How to Read Musculoskeletal X-Rays
Prof. Mamoun Kremli | Dr. Tarif Alakhras
Introduction
- X-rays are part of diagnostic tools
- When requesting an X-ray, information given (written) helps in reaching a diagnosis
- Important points in history
- Relevant physical findings
- Age and sex
- Differential diagnosis
- Question(s) to be answered
- Required views should be mentioned
X-ray Request Form
- Name of the institution
- Name of the patient, including UR number, date of birth, gender
- Indicates if the patient is ambulant, arriving in a wheel chair or confined to a bed
- Any allergies applicable to the imaging procedure e.g. allergy to contrast media
- The name of the referring doctor, signature and date of request
- Contact details of referring doctor, in this case an internal pager number is given
- Clinical details of the patient, to enable the radiographer to perform the most beneficial views and information for the radiologist to assist with reporting
- Indicates if previous imaging studies have been performed for this patient at this department, old films are an excellent source of information as they enable you to compare images over time
- What examination has been requested e.g. chest x-ray
- Where is the patient located e.g. Emergency Department
- The head of the department of the referring doctor, often for billing purposes

Reading X-rays: Systematic Approach
- General information
- Reading bone
- Reading joints
- Reading soft tissues
General Information
- Identify patient’s information
- Name, sex, age, file number, date of X-ray
- Anatomical area
- What parts are seen on the film
- View(s)
- AP, Lat., Oblique, Special, …
- X-ray quality
- Extra:
- In full cast, cast slab, splint, traction pin, implants…
How to Read X-Rays
General Guidelines
Prof. Mamoun Kremli
Introduction
- X-rays are part of diagnostic tools
- When requesting an X-ray, Required views should be mentioned,
- ex. AP, lateral, special views
- The written information given helps in reaching a diagnosis
- Age & sex
- ex. limp in DD of tumor
- Important points in history
- ex. patient exposed to trauma, sport or dynamic injury
- Relevant physical findings
- ex. stability of knee, bleeding, wounds, allergy
-
* to the contrast given with X-ray
- Differential diagnosis
- for X-ray to exclude some of them
- Question(s) to be answered
- Age & sex
General Guidelines
- Describe what you see (Normal / abnormal)
- Do not jump to diagnosis ex. first say: x-ray AP view of knee of child
- If you identify one abnormality, keep looking for others!
- Read clearly systematically. Avoid long silence
- Use appropriate terms
- Parts of bone ex. Proximal part of femur
- Alignment (Varus, Valgus)
- Displacement. Rotation
- Compare to: Other view(s). Other side. A previous x-ray don’t depend on AP view only
- When in doubt: Follow the cortex if there is no separation of cortex = no fracture
Reading X-rays
- General information
- Reading bone
- Reading joints
- Reading soft tissues
General Information
- Identify patient’s information
- Name, sex, age, file number, date of X-ray
- Anatomical area
- What bony parts are seen on the film
- View(s)
- AP, Lat., Oblique, Special
- ordered in spine
- AP, Lat., Oblique, Special
- X-ray quality
- be too dark (when giving too much radiation)
- when suspect:
- - spondylolisthesis
- - pars interarticularis defect
- Extra:
- cast. slab, splint, traction pin, implants

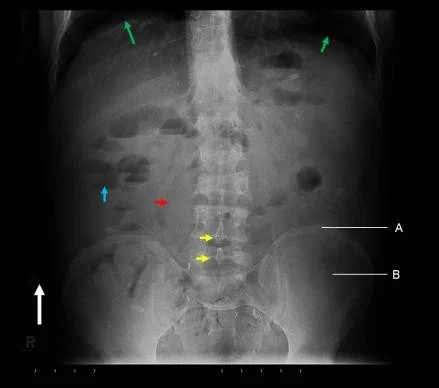
Anatomical Information

- x-ray AP and lateral view of forearm, show a displaced fracture in both radius and ulnar shaft with elbow dislocation
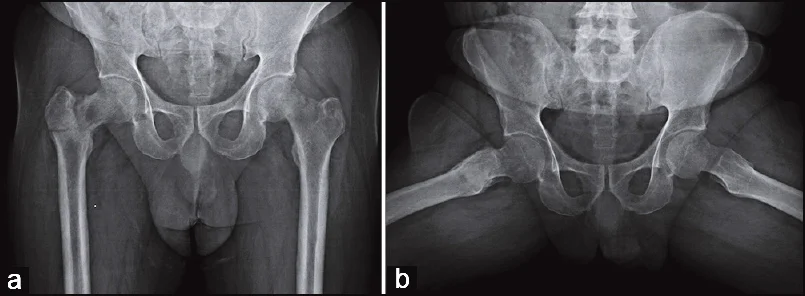

- x-ray of male pelvis and proximal femur, AP view, mature bone fracture in greater trochanter in right side, fracture in neck of femur on left side
View(s) Information
AP, Lat., Oblique, Special

Extra Information
- cast, slab, splint, traction pin, implants
 Cast
Cast

- X-ray AP view of Lt femur, fracture of distal femur with slab, Thomas splint

- X-ray AP view of Rt distal femur, presence of traction pin

- X-ray AP view of Lt femur, fracture in distal femur with plate and screws
Reading The Bone
- Which bone / Which view
- Bone age / quality / shape
- Look for fractures
- Look for lesions / Periosteal reaction
- Use anatomical descriptions
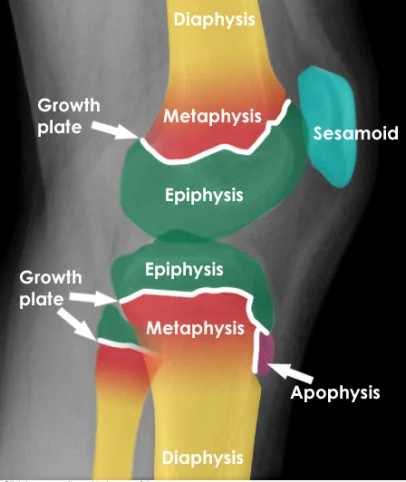
Use Anatomical Description







Annotated Features:
- Diaphysis
- Metaphysis
- Epiphysis
- Growth plate (appears twice)
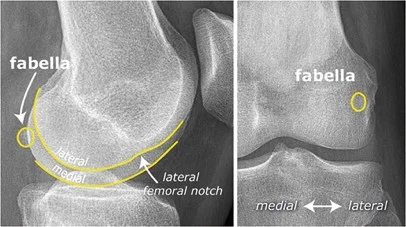
- Patella or Sesamoid bone (bone inside a tendon)
- Apophysis (normal)
Additional Notes:
- If there was calcification in a specific area, it’s called Fabella.

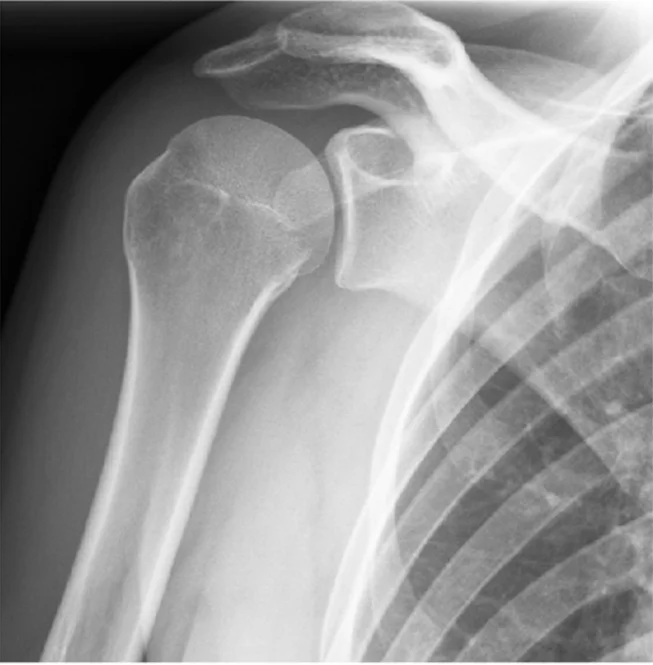
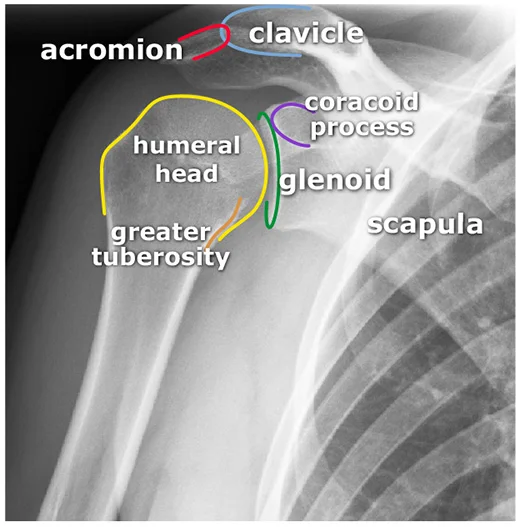
x-ray AP view of Shoulder Joint
- The image contains two X-ray views of a shoulder joint.
- The right X-ray is annotated with labels for various anatomical features.
- acromion
- clavicle
- coracoid process
- humeral head
- glenoid fossa
- greater tuberosity
- scapula
Use Anatomical Description



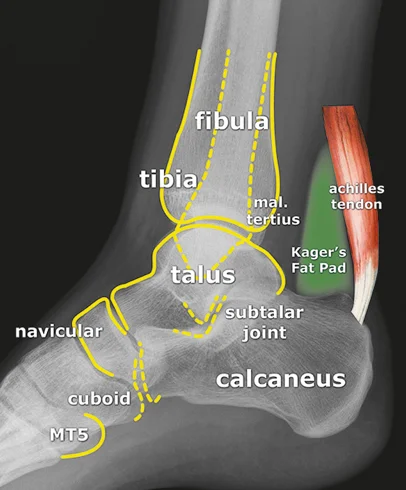
x-ray lat. view of ankle joint
- The image presents two X-ray views of an ankle joint.
- The left image is a plain X-ray.
- The right image is a labeled version of the same X-ray.
Labeled Components:
- Bones:
- tibia
- fibula
- talus
- navicular
- cuboid
- calcaneus
- MT5 (Fifth Metatarsal)
- Other Structures:
- achilles tendon
- Kager’s Fat Pad
- Joints:
- subtalar joint
- Other:
- mal. tertius

