Systemic & Metabolic Response to Injury
Dr. Omar Alaidaroos
Injury could be fracture, burn, sepsis or surgical operation
-
Neuroendocrine mechanisms that act locoregionally and systemically to try to restore the body to its pre-injury condition. i.e., SURVIVAL***
-
For survival, these mechanisms can cause great harm. By minimizing and manipulating the metabolic response to injury, surgical mortality, morbidity and recovery times can be greatly improved. i.e., GOLDEN HOUR***
-
Severity of the injury …. Host fitness
-
Triggers: Pain ……. Hypovolaemia
-
Restore tissue function
-
Eradicate invading Microorganisms—Bacterial Translocation
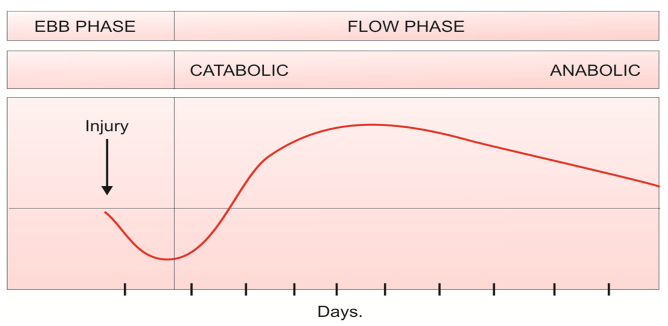
Metabolic Response to Injury: Two phases
-
Initial ‘Ebb’ phase: SHOCK Usually lasting for 24 hrs. It is the phase of reduced energy expenditure; patients were cold and hypotensive, shocked.
When intravenous fluids and blood transfusion became available, this shock was sometimes found to be reversible and in other cases irreversible. If the individual survived the ebb phase, patients entered
