/
Normal Menstrual Cycle Manifestation and Control
Manifestation of normal menstrual cycle Is: Presence of regular vaginal bleeding as a result of
- ➡️ shedding of the endometrial lining following
- ➡️ failure of fertilization.
The cycle depends on: Changes occurring in ovarian hormones
Which controlled by:
- Pituitary
- Hypothalamus
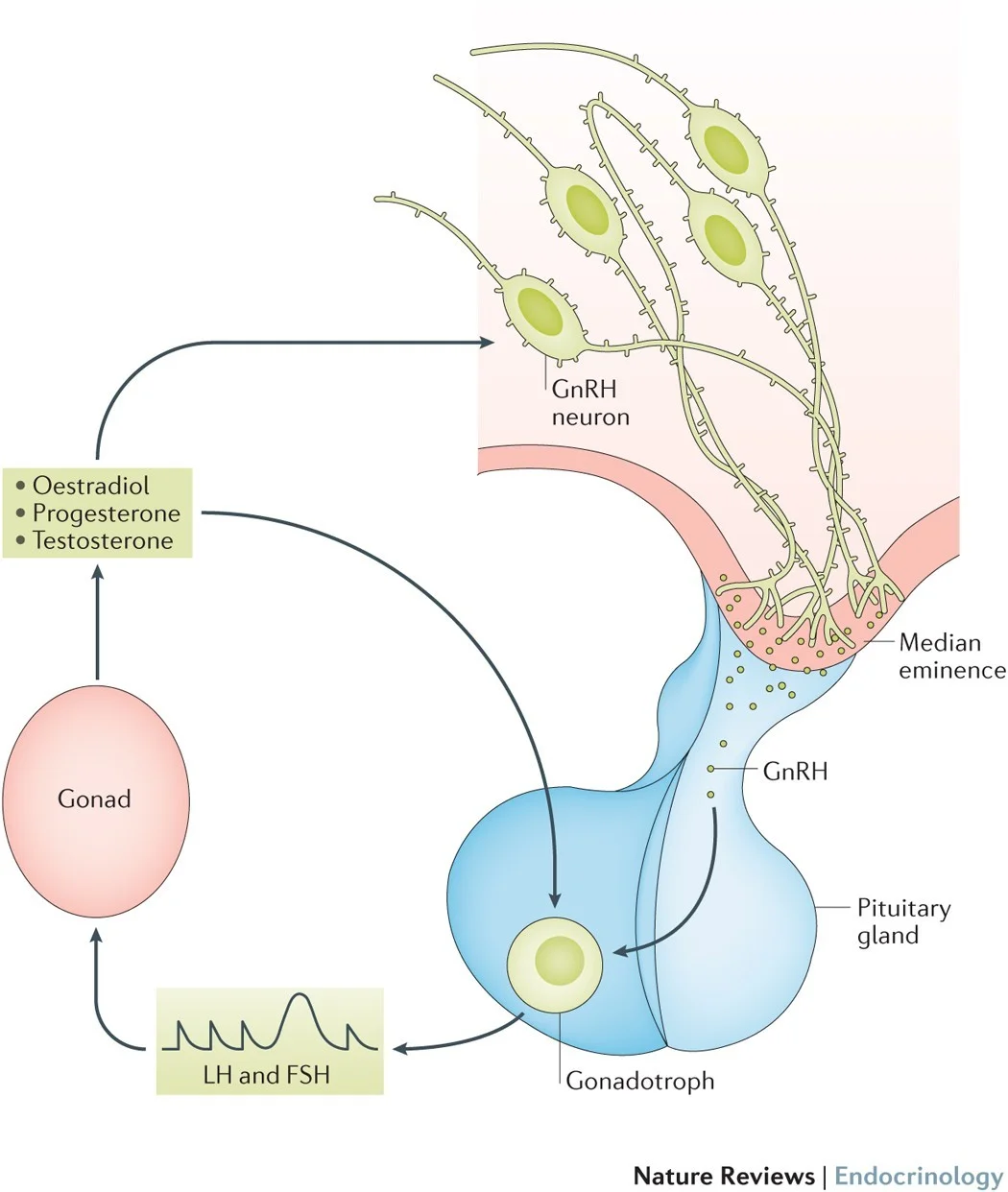
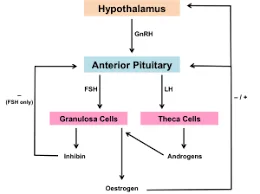
The hypothalamo–pituitary–ovarian axis (HPO). Hormonal abnormalities lead to menstruation abnormalities.