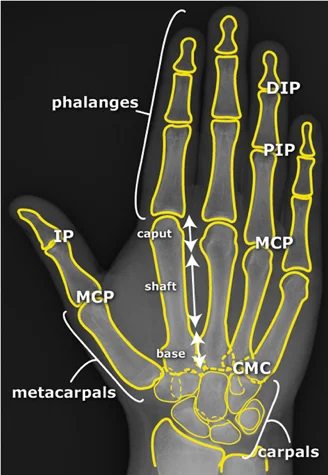
x-ray of hand


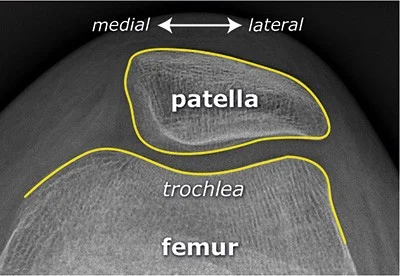
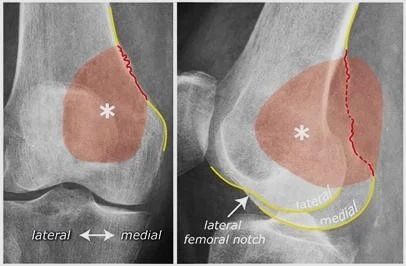
Reading Joints
- Name of joint
- Bone and Joint Alignment
- Position / Relations
- Joint space
- Articular surfaces



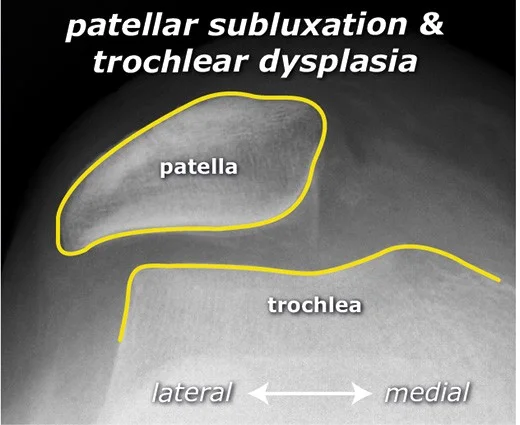
bone alignment

- subluxation of patella

- Anterior dislocation of shoulder joint
Reading Soft Tissue
- Air (open wounds / infection) indicate for
- Calcifications / Fluid
- Muscles / Tendons
- Next to bone / Fat Pad
- Other soft tissue
- Displaced fat pad sign
- By hematoma of fracture

- Air in fractures
- sign of an open fracture


- sign of an open fracture
Reading a fracture
- Site:
- Which bone
- Where in bone
- Metaphysis. Diaphysis. Epiphysis
- Intra/extra-articular
- Head, neck, shaft, Base
- Inter /sub- trochanteric
- Medial/Latera malleolus
- Greater/Lesser trochanter/ tuberosity
- Type
- Fracture line
- Displacements
- Special issues

-
fracture distal fibula
-
pelvis disconounty of cortex indicating fracture in neck of right femur #CC

- X-ray of … CC

- simple fracture of femur
- spiral fracture of tibia

- avulsion of median epicondyle
- communicated butterfly fracture of mid shaft of tibia
- segmental fracture of femur

- wedge fracture of spine
- .
- widening of joint space, indicating depressed fracture
Overview
Reading a fracture involves a systematic approach to understand the nature and severity of the fracture. This includes identifying the site, type, fracture line, displacements, and any special issues related to the fracture.
Key Elements to Identify
Site
- Location of the fracture
Type
- Simple: A single break in the bone
- Comminuted: The bone is broken into multiple pieces
- Other types include spiral, transverse, oblique, and complex fractures
Fracture Line
- Describes the orientation and characteristics of the fracture line
- Oblique
- Transverse
- Vertical
- Spiral
- Complex
Displacements
- Refers to the position of the distal fragment in relation to the proximal fragment
- Shift (medial/lateral, anterior/posterior)
- Tilt (medial/lateral, anterior/posterior)
- Rotation (medial/lateral)
- Overlap/Shortening
- Gaping/Lengthening
- Impaction
Special Issues
- Includes complications or specific conditions associated with the fracture
- Healing: Callus formation or non-union
- Avascular necrosis (AVN)
- Pathological fractures due to weak bone (osteopenia, tumor, cyst)
- Fixation methods (internal: wire, screw, plate, DHS, IM nail, elastic nail; external: splint, external fixator, skeletal traction, cast, slab)

Avulsion fracture of patella

- spiral fracture of humerous
- fracure of medial malleolus
- fracture in distal humerous intracondylar
- fracture of patella
- laterral line fracture of tibial p
 Simple, Spiral
Simple, Spiral
Reading a fracture
Two joints / Two views
- Site
- Type
- Fracture line
- Displacements : distal part in relation to proximal part
- Shift : medial/lateral, anterior/posterior
- Tilt : medial/lateral, anterior/posterior
- Rotation : medial/lateral
- Overlap/shortening, gaping/lengthening
- Impaction : one bone / two bones (forearm fracture/dislocation)
Special issues
- Healing : callus formation / non‑union
- Avascular necrosis
- Pathological conditions
- Weak bone : osteopenia with thin cortex, tumor, cyst
- Fixation
- Internal : wire, screw, plate, DHS, intramedullary nail, elastic nail
- External : splint, external fixator, SK traction, cast, slab

- Displaced fracture of proximal femur with osteolytic lesion

- Talar fracture

- Femoral fracture treated by IMN - fracture
- mature bone adult

- Trauma: evaluate for periosteal reaction (= callus formation).
• Ask whether the patient is an athlete; callus formation in the 2nd metatarsal often indicates a stress fracture.

Follow the Cortex

- x-ray of wrist undisplaced fracture of scaphoid
- In Trauma – “Follow the Cortex” – adjust brightness/contrast to reveal the fracture line.

Do Not Get Distracted!

Reading a fracture — Two joints / Two views
- Site – the anatomical location of the fracture.
- Type – classification (e.g., transverse, oblique, comminuted).
- Fracture line – orientation and pattern of the break.
- Displacements – any shift or angulation of bone fragments.
- Special issues – associated injuries, neuro‑vascular concerns, or atypical findings.
Reading a fracture — when reviewing two joints / two views, concentrate on the following key aspects:
- Site
- Type
- Fracture line
- Displacements
- Special issues
Important to have two views

Reading a fracture

- Site: Shaft tibia – lower 1/3
- Type: Simple
- Fracture line: Transverse
- Displacements: Lateral & posterior shift; minimal medial & anterior tilt
- Special issues: Joint above not visualized

-
Patient: 62‑year‑old man
-
Mechanism of injury: slipped at the carpet edge and fell on an outstretched hand, resulting in wrist pain and swelling
-
Fracture details
- Site: distal radius
- Type: simple, transverse, extra‑articular
- Displacement: dorsal tilt of ~20°
-
Special considerations
- Osteoporosis/penia (reduced bone density)
- Colles’ fracture (classic distal radius fracture pattern)

- Patient: 9‑year‑old girl
- Injury site: lower shaft of the radius and ulna
- Fracture type: incomplete – simple
- Radius: green‑stick fracture, tilted ≈ 38° radially
- Ulna: torus fracture, tilted ≈ 40° dorsally
- Displacement: notable radial and dorsal tilts of the radius
- Management: requires closed reduction followed by casting
Key point: the combined tilt (≈ 38° radially, 40° dorsally) makes prompt reduction essential.
 A 6‑year‑old fell off a tricycle and presented with pain in the lower forearm.
A 6‑year‑old fell off a tricycle and presented with pain in the lower forearm.
- Site: lower radius
- Fracture type: torus/buckle
- Fracture line: transverse
- Displacement: none
- Management: treated conservatively with a slab

- 12‑year‑old boy fell while playing football.
- Site: upper shaft of the right humerus
- Type: simple fracture
- Fracture line: short oblique, “eaten” fracture line
- Displacement: lateral tilt ≈ 20° with a slight medial shift
- Special issue: pathological fracture in a bone cyst

- Patient: 11‑year‑old with open trauma, 3 weeks in traction
- Site: Mid‑shaft femur
- Type: Simple
- Fracture line: Transverse
- Displacements: Medial angulation tilt 20°; posterior shift/overlap (shortening)
- Special issues: Callus present
 Site – mid‑shaft forearm
Site – mid‑shaft forearm
Fracture type – simple radius & ulna
Fracture line – transverse across both bones
Displacement – 90° rotation of radius & ulna
Imaging – one joint captured in an AP view, the other in a lateral view on the same film
Special considerations – accurate anatomical reduction and absolute stability (a joint) are essential; note that Theddy‑Slongo principles may not apply to forearm fractures.
Review the fracture lines carefully.
 Site: mid‑shaft forearm
Site: mid‑shaft forearm
Type: simple radius / simple ulna fracture
Fracture line: transverse across both radius and ulna
Displacements:
- 90° rotation of both bones
- 35° posterior tilt of both bones
Special issues:
- Requires accurate anatomical reduction and absolute stability (a joint)
Note: The Slongo technique may not apply to forearm fractures; always verify fracture lines.

- Site: mid‑shaft left femur
- Type: simple
- Fracture line: short oblique
- Displacements: medial shift with overlap
- Special issues: hematoma
- Knee joint: not seen
- View: no lateral view
Compare with Previous Image
 Patient: 46‑year‑old lady
Patient: 46‑year‑old lady
Incident: Fell two steps down the stairs and is now unable to stand.
Oncologic history: Breast carcinoma previously treated with chemotherapy and radiotherapy.
Fracture details
- Site: Upper shaft of the femur
- Type: Simple fracture
- Fracture line: Oblique crossing a lytic lesion – appears atypical
- Displacement: Medial shift with some overlap
- Special considerations: Pathological fracture related to metastatic disease
 46‑year‑old woman who slipped two steps down the stairs and was unable to stand.
46‑year‑old woman who slipped two steps down the stairs and was unable to stand.
She has a history of breast carcinoma treated with chemotherapy and radiotherapy.
Fracture details
- Location: Upper shaft of the femur
- Type: Simple fracture
- Fracture line: Strange? (unusual pattern)
- Displacements:
- Medial shift
- Overlap
Special considerations: Pathological fracture (related to underlying disease).
Reading a fracture
 Patient: 58‑year‑old woman who fell at home and now has right‑hip pain with inability to walk.
Patient: 58‑year‑old woman who fell at home and now has right‑hip pain with inability to walk.
Site – neck of the right femur (intra‑capsular).
Fracture type – simple, transverse line.
Displacement – varus, with the femoral head angled downward.
Special concerns – high risk of avascular necrosis (AVN) because the fracture is intra‑capsular.

Patient: 17‑year‑old male – fell from a bicycle, landing on his left shoulder.
Symptoms: Pain on shoulder movement; tender point medial to the shoulder; no skin lesions.
Imaging (X‑ray, left side)
- Location: Middle third of the left clavicle
- Fracture type: Simple
- Fracture line: Transverse
- Displacement: Downward tilt of ≈ 35°
Special considerations: The fracture could be managed conservatively.

