Miscarriage
By dr Mona Ahmed


LEARNING OBJECTIVES
- Understand the social and emotional context of early pregnancy loss.
- Understand why a high suspicion of pregnancy is needed in all women of reproductive age with symptoms.
- Obtain a detailed knowledge of the clinical presentation and management of miscarriage and ectopic pregnancy.
- Obtain an awareness of less common early pregnancy conditions, including recurrent miscarriage, gestational trophoblastic disease and hyperemesis gravidarum.




Miscarriage
is a pregnancy that ends spontaneously before 24 weeks’ gestation or (or before viability).
- What is viability? More than 24 weeks of gestation or more than 500 gms.

Incidence:
15 - 20% of pregnancies.
Classification:
- Spontaneous miscarriage: occurs without medical or mechanical.
- induced abortion
![]()
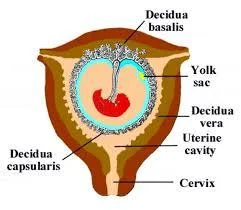
Pathophysiology
Haemorrhage into the decidua basalis lead to:
A. Necrotic changes in the tissue adjacent to the bleeding. B. Detachment of the conceptus. C. The above will stimulate uterine contractions resulting In expulsion.
RISK FACTOR
- Maternal age - more than 35years.
- Increased gravidity.
- Previous history of miscarriage.
- Multiple pregnancy
Causes of miscarriage
Fetal causes & maternal causes
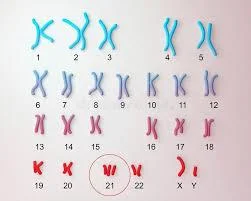
Fetal causes:
- Chromosomal e.g. Trisomy.
- Structural e.g. Neural tube defect.
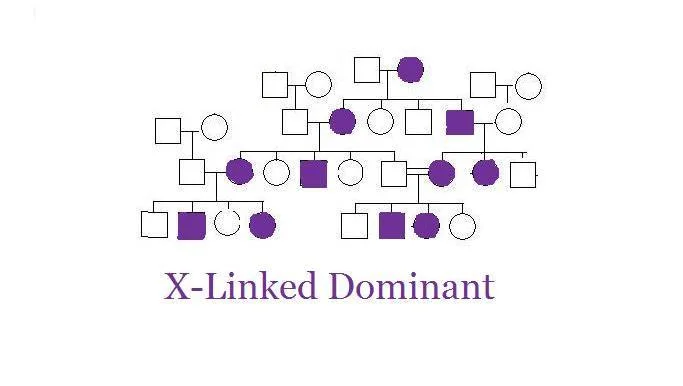
- Genetic e.g. X- Linked diseases

Maternal causes:
Immunological:
- Autoimmune diseases :APL.
uterine abnormality:
- septate uterus & cervical incompetence.Z
Endocrine :
Infections (maternal/fetal):
- as TORCH infections.
- listeria
Environmental toxins:
- alcohol.
- Smoking.
- drug abuse.
- ionizing radiation.