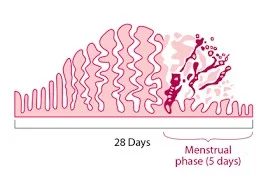
28 Days Menstrual phase (5 days)
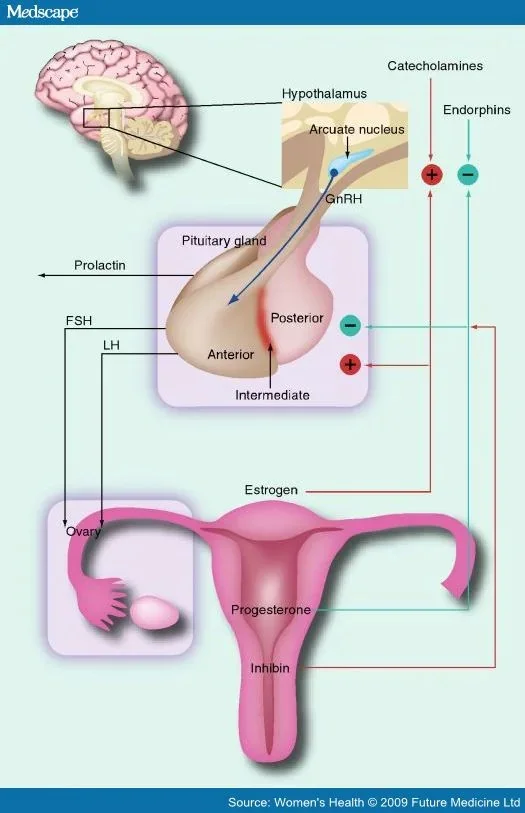
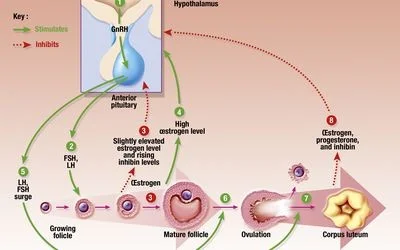
The Hypothalamus
- Secretes gonadotrophin-releasing hormone (GnRH)
- which controls hormone secretion in the:
- anterior pituitary gland
- ✓ luteinizing hormone (LH)
- ✓ follicle-stimulating hormone (FSH)
- anterior pituitary gland
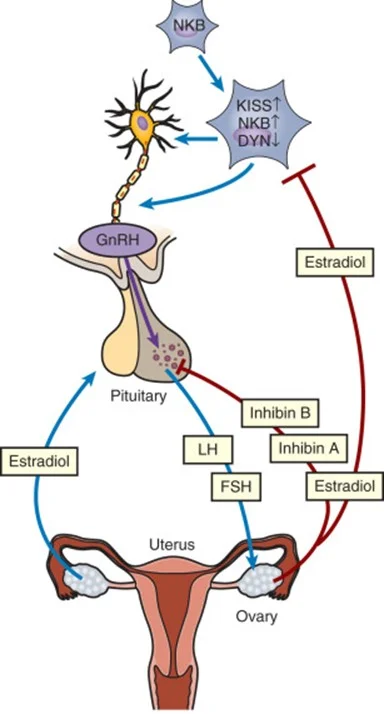
- ➤ GnRH released in a pulsatile pattern
- ➤ This process is modulated by the ovarian sex steroid hormones
- oestrogen and progesterone
- which controls hormone secretion in the:
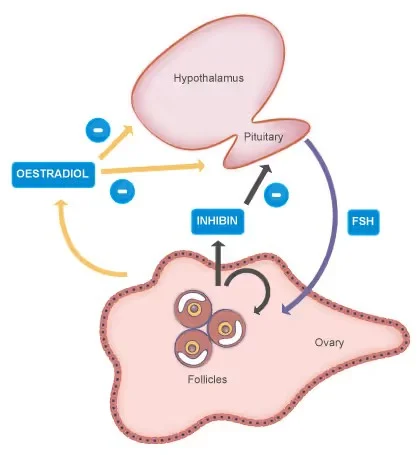
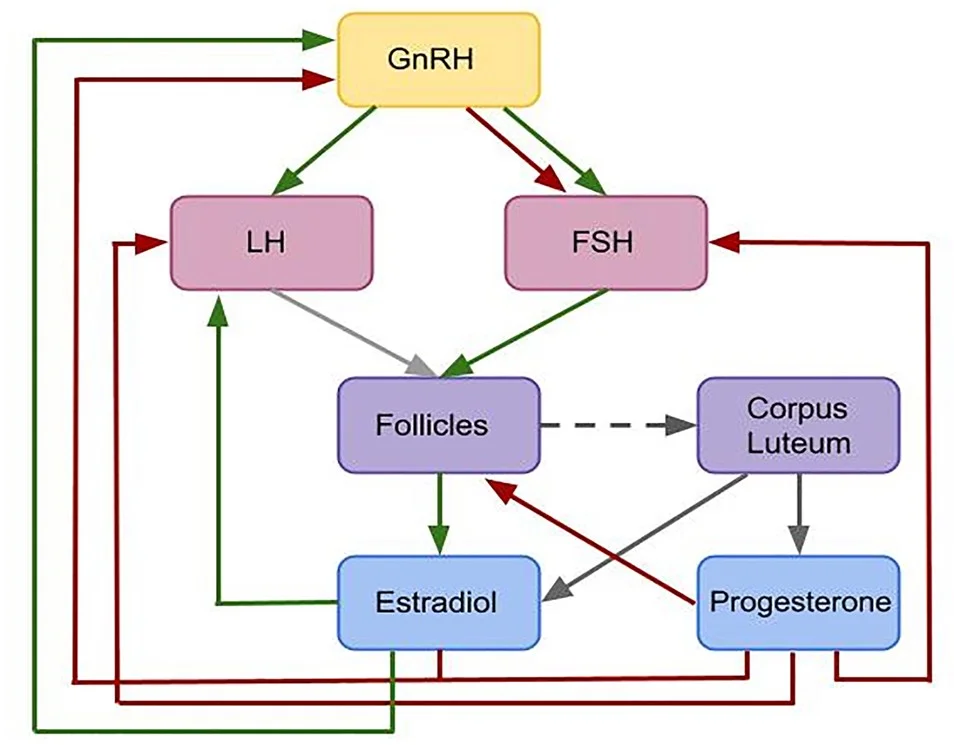
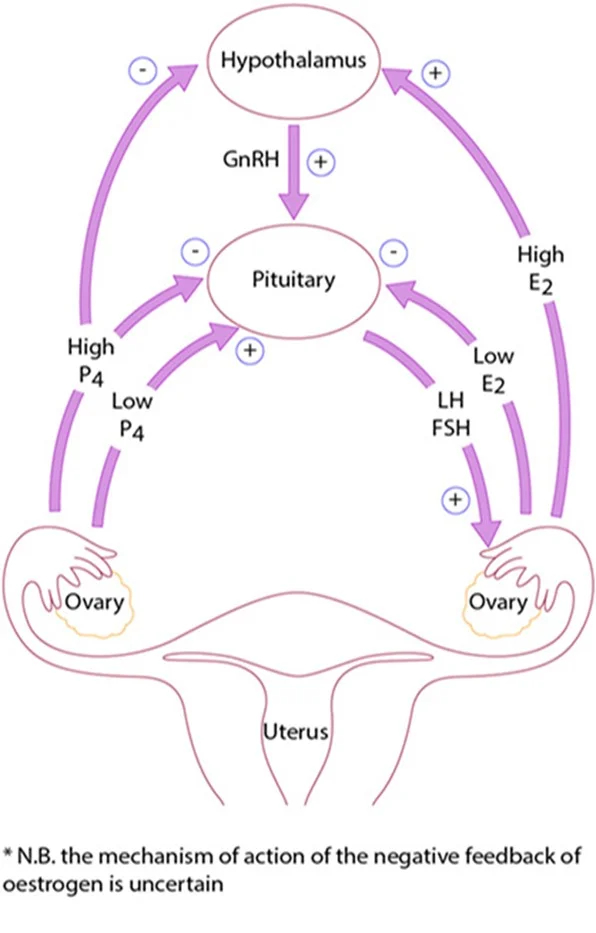
Hypothalamus-Pituitary-Ovary-Uterus Feedback Loop
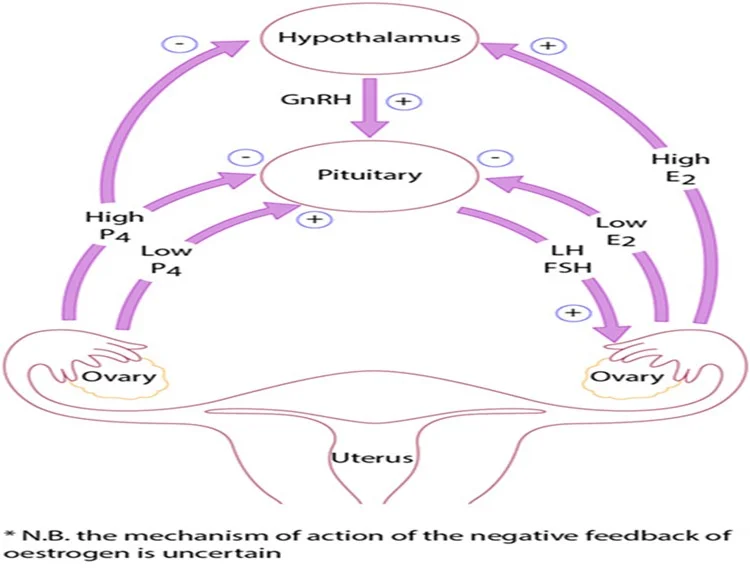
- N.B. the mechanism of action of the negative feedback of oestrogen is uncertain
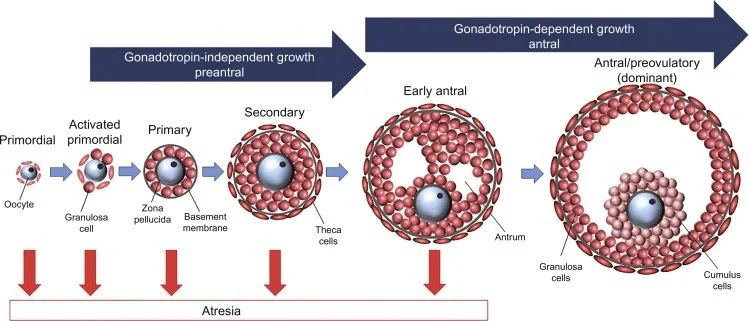
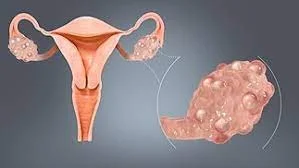
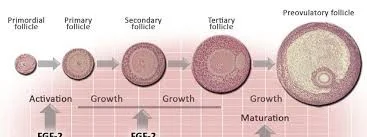
Initial Stages of Follicular Development
Gonadotropin-Independent Growth
The initial stages of follicular development are independent of hormone stimulation.