- Site: Greater tuberosity of the right humerus
- Type: Simple
- Fracture line: Vertical
- Displacements: None
- Special issues: Can be treated conservatively

Patient: 65‑year‑old woman – slipped on a wet floor and fell onto her left shoulder.
Findings
- Site: upper humeral neck
- Type: comminuted fracture
- Fracture line: multiple (3‑part)
- Displacement: minimal
- Special issues: treated conservatively

A 28‑year‑old runner presented with foot pain, without any history of trauma.
- Site: upper shaft of the 3rd metatarsal
- Type: simple
- Fracture line: transverse
- Displacement: none
- Special issues: callus formation – healing attempt (consistent with a stress fracture)

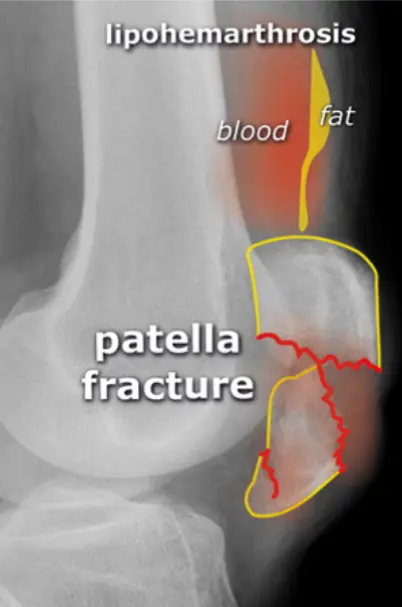
- Site: Supracondylar humerus
- Type: Simple
- Fracture line: Transverse extra‑articular
- Displacements: Posterior tilt
- Special issues: Displaced fat pad sign

- Site: Olecranon
- Type: Simple
- Fracture line: short oblique, intra‑articular
- Displacements: pulled and tilted backwards by the triceps muscle
- Special issues: requires open anatomical reduction and internal fixation with absolute stability
- Site: Radial neck
- Type: Complete, simple
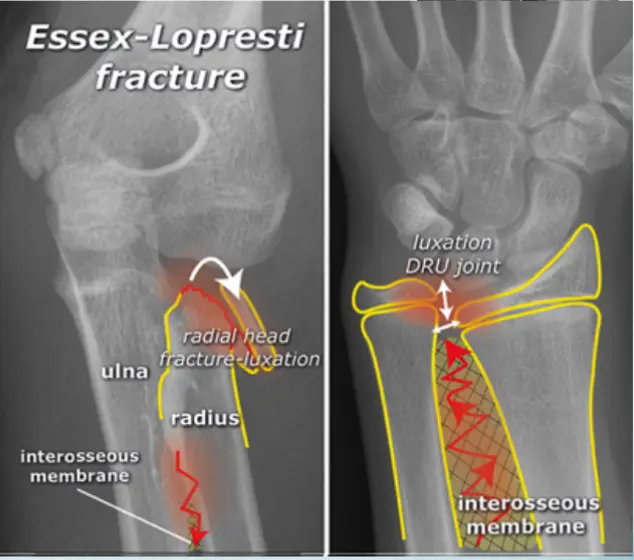
- Fracture line: Transverse
- Displacement: Displaced, tilted laterally (~90°)
- Special issues: Distal radioulnar joint separation – unstable (interosseous‑membrane rupture); managed with ORIF

12‑year‑old boy injured in a motor‑vehicle accident
- Site: mid‑shaft femur
- Fracture type: simple
- Fracture line: transverse
- Displacements: medial shift & tilt, posterior shift, overlap
- Special issues: *considered

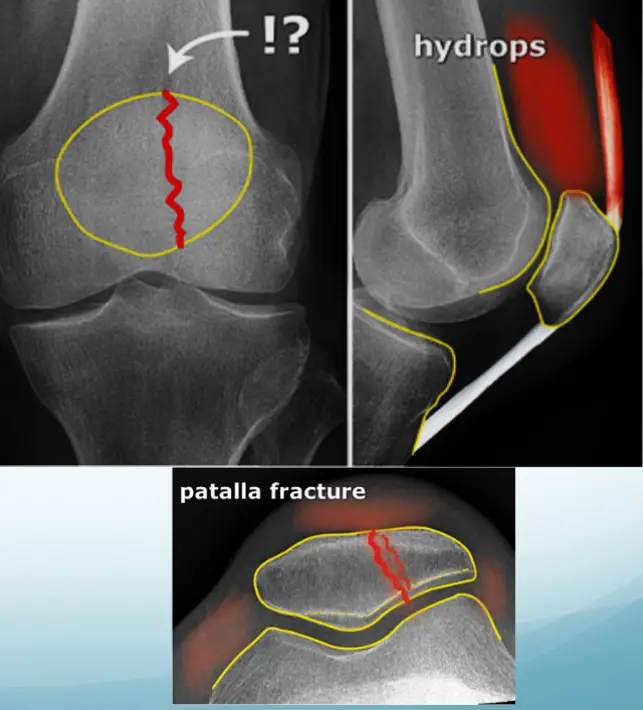
Patient – 40‑year‑old female
Mechanism – Jumped from the 2nd floor
Presentation – Pain and swelling around the right knee
Site – Lateral tibial plateau
Type – Simple
Fracture line – Vertical split
Intra‑articular – Yes
Displacements – Small gap in the articular surface
Special issues – Requires surgery for absolute stability
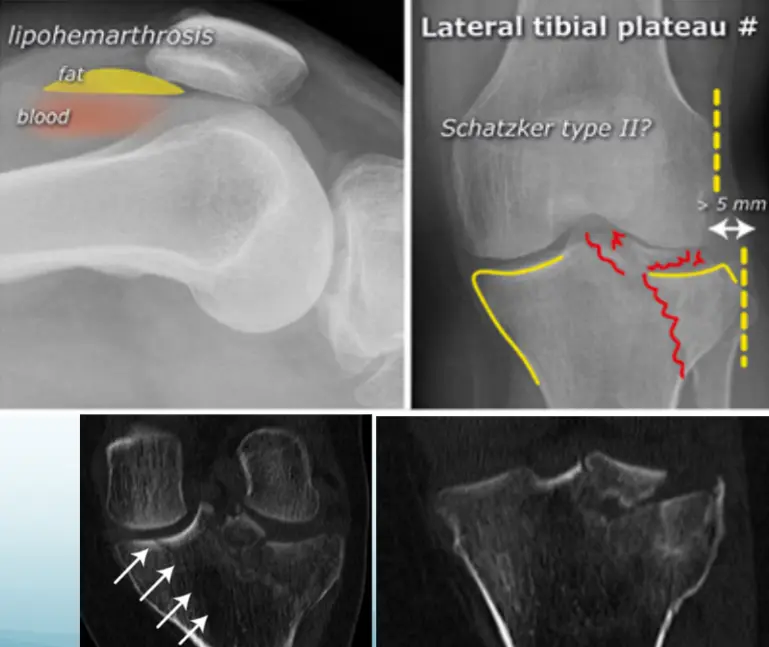
A 32‑year‑old patient fell from a palm tree and now presents with pain and swelling around the left knee.
- Site: Lateral tibial plateau
- Fracture type: Comminuted
- Fracture line: Vertical split
- Displacement: Depressed
- Special issues: CT scan required for detailed assessment
- Management needed: Surgical intervention

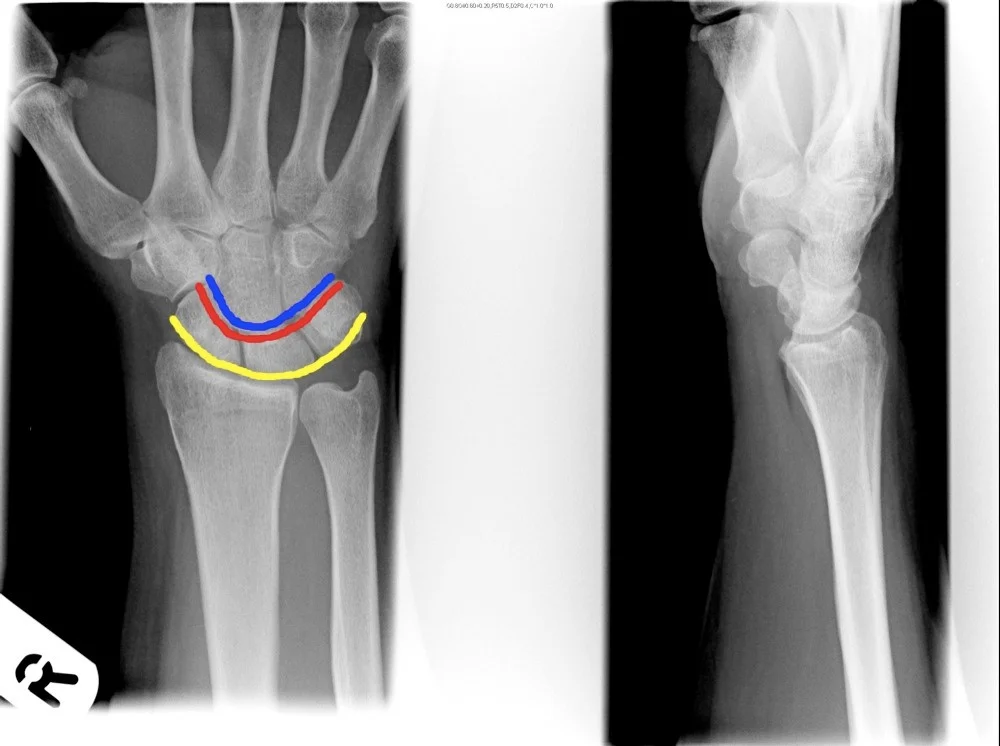
A 29‑year‑old man fell from a ladder and presents with pain in the wrist.
- Site – wrist
- Type – (Specify fracture type)
- Fracture line – (Describe orientation)
- Displacements – (Note any displacement)
- Special issues – (Highlight any neurovascular or soft‑tissue concerns)
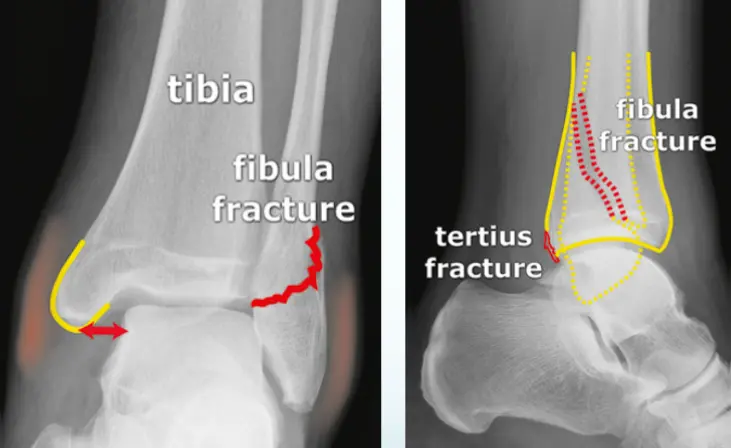
Patient: 32‑year‑old male with a severe twisting ankle injury → painful, swollen and unable to stand.
Findings
- Site: lateral malleolus
- Fracture type: simple
- Fracture line: spiral
- Displacement: gap medially
- Special issue: possible ruptured deltoid ligament