-
The flow phase has a
-
catabolic phase lasting for 3-8 days The catabolic phase is characterized by increased metabolism, hyperglycemia, lipolysis, negative nitrogen balanceZ, increased heat production and oxygen consumption. followed by the
-
anabolic or ‘recovery’ phase lasting for several weeks or months. phase characterized by protein and fat synthesis and associated with weight gain
-
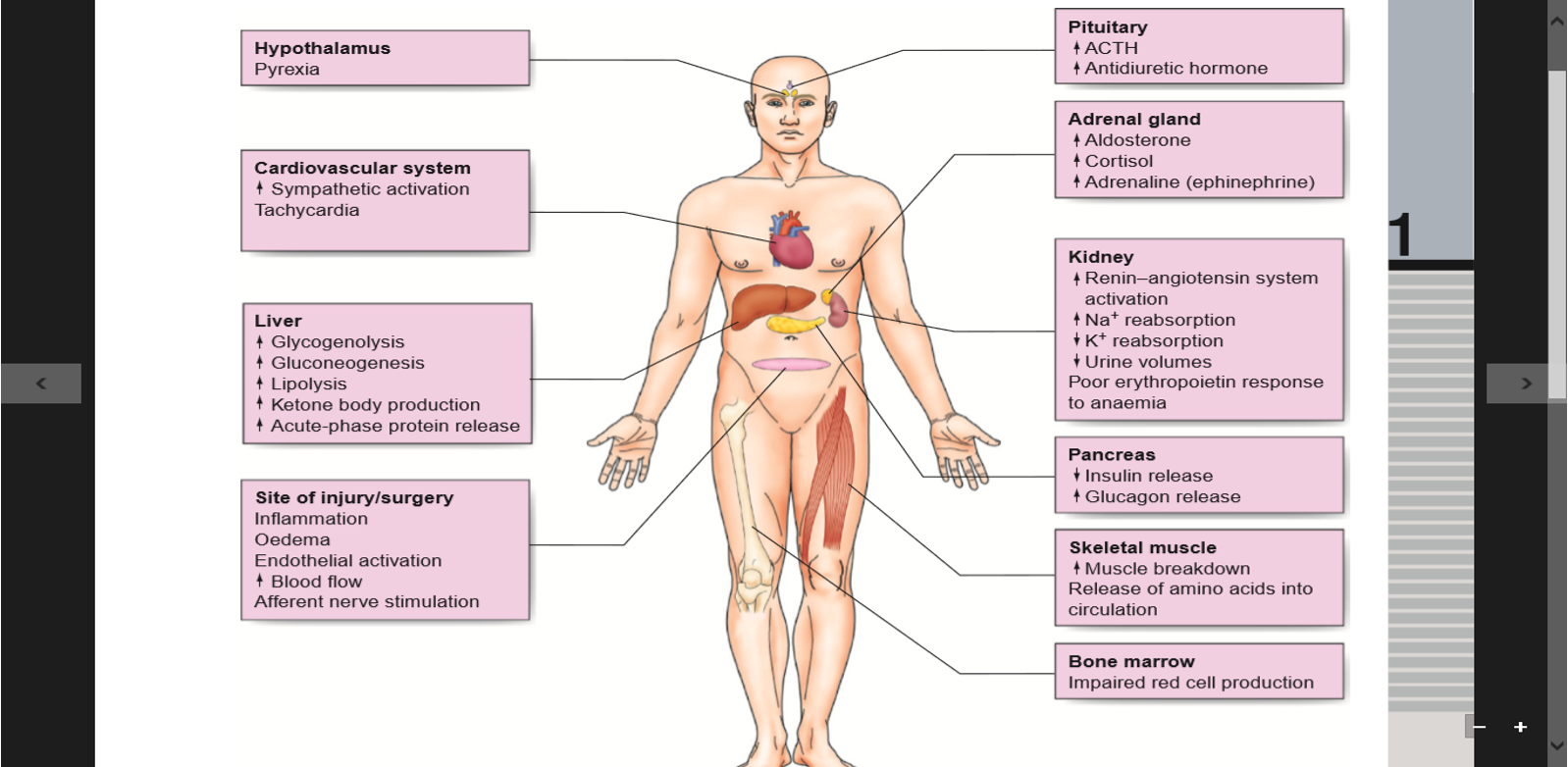
Factors mediating the metabolic response to injury
Four principal systems produce the response:
-
Acute phase inflammatory response.
-
Vascular endothelial cell response.
-
Sympathetic nervous system
-
Endocrine response
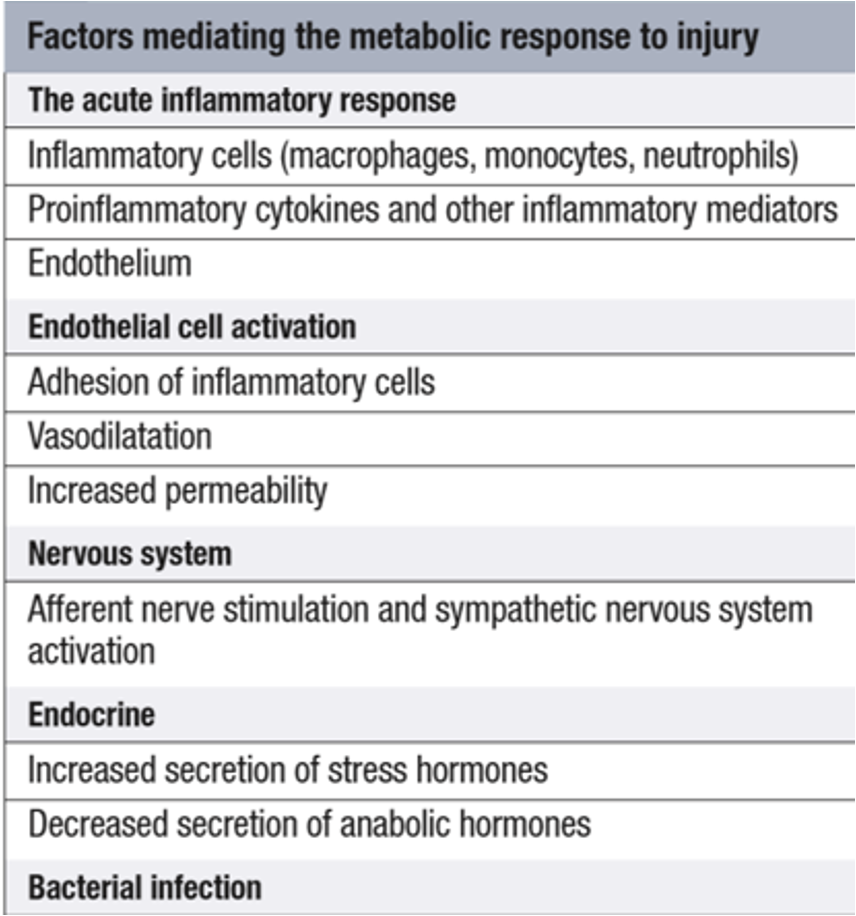
1. The acute inflammatory response:
Physical damage to tissues results in local activation of cells such as tissue macrophages which release a variety of Cytokines as:
-
Interleukin- 8 (IL-8), attract large numbers of circulating macrophages and neutrophils to the site of injury.