- Follicular development will fail at the preantral stage and follicular atresia will ensue if pituitary hormones LH and FSH are absent.
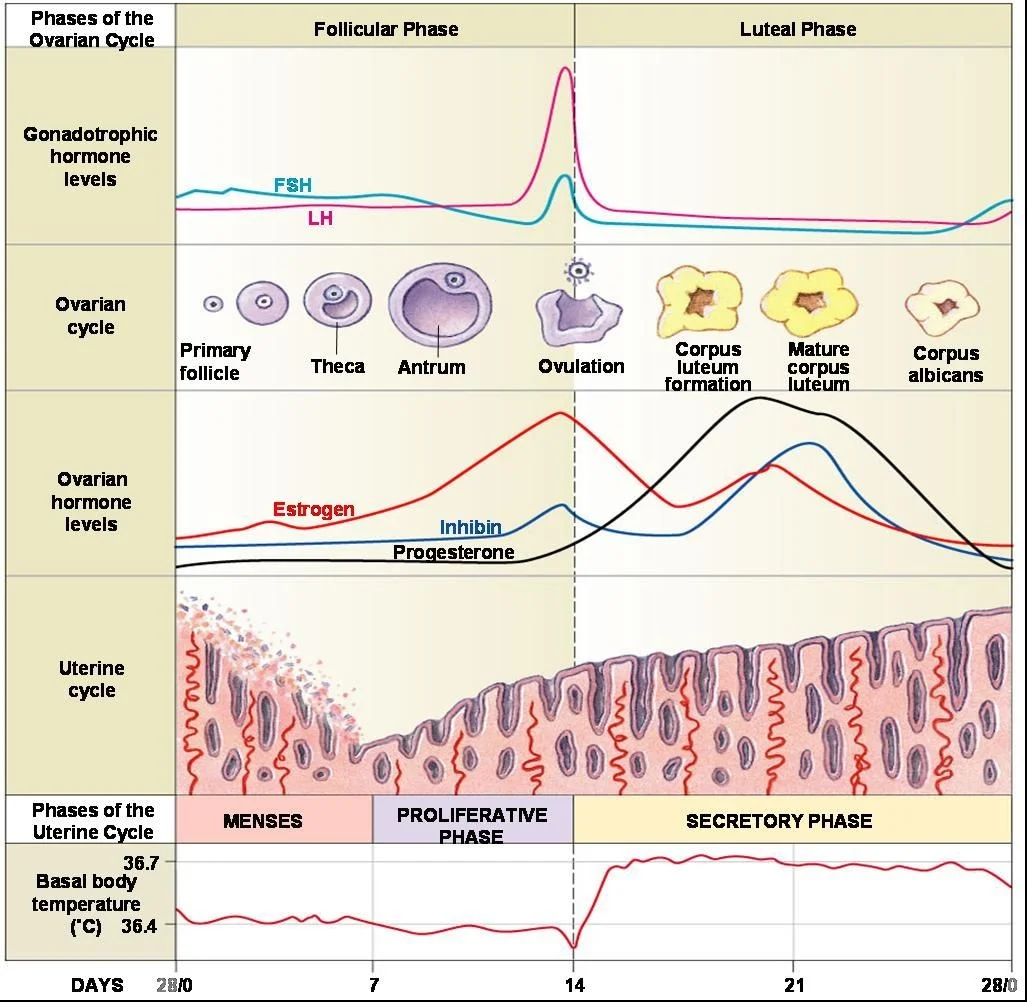
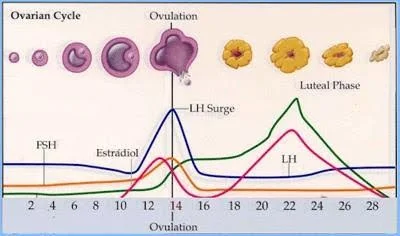
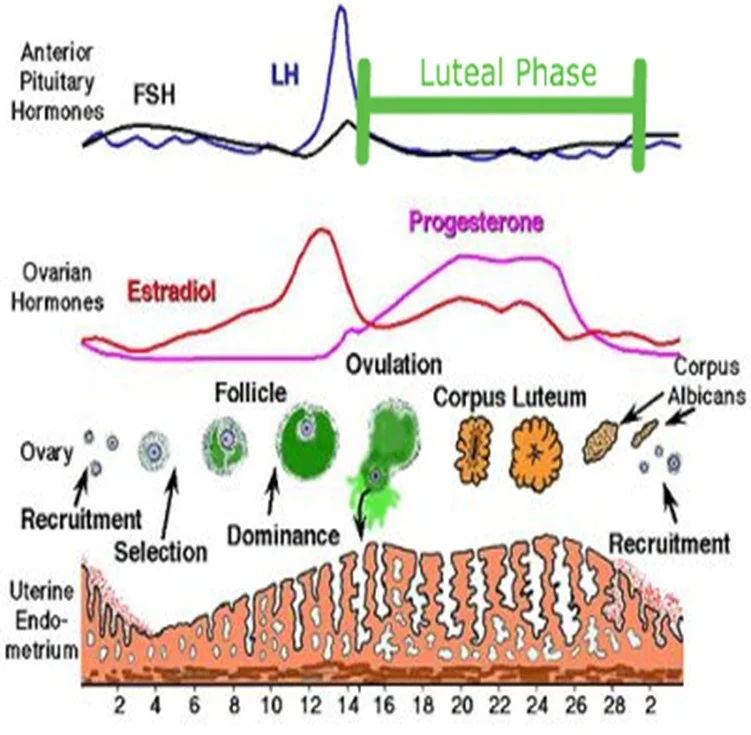
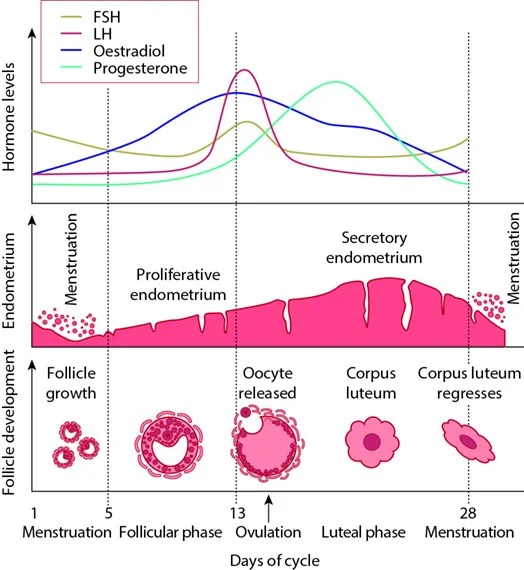
- ➢FSH levels rise in the first days of the menstrual cycle, when oestrogen, progesterone and inhibin levels are low.