- Site: intertrochanteric
- Type: comminuted
- Fracture line: multiple
- Displacements: varus / overlap
- Special issues: osteoporosis, unstable fracture, no AVN
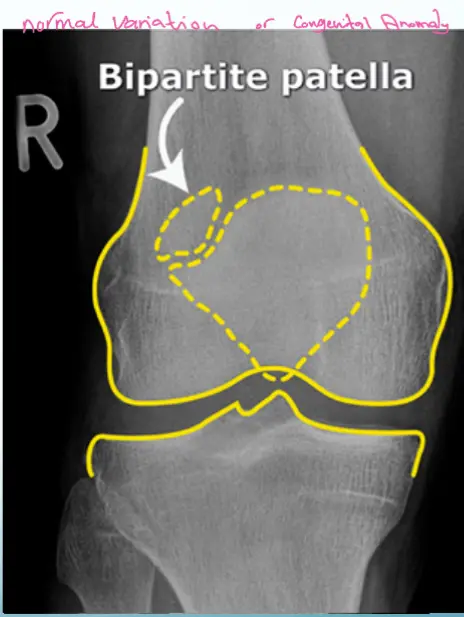
Patient: 26‑year‑old male who fell while running.
External findings: superficial anterior abrasions, but full range of motion retained.
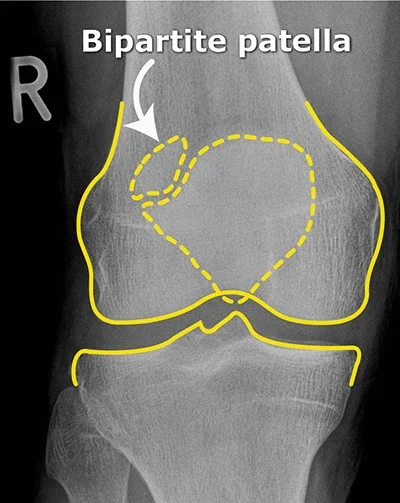
- Upper‑lateral corner of the patella
- Line not as sharp as a fresh fracture
- Area not clearly tender
- Full ROM (consistent with the overall exam)
- Trauma insufficient to cause a definitive fracture

- Site: Neck Lt femur – intra‑capsular
- Type: Simple
- Fracture line: Transverse
- Displacements: Valgus / impaction
- Special issues: Stable; has vascular clips; AVN depends on age

- Site – Bimalleolar ankle fracture
- Type – C (fibular fracture above the syndesmosis); medial malleolus simple
- Fracture line – medial malleolus transverse; lower fibula complex (comminuted)
- Displacements – medial malleolus & talus shifted laterally
- Special issues – syndesmosis injured; intra‑articular fracture needs anatomical reduction (ORIF)

- Site – Medial malleolus intact; fibular fracture present.
- Fibular fracture – Type B (located at the level of the syndesmosis), simple pattern with an irregular transverse fracture line.
- Displacement – Talus shifted laterally.
- Special issues – Deltoid ligament ruptured; syndesmosis may be intact.
- Management – Requires anatomical ORIF and ligament repair.

Site: Medial malleolus
Type: Simple intra‑articular fracture
Fracture line: Vertical
Displacements
- Gap in joint line
Special issues
- Requires anatomical reduction and absolute stability
- Possible lateral collateral ligament injury
Bone and Joint Alignment
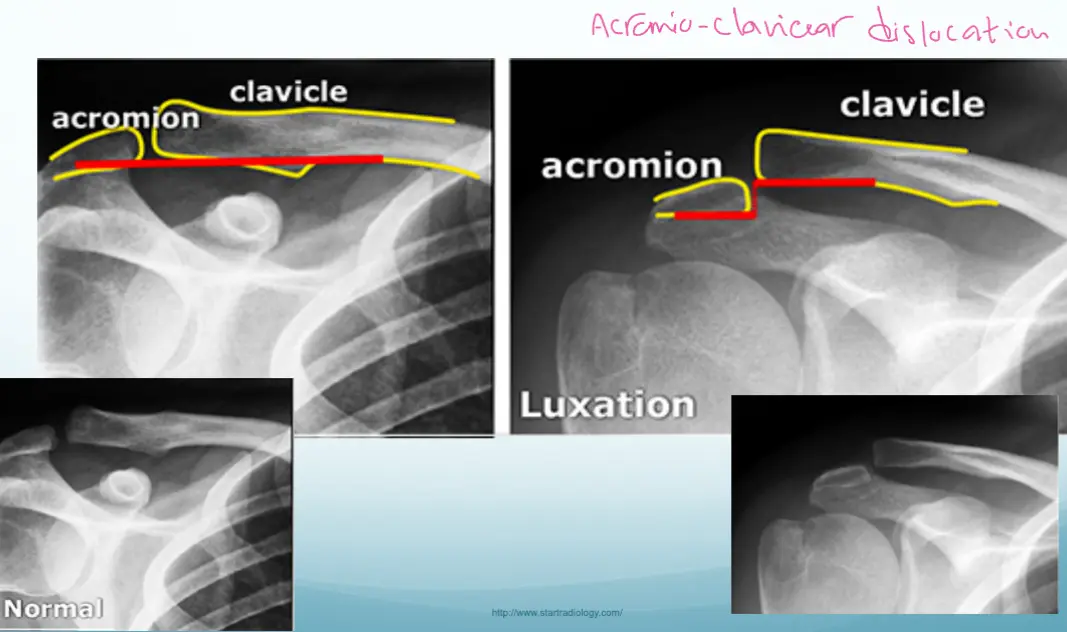
A 32-year-old football player complained of right shoulder pain after he fell down on it during a football game.
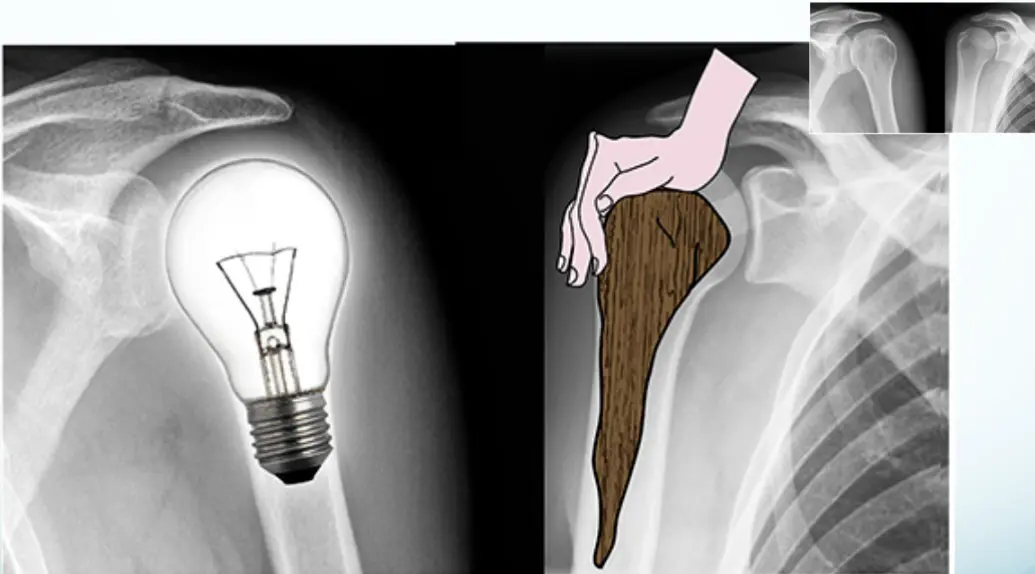 Figure 18. Lightbulb sign in posterior shoulder luxation on an AP image (a); normal AP image of the right shoulder for comparison (b).
Figure 18. Lightbulb sign in posterior shoulder luxation on an AP image (a); normal AP image of the right shoulder for comparison (b).
 During a rugby game, a player complained of right shoulder pain following a frontal confrontation with an opponent. External rotation is particularly painful. A shoulder x-ray is made
During a rugby game, a player complained of right shoulder pain following a frontal confrontation with an opponent. External rotation is particularly painful. A shoulder x-ray is made
Reading a fracture
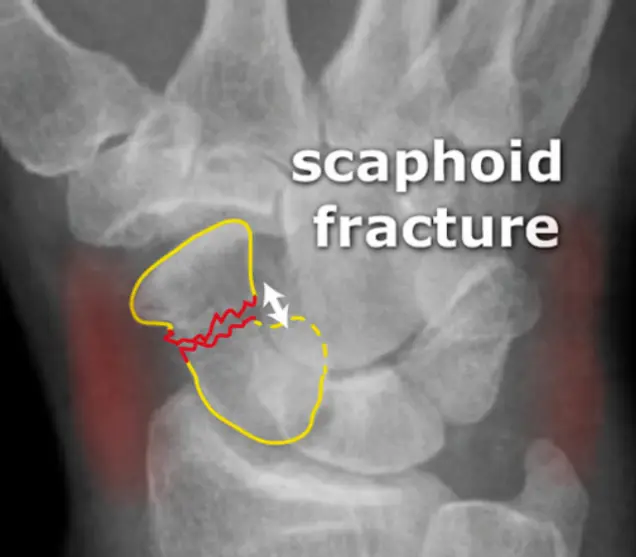 A 37-year old man fell from a down the stairs, C/O pain at wrist • Site • Type • Fracture line
A 37-year old man fell from a down the stairs, C/O pain at wrist • Site • Type • Fracture line
- Displacements
- Special issues
- Site
- Type
- Fracture line
- Displacements
- Special issues

