hormone treatment.
-
HER 2 (human epidermal growth factor receptor) +ve tumors (15%) are dependent on this growth factor. This can be blocked by monoclonal antibody- Trastuzumab (Herceptin) which is used in treatment.
- HER2 tumors have a worse outlook than HER2 negative.
-
Triple negative (ER, PR,HER2): worse prognosis.
Clinical Features
Asymptomatic (screening detected).
Symptomatic:
- Lump 76%- painless, ill-defined, skin attachment, peau d’orange
- Pain 5%
- Nipple retraction (whole nipple is pulled in)
- Discharge
- Skin retraction (Dimpling)
- Axillary mass
BOOK REFERENCE
PRINCIPLES AND PRACTICE OF SURGERY
6th edition:
Edited by
- O. James Garden,
- Andrew W. Bradbury
- John L.R. Forsythe
- Rowan W. Parks
PAGE NO: 302-11