Clinical presentation
- The most common sign of miscarriage is vaginal bleeding.
- Abdominal pain.
- Hypovolemic shock.
- Expulsion of products of conception.
- A symptomatic.
- Each type has its own symptoms
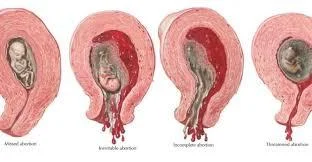
TYPES
MISCARRIAGE
- Threatened Miscarriage
- Incomplete Miscarriage
- Inevitable Miscarriage
- Missed Miscarriage
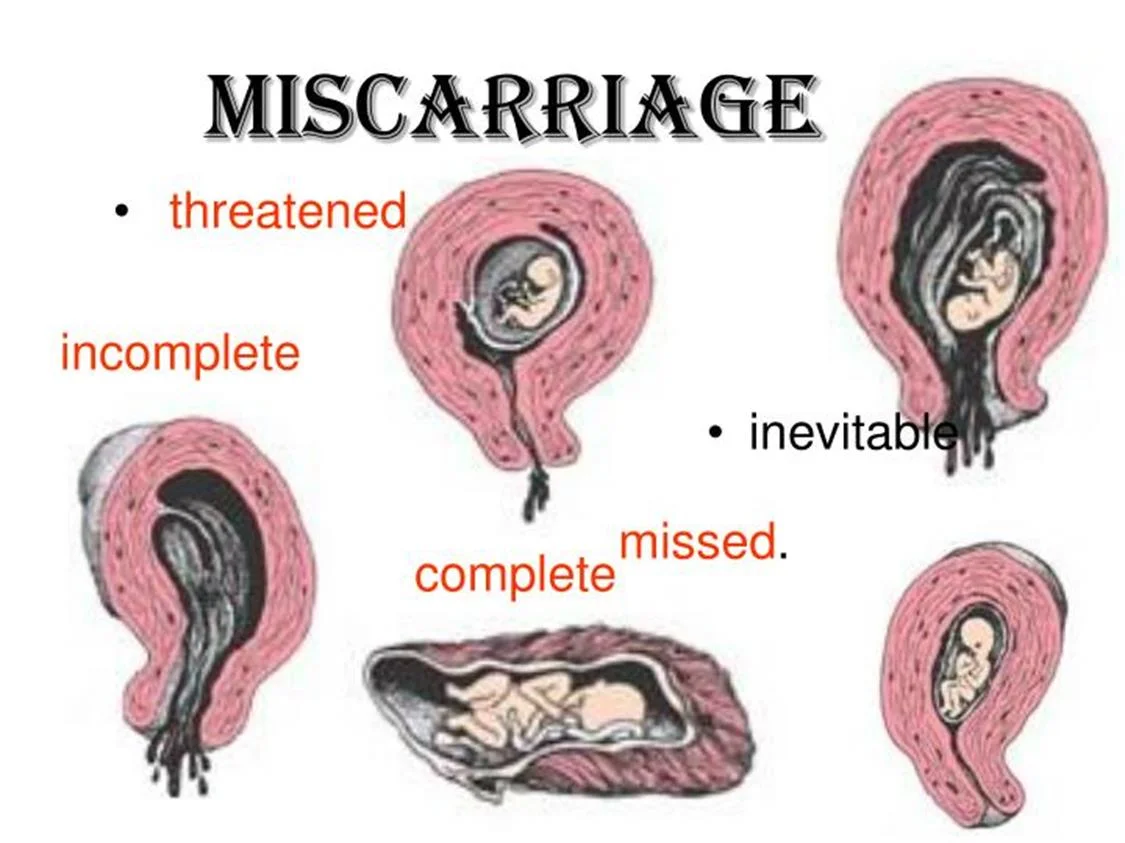
Threatened miscarriage
-
Clinical feature:
- Amenorrhea.
- Mild bleeding (spotting).
- Mild pain.
-
On examination:
- Uterus corresponding to the date.
- PV: closed cervical os.
-
Investigations:
- Pregnancy test (hCG): +ve.
- US: viable intra uterine fetus.
-
Management:
- reassurance.
- Rest.
- Repeated U/S
- Progesterone support.
THREATENED MISCARRIAGE
~ COMMON & MOSTLY DOES NOT RESULT in a MISCARRIAGE
BLEEDING from CLOSED CERVIX


Inevitable miscarriage
-
Clinical feature:
- Amenorrhea.
- heavy bleeding accompanied with clots (may lead to shock).
- Severe lower abdominal pain.
- On examination:
- P.V.: opened cervical os + product inside the cervical canal.
-
Management:
- I.V fluids.
- Blood if need.
- Digital evacuation if possible.
- Ergometrine & syntocenon.
- evacuation of the uterus (medical/surgical).
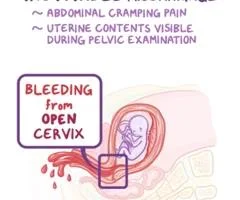

Incomplete Miscarriage
Clinical feature:
- Partial expulsion of products
- Bleeding
- colicky pain continue.
On examination:
- P.V.: opened cervix.
- retained products may be felt through it.
Investigations:
- US: retained products of conception.
Treatment :
- Medical or surgical.
- Surgical evacuation.
- Medical evacuation(prostaglandins , syntocenon).


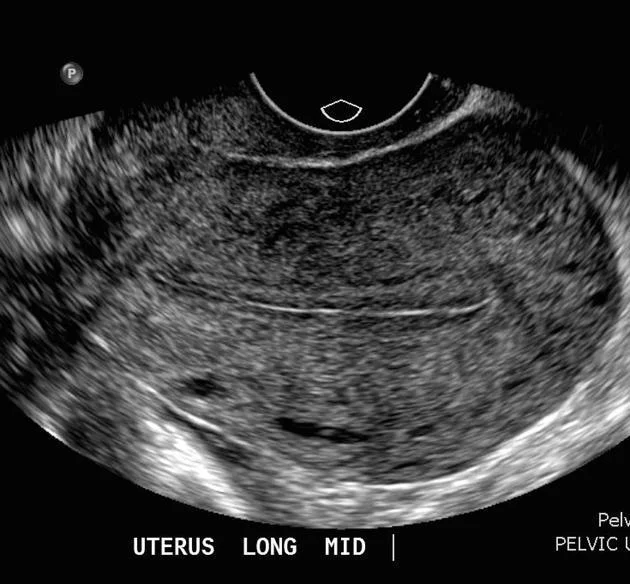
Complete miscarriage
- Clinical feature:
- Expulsion of all products of conception.
- Cessation of bleeding and abdominal pain.
- on examination:
- P.V.: closed cervix.
- Investigations:
- US: empty uterus.
- Treatment:
- Supportive.