- • Site
- • Type
- • Fracture line
- • Displacements
- • Special issues

36‑year‑old lady presents after a twisting ankle injury.
The ankle is swollen and tender, and she is unable to bear weight.
- Question: Is there a fracture?
- Likely site: possible lower fibula fracture
- Imaging needed: a lateral ankle film
-
Reading X‑rays – general information and systematic approach
- Bones – identify which bone and which view; assess bone age and quality/shape
- Joints – evaluate joint spaces and alignment
- Soft tissues – look for any abnormalities
-
Fracture assessment – examine two joints from two views
- Location – precise site of the fracture
- Type – transverse, oblique, spiral, etc.
- Fracture line – orientation and pattern
- Displacement – degree of fragment shift
- Special issues – periosteal reaction, comminution, involvement of growth plates, etc.
-
Key checklist – always look for fractures and any periosteal reaction; use clear anatomical descriptors throughout the report.
-
Recommended web resources – excellent references for further study:
Reading Bone
- Bone age
- Epiphyseal plates open/closed (child vs. adult)
- Bone Quality (Texture)
- Generalized
- Local area
- Cortex
- Medulla
- Bone Morphology
- Shape, size, deformities

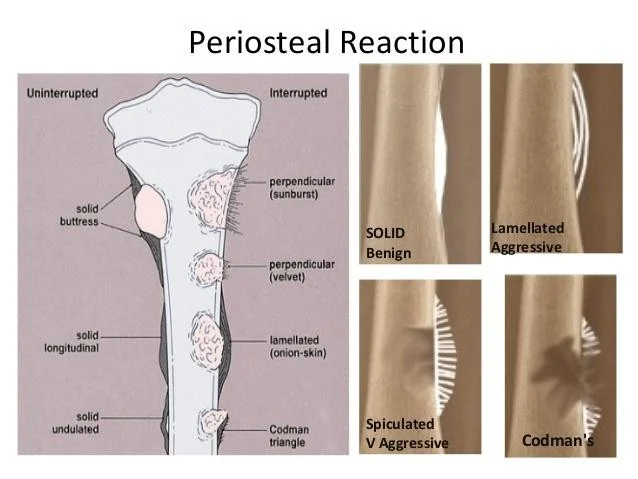
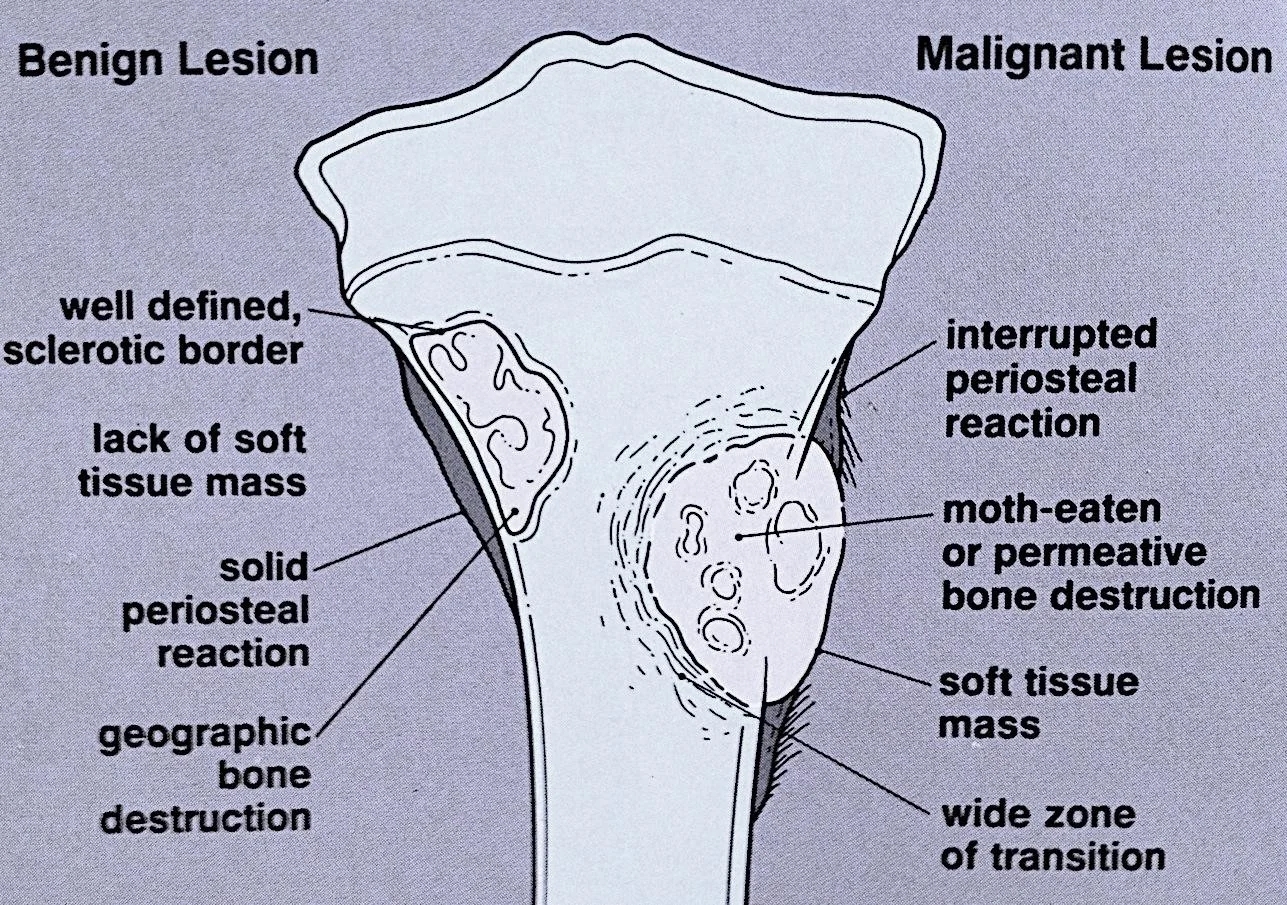
Reading Bone - Periosteal Reaction and Destruction
- Periosteal reaction
- Solid: Benign
- Interrupted: Aggressive
- Lamellated / Sun-burst / Codman’s triangle
- Bone growth
- Bone destruction
 periosteal reaction
periosteal reaction
 bone growth
bone growth
Bone Destruction

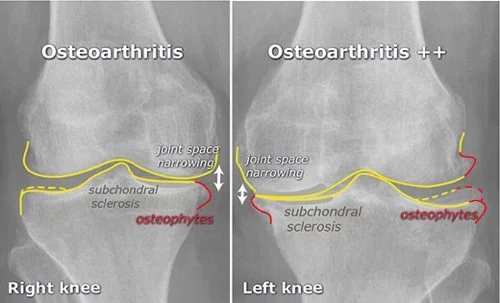
Reading Joints
- Position
- Relations
- Alignment
- Joint “Space”
- Joint line
- Subchondral bone
Joint Position and Relations

Joint Anatomy
- The annotations include:
- Joint space
- Cartilage
- Meniscus
- Joint soft tissues
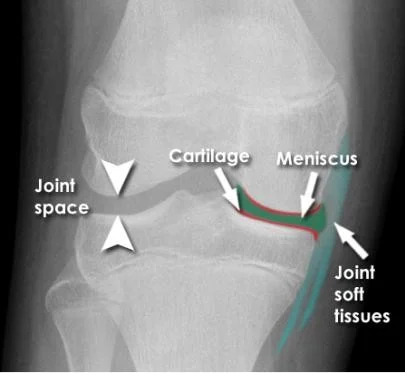
Bone and Joint Alignment

Joint Space
- **Joint narrowing**
- **Osteophytes**

Bone and Joint Examples



Soft Tissue Reading
- In relation to bone cortex
- Next to bone
- e.g. fat pad
- Muscles
- Muscle planes, bulk
- Other soft tissues
- Vessels, lungs, organs, cartilage
- Calcifications, Air, Fluid, …



Look for the Unexpected
- Minor narrowing of the subacromial space (arrowheads) - suggesting rotator cuff disease - very common cause of shoulder pain
- It would be easy to consider this the only abnormality if not checking the image systematically
- Unexpected apical lung mass!
- Clinically suspected rotator cuff disease
- Pain distal to the elbow - rarely if ever caused by shoulder pathology
- Diagnosis
- Minor rotator cuff disease
- ‘Pancoast’ tumour - apical lung cancer (cause of distal pain - referred from brachial plexus)

Artifacts Obscuring Diagnosis

The Fabella - Normal Variant

Bipartite Patella - Normal Variant
- No localized tenderness
- Superolateral
- Line not that of a fresh fracture
Osteoarthritis Examples

Patellar Position
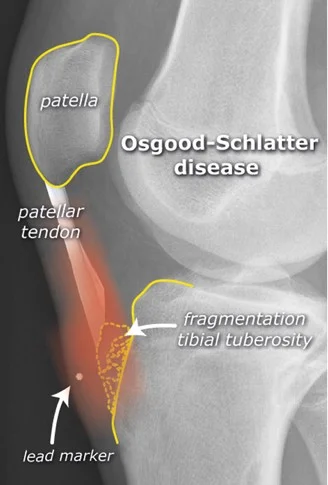
Traction Apophysitis
- Osgood Schlatter
64-year-old lady Pain R shoulder Limited ROM


• Inflamed tendons


Osteoarthritis


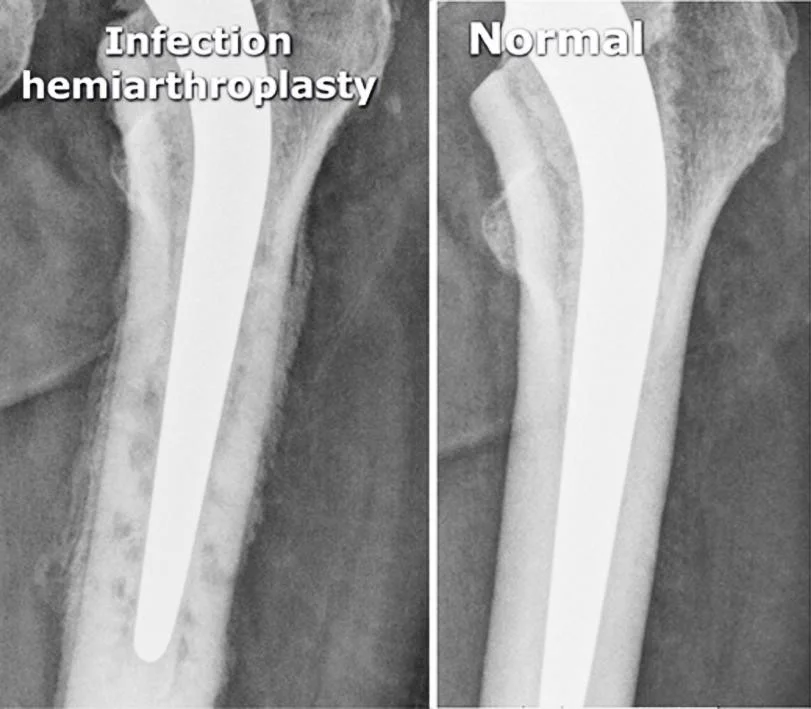
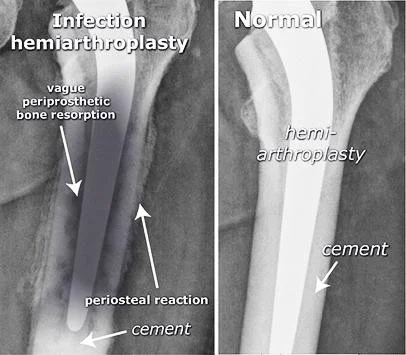
Arthroplasty
- Total Hip Arthroplasty (THA)
- Hemiarthroplasty (HAP)