- • This stimulates a cohort of small antral follicles on the ovaries to grow.
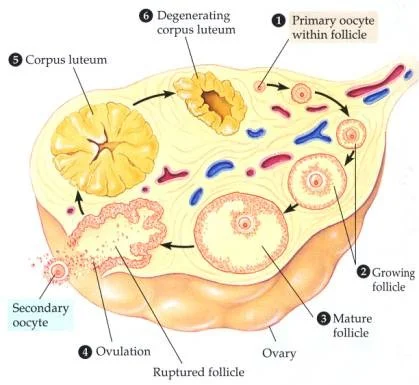
Follicle Development Stages
Follicular and Luteal Phases Visual Overview


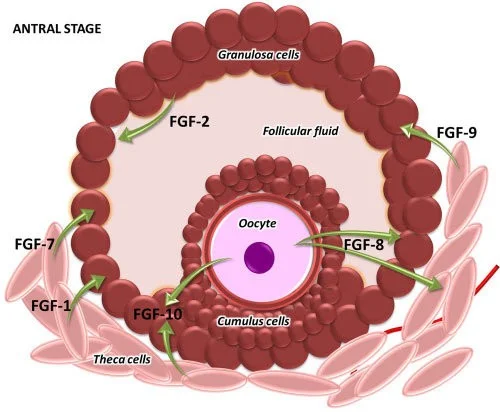
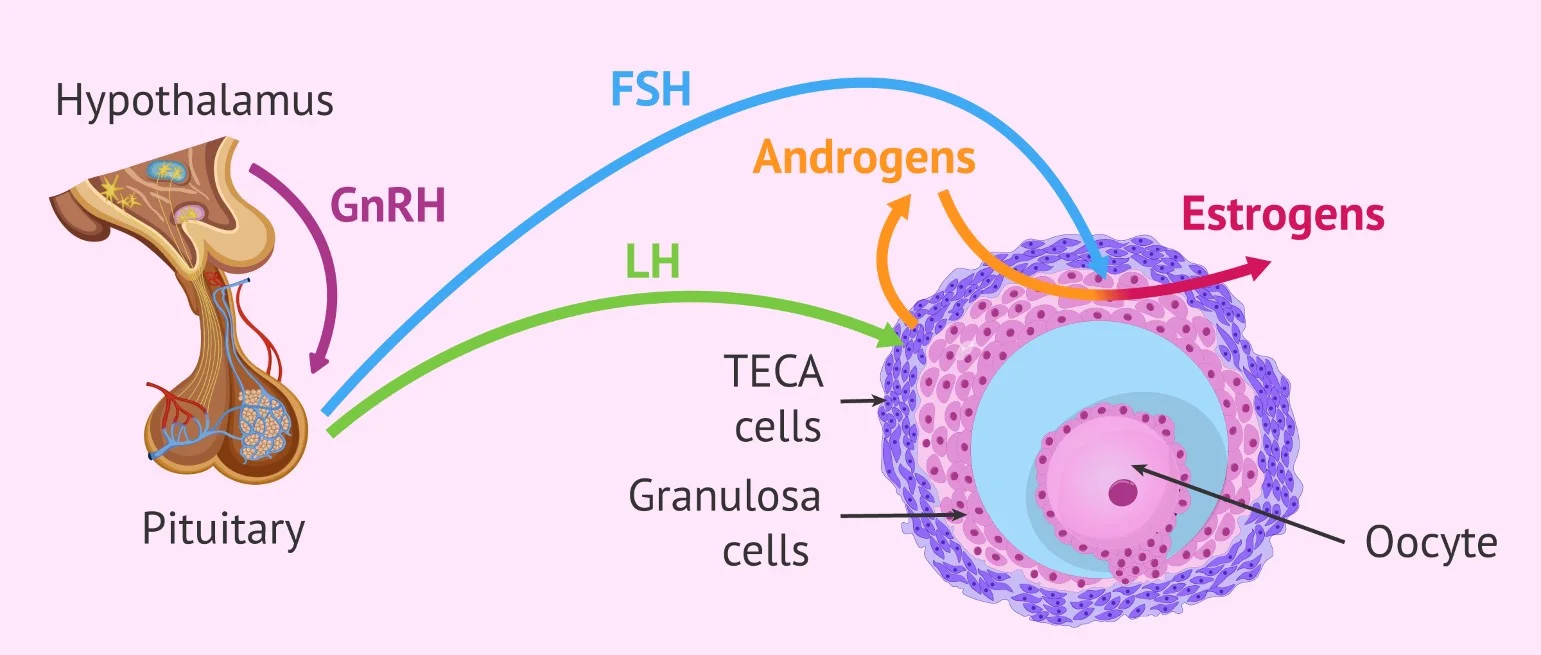
Cellular Interactions in Follicle Steroid Production
- Within the follicles, there are two cell types that are involved in the processing of steroids, including oestrogen and progesterone.