Missed miscarriage
-
Clinical feature:
- gradual disappearance of pregnancy Symptoms Signs.
- Brownish vaginal discharge.
- Milk secretion.
-
Investigations:
- Pregnancy test: negative( but it may be + ve).
- US: absent fetal heart pulsations.
-
Complications :
- Hypofibrinogenemia .
- Infection.
- DIC
-
Treatment :
- conservative: Wait 4 weeks for spontaneous expulsion -
- Surgical:( D&C) if Spontaneous expulsion does not occur after 4 weeks. Or if it’s the choice of the pt .
- Medical: PGs.
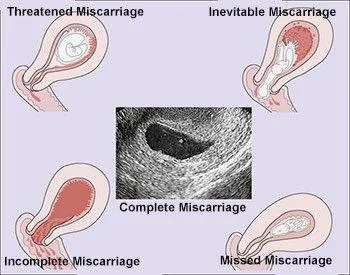
Types of miscarriages with ultrasound findings and clinical presentation
| Type of miscarriage | Ultrasound scan (USS) findings | Clinical presentation | Management |
|---|---|---|---|
| Threatened miscarriage | Intrauterine pregnancy with FH | Vaginal bleeding Abdominal pain Speculum cx os closed | Supportive |
| Inevitable miscarriage | Intrauterine pregnancy (with no FH) | Vaginal bleeding Abdominal pain Speculum cx os open | Expectant medical or surgical |
| Incomplete miscarriage | RPOC | Vaginal bleeding Abdominal pain Speculum cx os opened Retained products found in the os | Remove RPOC if possible at time of examination(speculum) Expectant medical or surgical |
| Complete miscarriage | Empty uterus Serum h CG to exclude EP (If no previous one with intrauterine pregnancy ) | Vaginal bleeding & Abdominal pain resolved Speculum cx os closed | Supportive |
| Missed miscarriage | IUP No FH | A symptomatic often diagnosed at booking UUS | Expectant medical or surgical |
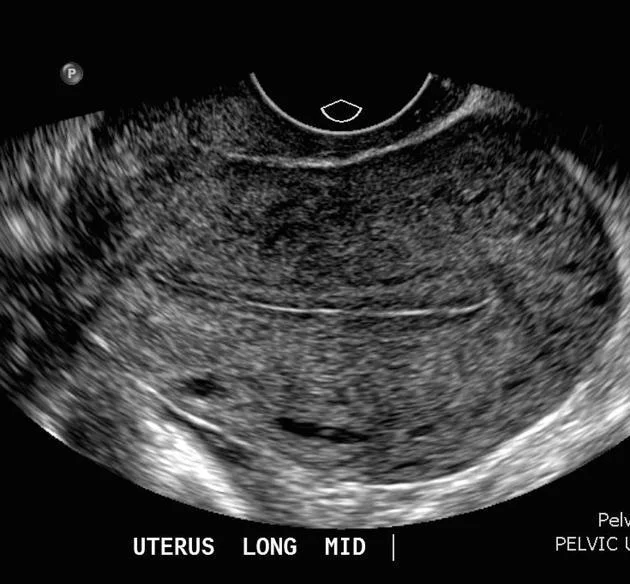
Investigations
- Transabdominal/TVUSS:
- a single ultrasound scan can diagnose a miscarriage if there is a pregnancy within the uterine cavity.
- Haemoglobin and ‘Group and Save’ (or cross-match if patient is severely compromised):
- Assess degree of vaginal loss and rhesus status.
Management
- expectant
- medical
- surgical
- approach depending on clinical presentation and patient choice
- Expectant management
- To avoid surgery
- urinary pregnancy test after 3 weeks and it is positive
- let pt come again She may need surgical treatment if she start to bleed heavily.
- Expectant management
Medical management
- Used in outpatient setting
- allow women to miscarry at home. It involves
- prostaglandin E analogue (misoprostol).
- progesterone antagonist (mifepristone)(if >9wks’).
The side-effects include:
- Pain.
- Vomiting
- Diarrhoea.
- women are routinely provided with pain relief and antiemetics). post-treatment pregnancy test is recommended
Women may need surgical treatment if medical treatment fail.