Infected Arthroplasty
- Pain after arthroplasty
- Mild fever
Infection hemiarthroplasty
- vague periprosthetic bone resorption
- periosteal reaction
- cement
Normal
- hemi-arthroplasty
- cement
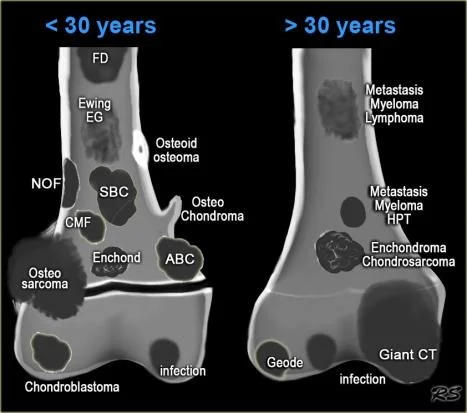
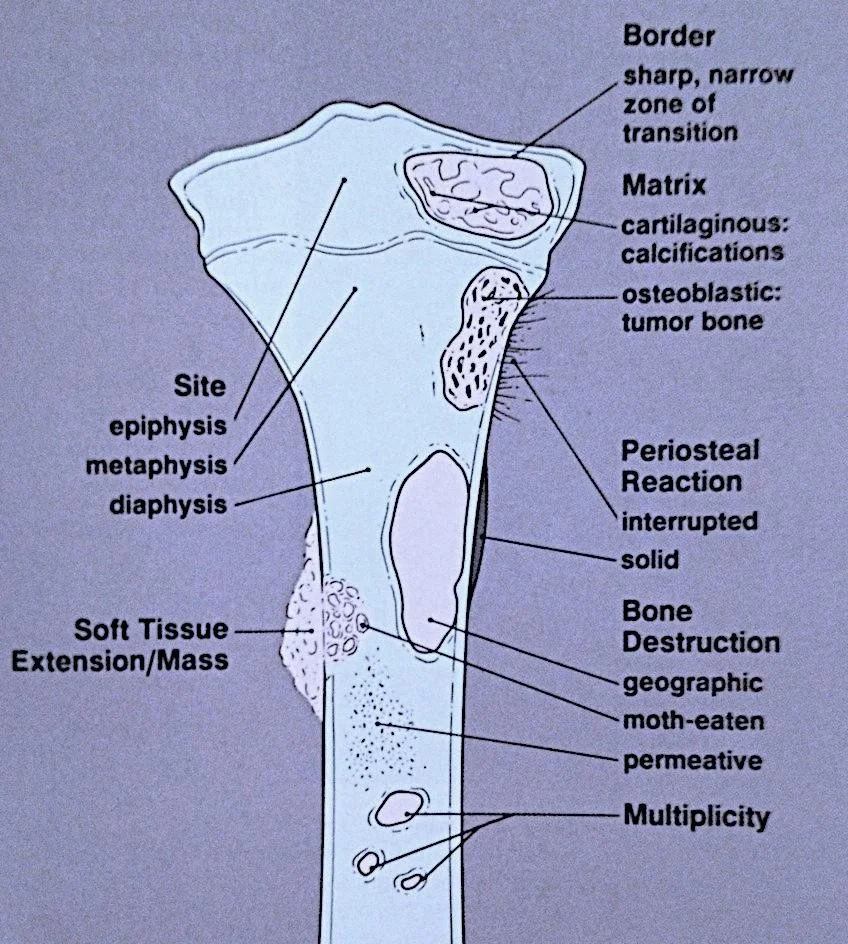
Reading Bone Lesions
- Which bone, and which site in bone?
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-defined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
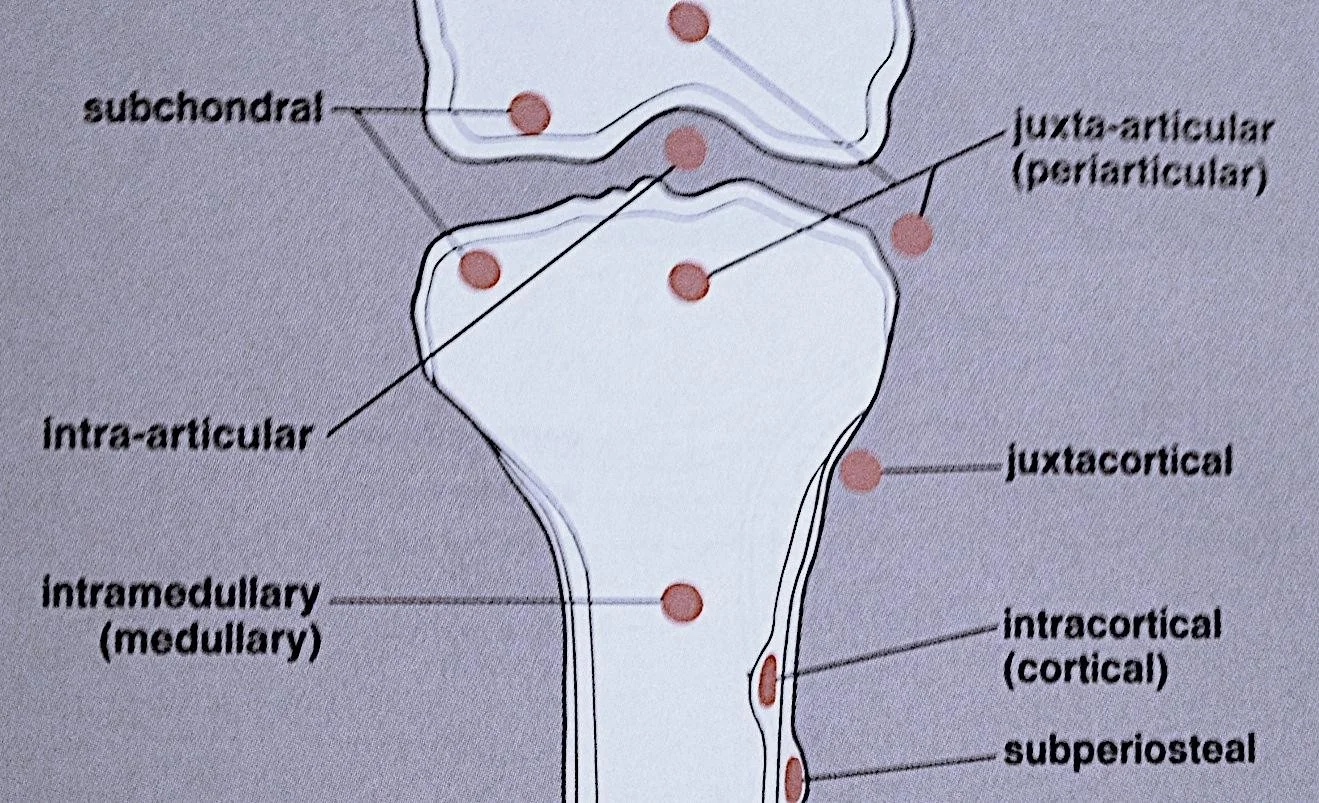
Location
- subchondral
- intra-articular
- intramedullary (medullary)
- juxta-articular (periarticular)
- juxtacortical
- intracortical (cortical)
- subperiosteal