- These are the theca and the granulosa cells, which respond to LH and FSH stimulation, respectively. Z
- Theca cells ➡️ LH stimulates Progesterone.
- Granulosa cells ➡️ FSH stimulates Oestrogen.
Androgen and Estrogen Synthesis
LH stimulates production of androgens (from cholesterol) within theca cells. …These androgens are converted into oestrogen in granulosa cells, under the influence of FSH.
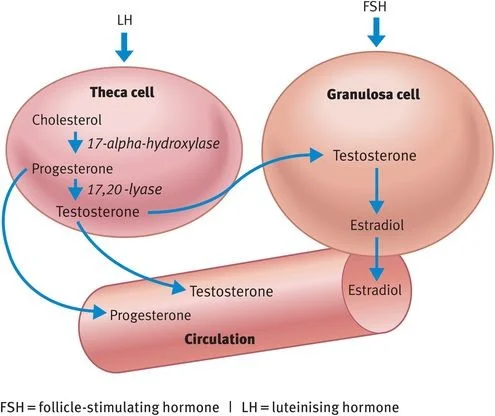 FSH = follicle-stimulating hormone | LH = luteinising hormone
FSH = follicle-stimulating hormone | LH = luteinising hormone
Follicle Growth and Feedback
As the follicles grow, oestrogen secretion increases, leading to negative feedback (on the pituitary) which causes a decrease in FSH secretion. (This assists in selection of the dominant follicle while smaller follicles will undergo atresia).
Follicle Maturation and Hormonal Influence
Hormonal Interactions
Regulation of Ovarian Hormones
- Inhibin is secreted by granulosa cells, enhancing androgen synthesis.
- Activin is secreted by granulosa cells (is structurally similar to inhibin, but has an opposite action), increasing FSH binding on the follicles.
- Insulin-like growth factors (IGF-I, IGF-II): highest levels found in the dominant follicle fluid towards ovulation.
- Kisspeptins: proteins recently found to play a role in regulation of the HPO axis, mediated in metabolism of leptin.
- Leptin (affect hypothalamus) plays a role in energy production, weight and reproductive health.
- ” Mutations in the kisspeptin receptors associated with delayed or absent puberty”.
Summary of Hormone Feedback and Cellular Action

Ovulation
At the end of the follicular phase (which lasts an average of 14 days), the dominant follicle has grown to approximately 20 mm (mature follicle).
- ✓FSH induces LH receptors on the granulosa cells.
- ✓ Oestrogen increases until making a positive feedback effect on the pituitary.
- ✓LH surge (24–36 hours later).
- ✓ Progesterone from the mature follicle provides feedback for secretion, causing a small periovulatory rise in FSH.
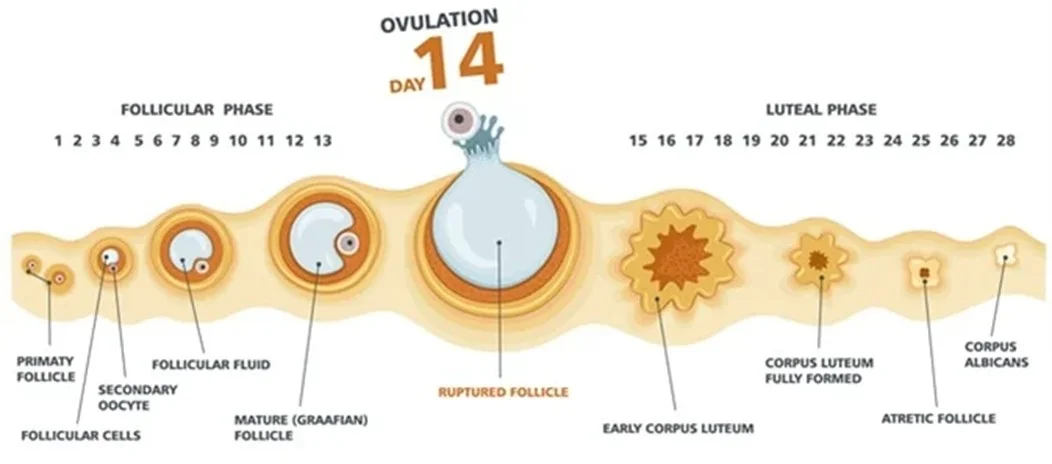
Mechanism of Ovulation
Ovulation occurs after breakdown of the follicular wall. The LH surge is a predictor of ovulation. This process is under the influence of LH, FSH, and proteolytic enzymes (prostaglandins PGs). Inhibition of PG production may result in failure of ovulation. Thus, women wishing to become pregnant advised to avoid taking PG synthetase inhibitors, such as aspirin and ibuprofen.