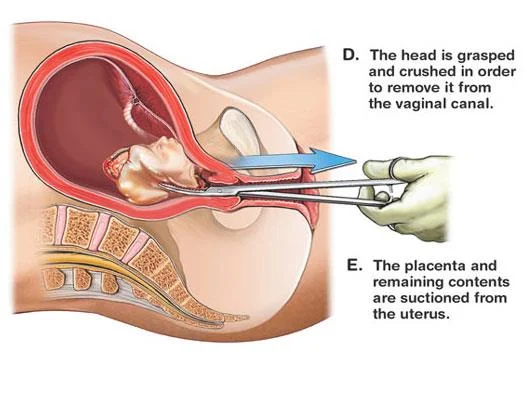
Surgical management
-
if there is:
- persistent excessive bleeding.
- haemodynamic instability.
- if women favour it.
-
It can be done by Surgical evacuation.
-
Evacuation risks:
- uterine perforation.
- postoperative pelvic infection.
- cervical trauma and subsequent cervical incompetence.Z
D. The head is grasped and crushed in order to remove it from the vaginal canal.
E. The placenta and remaining contents are suctioned from the uterus.
Recurrent miscarriage
Definition:
Loss of three or more consecutive pregnancies.
Incidence:
- 1% of pregnancies.
Risk factors:
- Advancing maternal and paternal age.
- Obesity.
- Balanced chromosomal translocations.
- Congenital abnormalities.
- Uterine structural anomalies and cervical incompetence.Z
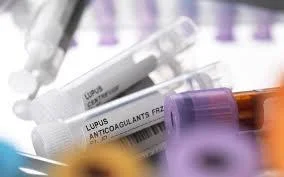
- Antiphospholipid syndrome (APS). Z
LMW

Investigations
- testing for antiphospholipid antibodies
- imaging of the uterus.
- Products of conception should be sent for cytogenetic analysis to detect chromosomal abnormality.
- peripheral blood karyotyping of both partners should be performed.
Most couples have normal investigations
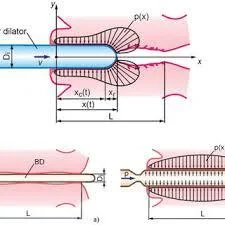
Diagnosis of cervical incompetence:Z
-
From history
- Three or more miscarriage es.
- Painless vaginal bleeding.
- decreased gestational age in subsequent pregnancy.
-
From investigations:
- Hagar dilator(No.8).
- HSG.
- During pregnancy: US Funnel shape, short cervix.
Management:
- Cervical cerclage.

SEPTIC MISCARRIAGE
- Following an incomplete miscarriage due to ascending infection.
- Or following criminal abortion.
- Clinical picture: -
- Symptoms:
- Offensive bloody vaginal discharge.
- Increased body temperature.
- Lower abdominal pain (pelvic peritonitis)
- generalized peritonitis.
- Signs:
- Increased pulse rate.
- Dehydration.
- toxicity.
- Symptoms:
- Clinical picture: -

Investigations:
- Blood.
- FBC.
- BHCG.
- Renal profile.(2ry to septic shock).
- Blood grouping & cross matching.
- ESR.
- High vaginal swab for C/S.
- Blood culture & sensitivity(if needed).
Treatment:
- Antibiotic.
- iv fluids.
- blood transfusion.
- Evacuation of retained product.
SEPTIC SHOCK
- Tachypnea Tachycardia
- Hypotension Hypothermia
- Oliguria
- Sepsis
- Multi organ failure
Anti-D administration
- All rhesus-negative women who have a surgical procedure to manage an EP or miscarriage should be offered anti-D immunoglobulin.
- Anti-D is not required for
- Threatened miscarriage.
- complete miscarriage.
- medical management of miscarriage or EP.
- but guidelines differ, and prophylaxis is often given

Notes
In all form of miscarriages: general clinical assessment should be made:
- vital signs.
- abdominal examination.
- vaginal examination.
- All needed investigations +/- ws:
- Send product for histopathology.
- Management should be according to clinical Type & gestational age.
Don’t Forget!!
- Pt emotionally distressed by her physical symptoms & loss of her baby. So
- Support her.
- Explain the causes & reassure her she is not guilty
may also be due hypothyroidism or diabetes for reccurent miscarriage