- Which bone, and which site in bone?
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-ndefined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
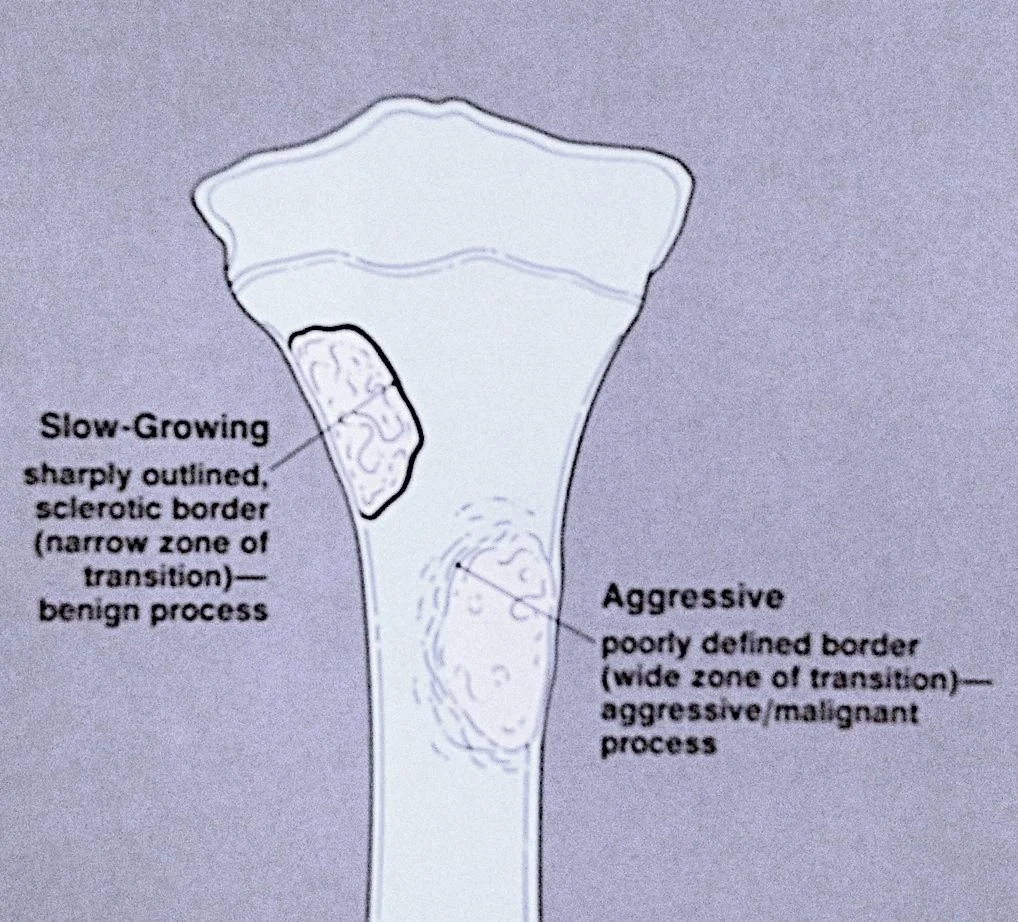
The Border
- Slow-Growing
- sharply outlined, sclerotic border (narrow zone of transition)—benign process
- Aggressive
- poorly defined border (wide zone of transition)—aggressive/malignant process
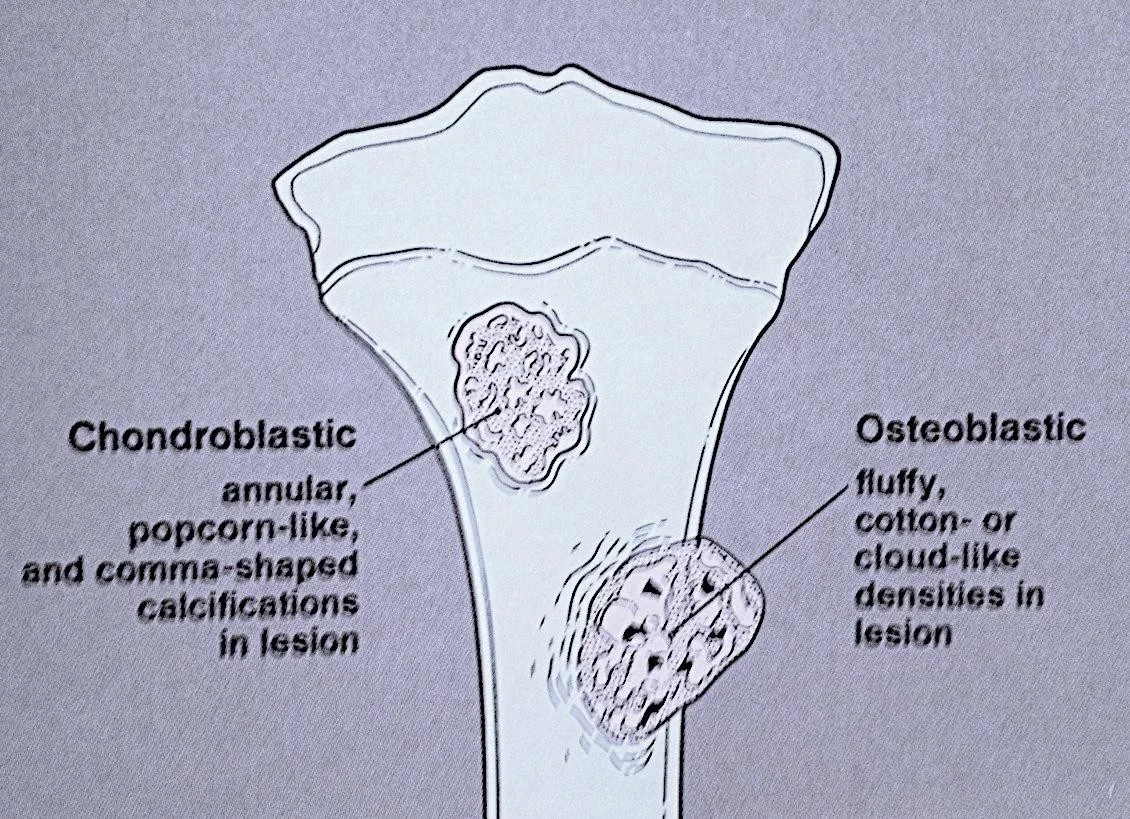
The Matrix
-
Chondroblastic
- annular, popcorn-like, and comma-shaped calcifications in lesion
-
Osteoblastic
- fluffy, cotton- or cloud-like densities in lesion
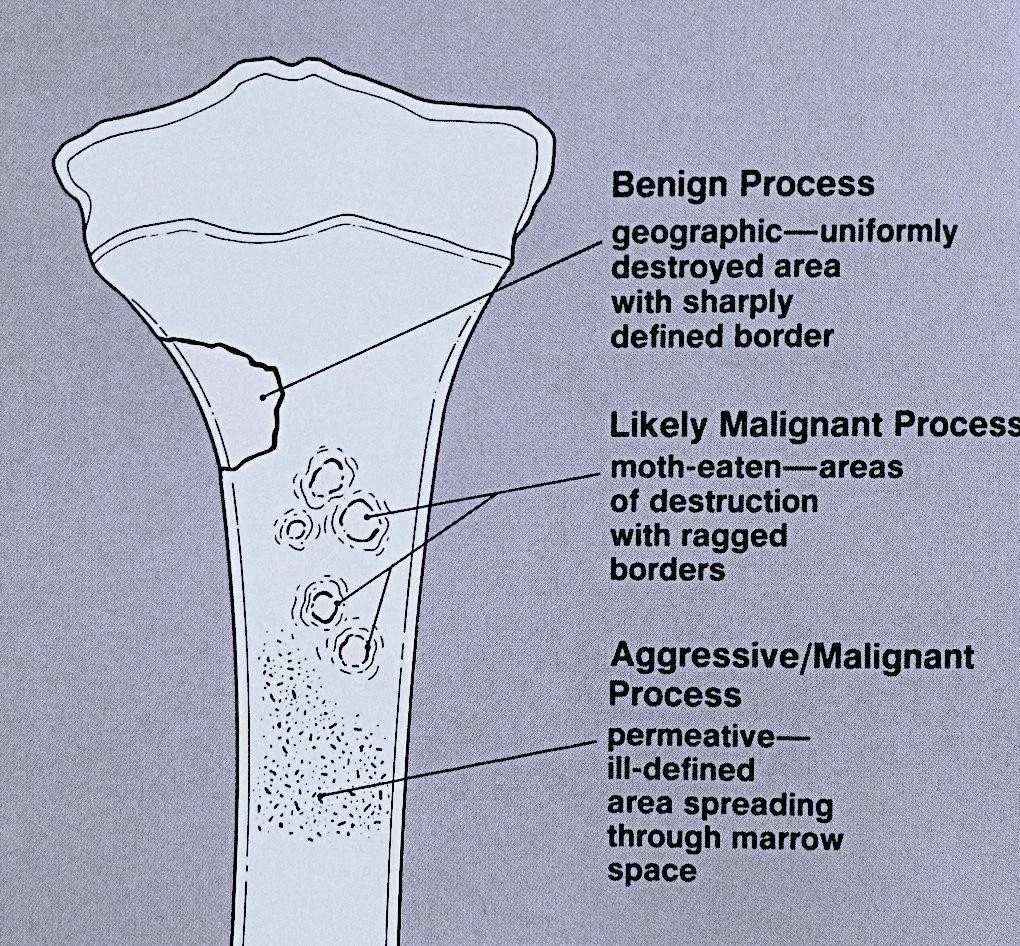
Type of Bone Destruction
-
Benign Process
- geographic—uniformly destroyed area with sharply defined border
-
Likely Malignant Process
- moth-eaten—areas of destruction with ragged borders
-
Aggressive/Malignant Process
- permeative—ill-defined area spreading through marrow space
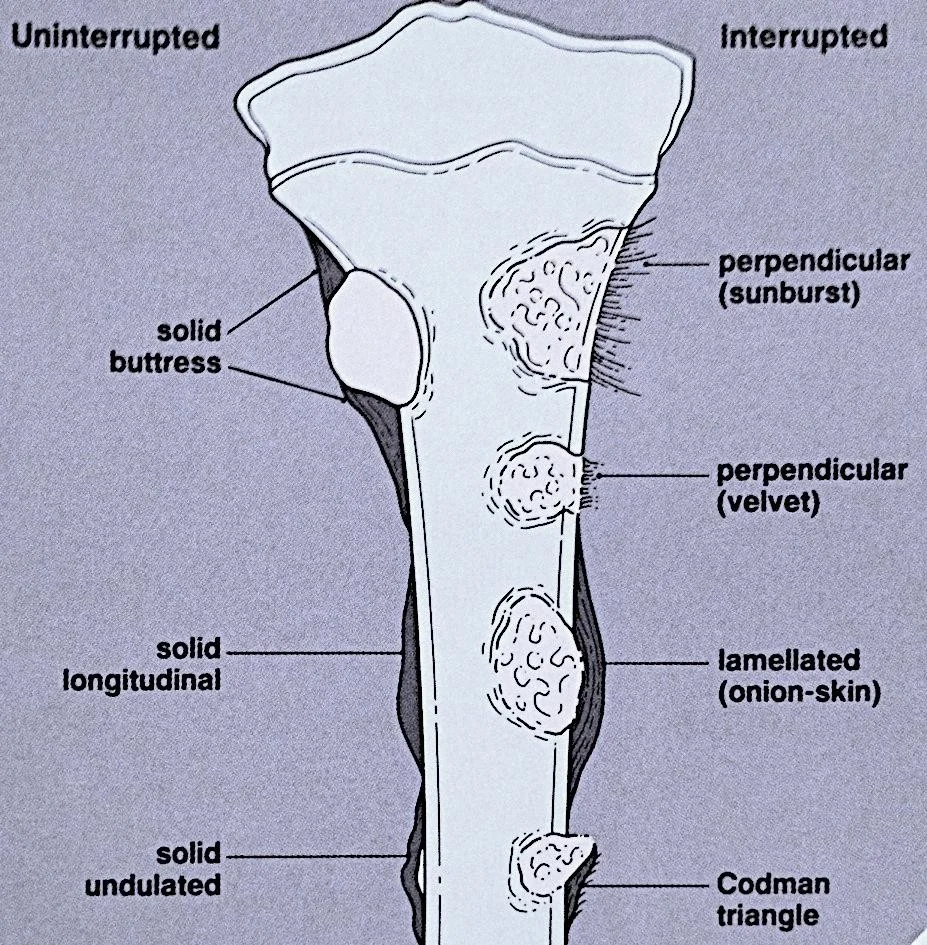
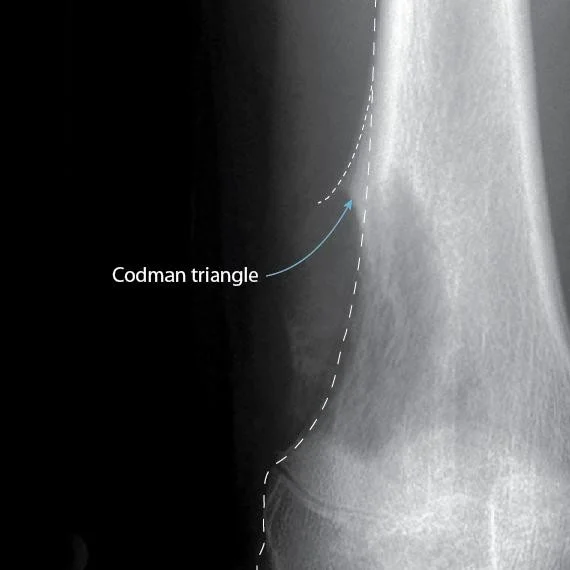
Type of Periosteal Reaction
-
Uninterrupted
- solid buttress
- solid longitudinal
- solid undulated
-
Interrupted
- perpendicular (sunburst)
- perpendicular (velvet)
- lamellated (onion-skin)
- Codman triangle
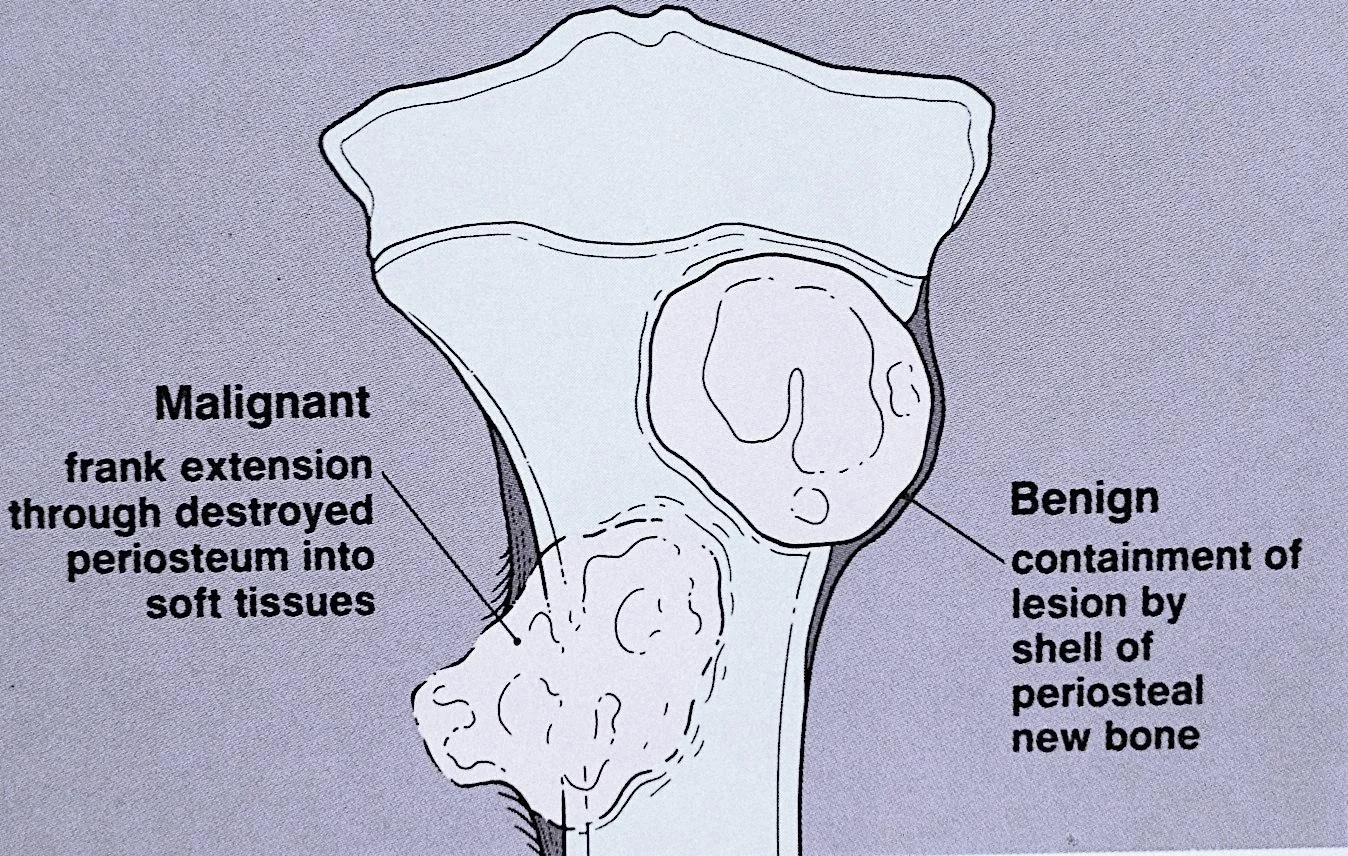
Soft Tissue Extension
-
Malignant
- frank extension through destroyed periosteum into soft tissues
-
Benign
- containment of lesion by shell of periosteal new bone
Benign Vs. Malignant
Benign Lesion
- well defined, sclerotic border
- lack of soft tissue mass
- solid periosteal reaction
- geographic bone destruction
Malignant Lesion
- interrupted periosteal reaction
- moth-eaten or permeative bone destruction
- soft tissue mass
- wide zone of transition
Type of Periosteal Reaction - Examples
Codman Triangle
Sunburst Pattern