Luteal Phase
- ✓After release of oocyte, the remaining granulosa and theca cells form the corpus luteum (CL) (due to accumulated yellow pigment).
- ✓Why? To supply granulosa cells with rich blood for steroidogenesis.
- ✓Progesterone stabilizes the endometrium in preparation for pregnancy.
- ✓High Progesterone levels suppress FSH and LH, which prevent another follicular growth.
- ✓The luteal phase lasts 14 days in most women; it is relatively constant in all women.
- ✓In the absence of βhCG (pregnancy), the CL will regress (luteolysis), leading to progesterone withdrawal, and shedding of the endometrium and menstruation.
Corpus Luteum Formation and Regression

Cycle Renewal and Hormone Feedback
- Reduction in levels of progesterone, oestrogen and inhibin feeding back to the pituitary cause increased secretion of gonadotrophic hormones.
- New preantral follicles begin to be stimulated and the cycle begins again.
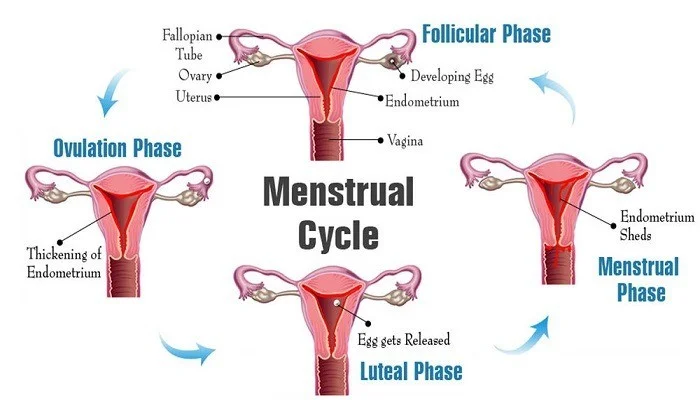
Phases of the Woman’s Cycle

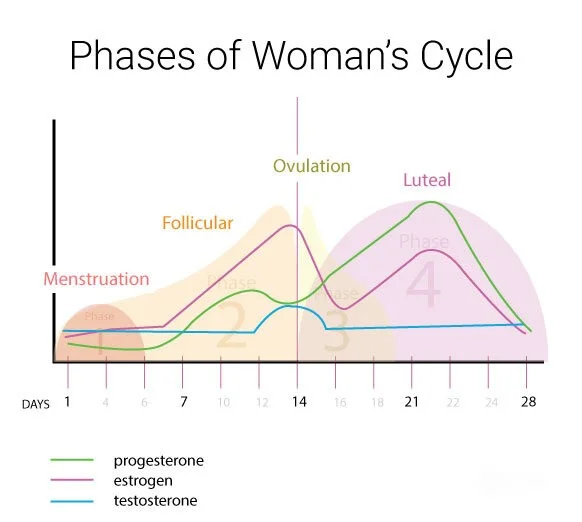
Menstruation
Menstruation (day 1) is the
- shedding of the ‘dead’ endometrium and ceases as the endometrium regenerates (which normally happens by day 5–6 of the cycle).
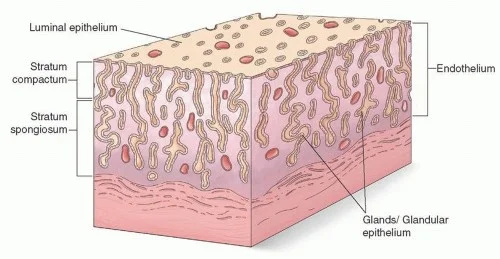
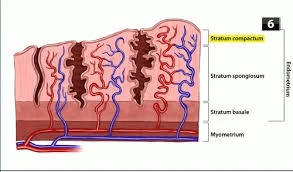
- Immediately prior to menstruation, three layers of endometrium can be seen.
- The basalis is the lower 25% of the endometrium, which will remain throughout menstruation and shows few changes during the menstrual cycle.
- The midportion is the stratum spongiosum with oedematous stroma and exhausted glands. The superficial portion (upper 25%) is the stratum compactum with prominent decidualized stromal cells.
Physiological Mechanism of Menstruation
A fall in circulating levels of oestrogen and progesterone 14 days after ovulation leads to loss of tissue fluid, vasoconstriction of spiral arterioles and distal ischaemia. This results in tissue breakdown and loss of the upper layers, along with bleeding from fragments of the remaining arterioles, seen as menstrual bleeding. Enhanced fibrinolysis reduces clotting. (This effect can be reproduced artificially, for example in patients taking the COCP).