-
Tumour necrosis factor alpha (TNF-α), IL-1 and IL-6, activate these inflammatory cells, enabling them to clear dead tissue and kill bacteria.
-
Cytokines act locally (paracrine action), their release into the circulation initiates some of the systemic features of the metabolic response, such as fever (IL-1) and the acute-phase protein response (IL-6)Z
-
Other pro-inflammatory (prostaglandins, kinins, complement, proteases and free radicals)
-
Anti-inflammatory substances such as antioxidants (e.g., glutathione, vitamins A and C), protease inhibitors (e.g., α2 -macroglobulin) and IL-10 are also released
Severe trauma can:
lead to -------→ excessive cytokine release Resulting in -------→ progressive organ dysfunction with lethal consequences.
The clinical condition of the patient depends on the extent to which the inflammation remains localized and the balance between these pro-and anti- inflammatory processes.
Systemic inflammatory response syndrome -SIRS
A clinical response to a nonspecific insult of either infectious or non infectious origin.
SIRS is defined as 2 or more of the following variables:
- Fever of more than 38°C (100.4°F) or less than 36°C (96.8°F)
- Heart rate of more than 90 beats per minute
- Respiratory rate of more than 20 breaths per minute or arterial carbon dioxide tension (PaCO2) of less than 32 mm Hg
- Abnormal white blood cell count (>12,000/µL or < 4,000/µL or >10% immature [band] forms)
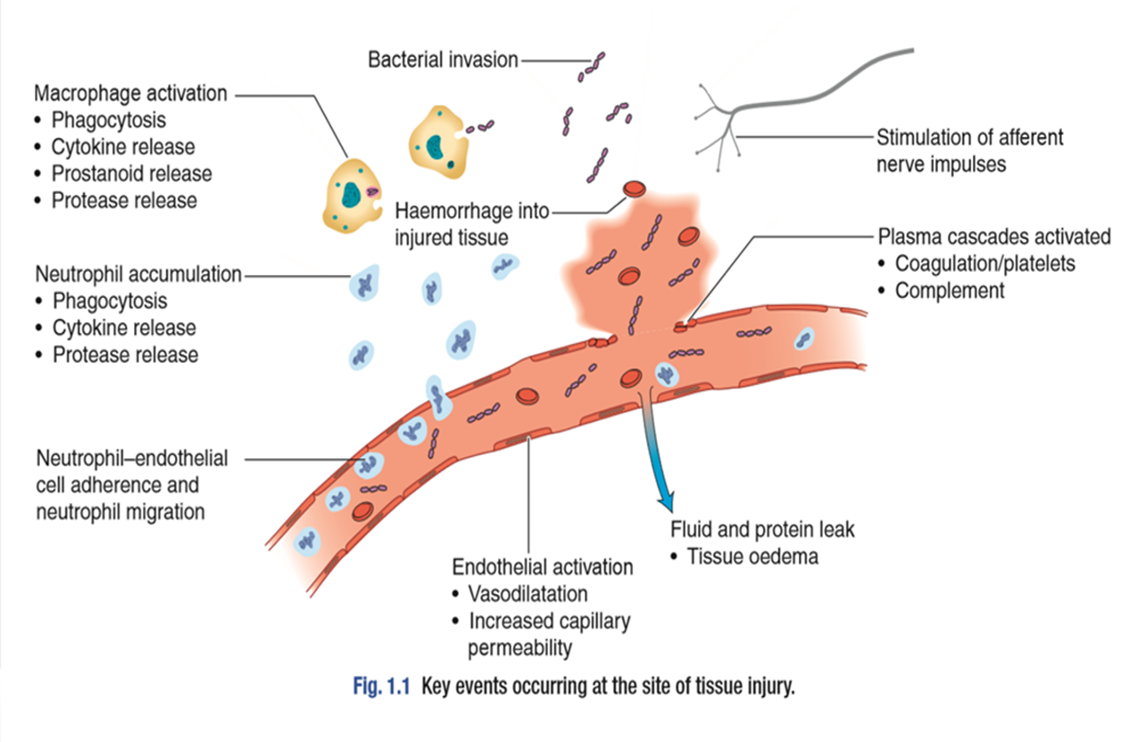
II. Afferent nerve impulses/ sympathetic activation:
Following injury, the afferent nervous impulses (including pain) arising from damaged tissues and from the hypovolemia associated with fluid loss, is carried through spinothalamic pathways to stimulate the hypothalamus.