Case 1: 45-year-old Lady with Knee Pain
Patient Profile: 45-year-old lady with knee pain

Initial Assessment:
Key Observations:
- Osteopenic lesion
- Eccentric
- Clear narrow zone of transition
- Breaking through posterior cortex
- Periosteal reaction
Further Investigation: MRI recommended
MRI Findings: Soft tissue extension

Diagnosis: Biopsy showed mammary carcinoma - had undiagnosed Ca Breast
Case 2: 15-year-old Boy - Asymptomatic

 Patient Profile: 15-year-old boy, asymptomatic
Patient Profile: 15-year-old boy, asymptomatic
Diagnosis: Simple bone cyst
Key Features:
- Osteopenic lesion
- Uniform consistency
- Eccentric
- Clear narrow zone of transition
- Respecting cortex
- No periosteal reaction
Case 3: 12-year-old Boy with Swelling Lower Leg
 Patient Profile: 12-year-old boy with swelling lower leg
Patient Profile: 12-year-old boy with swelling lower leg
Diagnosis: Aneurysmal bone cyst
Key Features:
- Osteopenic lesion
- Eccentric
- Clear narrow zone of transition
- Respecting cortex
- Ballooning cortex
- No periosteal reaction
Case 4: 45-year-old with Pain R Thigh


Patient Profile: 45-year-old with pain R thigh, swollen, tender
Key Features:
- Osteopenic lesion
- Inside medulla
- Unclear /Wide zone of transition
- Ill-defined
- Respecting cortex
- No periosteal reaction
Assessment: Aggressive lesion, could be Tumor / infection, Need further investigation
Key Features:
- Widely spread inside medulla
- Extends to soft tissues
- Edema in soft tissues
Diagnosis: Osteomyelitis
Case 6: 2-year-old with Fever, Vomiting, Pain L Hip

Patient Profile: 2-year-old with fever, vomiting, pain L hip, limited ROM
Key Features:
- Localized osteopenic lesion upper metaphysis L femur
- Reaching epiphyseal plate
Differential Diagnosis: Osteomyelitis, Septic arthritis
Further Investigation:
- CBC, Diff. WBC, CRP, ESR
- Ultrasound
- MRI
Ultrasound Findings: U/S: large hip effusion with echogenic content (Pus)
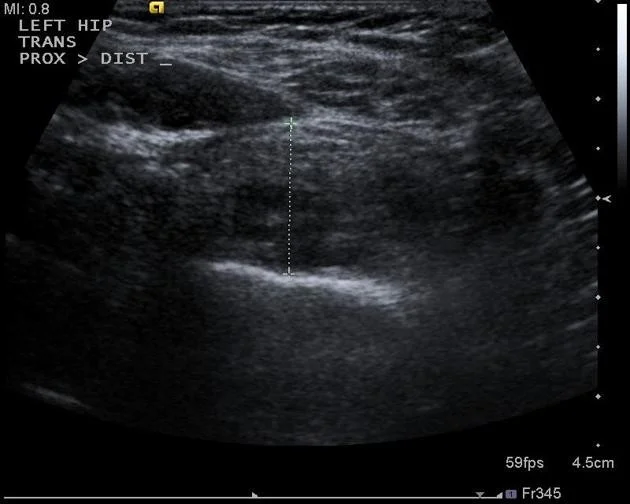
MRI Findings: MRI: hyperintense T2, Oedema, Fluid collection outside bone, Effusion in hip joint

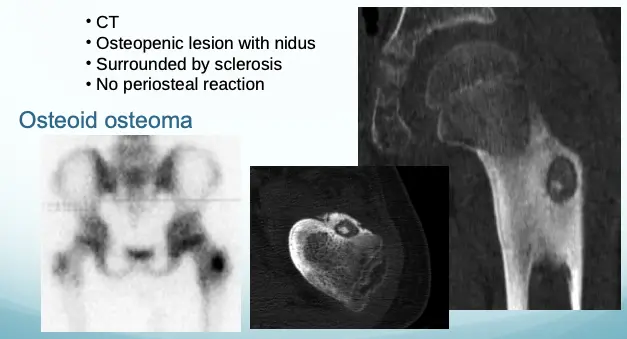
Case 8: 10-year-old with Pain L Hip
 Patient Profile: 10-year-old with pain L hip, no tenderness, full ROM
Patient Profile: 10-year-old with pain L hip, no tenderness, full ROM
Key Features:
- Osteopenic lesion
- Sclerosis in intertrochanteric area
Further Investigation: Need CT
CT Findings:
- Osteopenic lesion with nidus
- Surrounded by sclerosis
- No periosteal reaction
Diagnosis: Osteoid osteoma
Case 10: 17-year-old with Painful Swelling Lower Thigh
 Patient Profile: 17-year-old with painful swelling lower thigh
Patient Profile: 17-year-old with painful swelling lower thigh
Key Features:
- Osteosclerotic lesion
- Inside and outside medulla
- Unclear /Wide zone of transition
- Ill-defined
- Not respecting cortex
- Extending into soft tissue
- Periosteal reaction
Diagnosis: Osteogenic sarcoma
Other Imaging Techniques
- Bone scan (Tc99):
- Shows the site of lesion / skip lesions / metastasis
- CT:
- Intra-osseous and extra-osseous structure and extension
- Good in deep bones (pelvis, spine)
- MRI:
- Shows:
- Soft tissue and cartilage
- Spread of lesion/tumor:
- Within bone, into joints, into soft tissue
- Relation to vessels
- Shows:
Summary of Key Points
- Systematic approach:
- General information
- Reading bone
- Reading joints
- Reading soft tissue
Reading Bone Lesions - Key Questions
- Which bone, and which site in bone?
- Solitary or multiple?
- Bone forming or bone eating?
- Margins: well-defined or ill-defined?
- Calcifications in the lesion?
- Is cortex eroded or destroyed?
- Is there periosteal new bone formation?
- Soft tissue extension?
Reading Joints - Key Aspects
- Position
- Relations
- Alignment
- Joint “Space”
- Joint line
- Subchondral bone