Vaginal bleeding will cease after 5–10 days as arterioles vasoconstrict and the endometrium begins to regenerate.
- Haemostasis in the uterine endometrium is different from elsewhere in the body (no clot formation and no fibrosis).
Endometrial Repair
NOTE Endometrial repair involves:
- both glandular and stromal regeneration
- and angiogenesis
- to
- reconstitute the endometrial vasculature.

The Endometrium
- The hormone changes effected by the HPO axis during the menstrual cycle will occur whether the uterus is present or not.
- The changes in the endometrium give the most obvious external sign of a regular cycle.
The Proliferative Phase
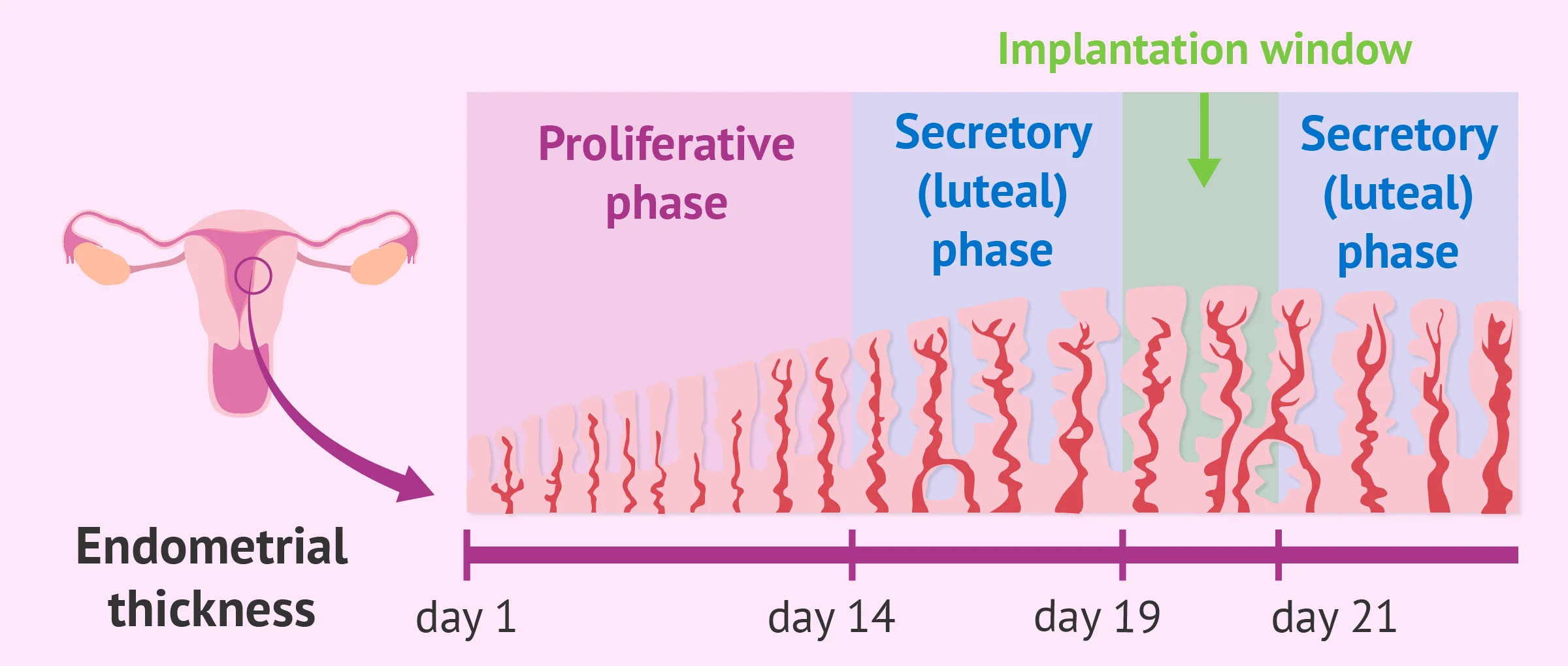
After menstruation, when glandular and stromal growth begin. The epithelium lining the endometrial glands cells increase by mitoses. Endometrial thickness increases from 0.5 mm to 3.5–5 mm at the end of the proliferative phase.
The Secretory Phase
- After ovulation (around day 14)
- there is a period of endometrial glandular secretory activity.
- Endometrial thickness does not increase any further.
- The glands will become more tortuous.
- Spiral arteries will grow.
- Fluid is secreted into uterine lumen.
- Later, formation of a temporary layer, known as the decidua, in the endometrial stroma.
Endometrial Receptivity
After day 21–22, a progesterone-dependent stage making the endometrium receptive for embryo implantation.
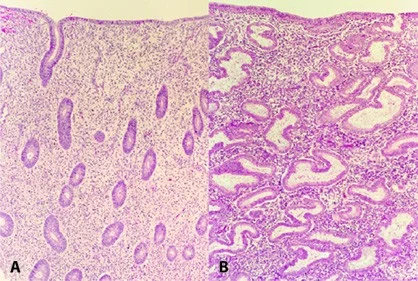
Endometrial Tissue Sections
- (A)proliferative phase.
- (B)secretory phases Of the menstrual cycle