So, results in a combined neural and endocrine discharge: Activation of the sympathetic nervous system leads to the release of noradrenaline from sympathetic nerve fiber endings and adrenaline from the adrenal medulla that is responsible for the traditionally named ‘fight or flight’ response by cardiovascular and metabolic actions. (Both α and β receptors effects occur) viz.
A) Cardiovascular effects —
- Vasoconstriction, increased heart rate (α effects) & contractility (β effects).
B) Metabolic effects:
- Glycogenolysis, lipolysis and calorigenic (β-effect).
- Gluconeogenesis and suppression of insulin secretion (α effect).
III. The endothelium and blood vessels:
The damaged vascular endothelium produce a number of substances, e.g. NO, which affects vasomotor tone and vessel permeability.
The expression of adhesion molecules upon the endothelium leads to leucocyte adhesion and transmigration
Increased local blood flow due to vasodilatation, secondary to the release of kinins, prostaglandins and nitric oxide, as well as increased capillary permeability increases the delivery of inflammatory cells, oxygen & nutrient substrates important for healing.
Colloid particles (principally albumin) leak into injured tissues, resulting in oedema.
The exposure of tissue factor promotes coagulation which, together with platelet activation, decreases haemorrhage. But at the risk of causing tissue ischaemia.
If inflammatory process generalized → microcirculatory thrombosis & disseminated intravascular coagulation (DIC) = death
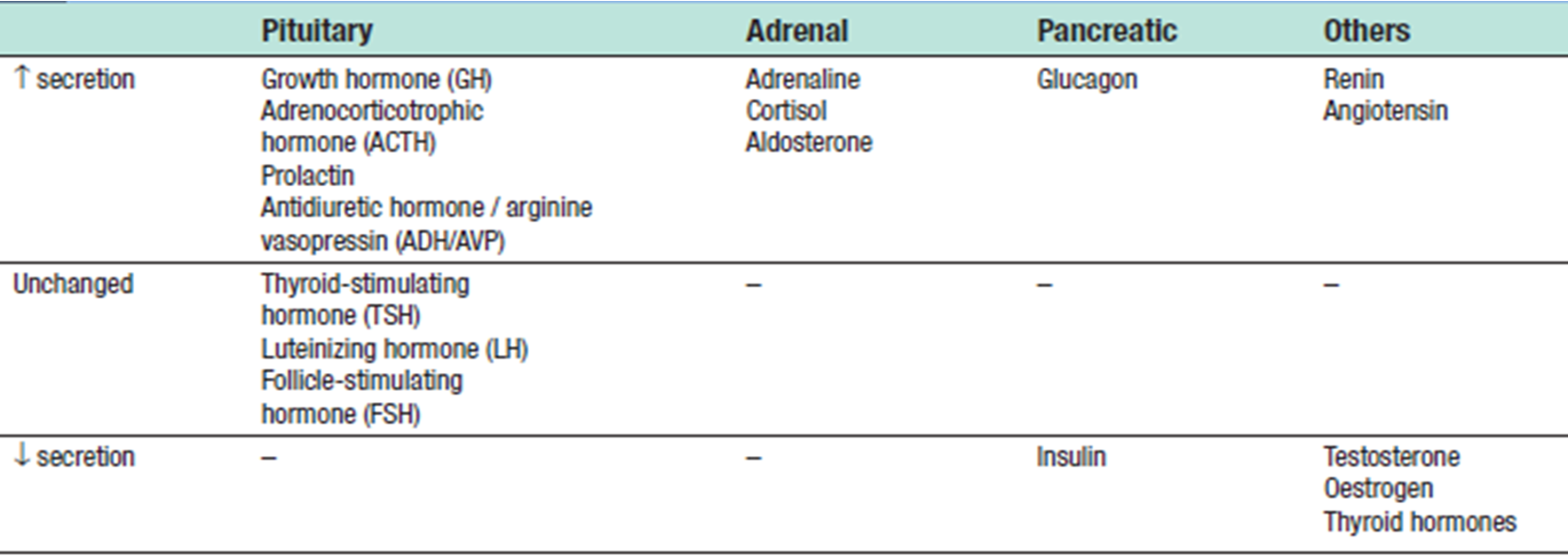
IV. The endocrine response to surgery:
Surgery leads to complex changes in the endocrine mechanisms that maintain the body’s fluid balance and substrate metabolism, with changes occurring to the circulating concentrations of many hormones following injury.
This occurs either as a result of direct gland stimulation or because of changes in feedback mechanisms.
Catabolism Phase
-
Carbohydrate, protein and fat catabolism is mediated by the increase in circulating catecholamines and proinflammatory cytokines, as well as the hormonal changes observed following surgery.
-
Increased Metabolism After Injury:
-
With acute injury, muscle and liver glycogen are used as energy fuel (glycogenolysis).
-
The muscle and liver glycogen, however, cannot continue to supply glucose all the time, as its total store would be exhausted in a day or two.
-
After this, protein and fat stores are mobilized to meet the energy requirement.
-
Fat is the principal energy store of the body.
-
Protein can also be used as an energy source, but it cannot be mobilized beyond a certain level, since their excessive breakdown would lead to muscle wasting, ineffective coughing, impaired wound healing and a diminished synthesis of enzymes.
Carbohydrate Metabolism After Injury
-
Catecholamines and glucagon stimulate glycogenolysis in the liver leading to the production of glucose and rapid glycogen depletion.
-
Gluconeogenesis, the conversion of noncarbohydrate substrates (lactate, amino acids, glycerol) into glucose, occurs simultaneously.
-
Hyperglycaemia occurs immediately after injury because glucose is mobilized from stored glycogen in the liver by catecholamines, and glucocorticoids, and because insulin resistance of peripheral tissues impairs their uptake of glucose (the ‘diabetes’ of injury or traumatic diabetes).
-
Glucose provides energy for obligate tissue such as the CNS, leukocytes in the wound and red cells (cells not requiring insulin for glucose transport).
-
In major injuries, the inflammatory cell infiltrate can account for 70 percent of the glucose uptake.
Fat Metabolism
-
After Injury Fat is the main energy source in trauma and starvation.
-
Lipolysis involves hydrolysis of triglycerides to fatty acids and glycerol.
-
Catecholamines produce lipolysis of adipose tissue.
-
The brain adapts to utilize ketones rather than glucose and this allows greater dependency on fat metabolism, so reducing muscle protein and nitrogen loss by about 25%.
Summary of metabolic responses to surgery and trauma
Biochemical and Fluid Balance disturbance
-
Salt and water retention: This results from both aldosterone and cortisol with raised levels of ADH, further hindering excretion of free water and resulting in lower volumes of high osmolality urine.
Any reduction in renal perfusion from hypotension secondary to hypovolemia or from the administration of NSAID worsens oliguria and can lead to acute renal failure.
-
Hyponatremia (Na+) – It occurs partly due to a dilutional effect from retained water (due to ADH) and partly because sodium drifts into cells (impaired Na-pump). It does not indicate sodium deficiency, as it occurs at a time when total body sodium is elevated.
No extra sodium is needed in the first 24 – 48
-
Acid-base abnormalities: The commonest change is the metabolic alkalosis due to intense reabsorption of sodium in distal tubules of the kidney, accompanied by excretion of K+ and H+ ions. In more severe injuries, a metabolic acidosis supervenes due to poor tissue perfusion and anaerobic metabolism with accumulation of lactic acid.
Urinary changes in metabolic response to injury:
- ↓ urine volume secondary to ↑ ADH and aldosterone release
- ↓ urinary sodium and
- ↑ urinary potassium secondary to ↑ aldosterone release
- ↑ urinary osmolality ↑ urinary nitrogen excretion due to the catabolic response to injury
Factors Reducing Metabolic Response ,Quick Recovery:
-
Off fluids and electrolyte lost and transfusion for hemorrhage if Hb is <8 gm/dl.
-
Reducing stimuli’As causing the response during surgical trauma by:
- Gentle tissue handling, Sharp dissection along anatomical planes, Careful hemostasis to remove tissue debris and clots and Careful suturing without strangulation
- Nutritional support, e.g.:
- with amino acid glutamine and arginine supplementation of enteral diets and omega - 3 fatty acids helps to overcome the immunodepression after surgical trauma.
- Control of pain with analgesics:
- like NSAIDs, local regional blockade.
- Correction of:
- Metabolic acidosis or alkalosis.
- Hypoxemia by administration of O2, and attention to airway and breathing.
- Hypovolemia by prompt replacement
- Sepsis
(shallow breathing result in… - give baloons to open alveoli)
ILOs
At the end of this presentation students will be able to describe:
- Body’s local and systemic response to injury.
- Interventions to minimize harmful effects.
- Clinical spectrum of SIRS