SURG
II. Liver function Test:
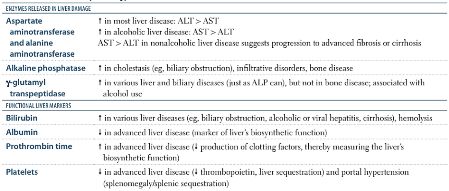
ALT, AST, ALP and GGT are used to distinguish between hepatocellular damage and cholestasis.
-
Alanine transaminase (ALT)- SGPT N= 4-36 U/L
-
Aspartate amino transferase (AST)- SGOT N= 8-33 U/L
-
Alkaline phosphatase (ALP) N= 25-120 U/L
-
Gamma-glutamyltransferase (GGT) N=M:10-55, F: 5-35 U/L) - increases in bile duct injury
Bilirubin, albumin and PT are used to assess the liver’s synthetic function.
- Bilirubin N= 0.1 to 1.2 milligrams per deciliter (mg/dL)
- Albumin N= 3.5 to 5.0 grams per deciliter (g/dL)
- Prothrombin time (PT) N= 9.4 - 12.5 seconds
SGPT = serum glutamic-pyruvic transaminase SGOT= Serum glutamic-oxaloacetic transaminase
What if the patient is jaundiced but ALT and ALP levels are normal? An isolated rise in bilirubin is suggestive of a pre-hepatic cause of jaundice.
AST Aspartate Aminotransferase: (SGOT)
-
Is an enzyme that is present in hepatocytes and myocytes (both skeletal and cardiac muscle)
-
Elevations in AST are most commonly a reflection of hepatocellular injury, but they may also be elevated in myocardial or skeletal muscle injury
Other Laboratory test for Cardiac vascular system
- Troponin: (less then 30ng/L) when muscle or heart cells are injured, troponin leaks out, and its level in blood is raised.
- Ischemia modified albumin (IMA): high level of IMA indicate ischemia.
- natriuretic peptide (NP) NP levels are higher in heart failure. Normal value : 100 (pg/mL)
- Creatine Kinase (CK): diagnosis for acute MI. Normal value : <150 units/L
Gamma-glutamyl transferase: (Gamma GT) A raised GGT can be suggestive of “biliary epithelial damage and bile flow obstruction”. It can also be raised in response to alcohol and drugs such as phenytoin.* A markedly raised ALP with a raised GGT is highly suggestive of cholestasis*.
Isolated rise of Alkaline phosphatase ALP: (25-120 U/L) Used to diagnose liver and bone disease. It is also present in bone and therefore anything that leads to increased bone breakdown can elevate ALP.
Causes of an isolated rise in ALP include:
- Bony metastases or primary bone tumours (e.g. sarcoma)
- Vitamin D deficiency
- Recent bone fractures
- Renal osteodystrophy
Assessment of hepatic function:
- Conjugation and elimination of bilirubin
- Synthesis of albumin
- Synthesis of clotting factors
- Gluconeogenesis
Investigations assess synthetic liver function:
- Serum bilirubin
- Serum albumin
- Prothrombin time (PT)
- Serum blood glucose
Albumin levels can fall due to:
- Liver disease resulting in a decreased production of albumin (e.g. cirrhosis).
- Inflammation triggering an acute phase response which temporarily decreases the liver’s production of albumin.
- Excessive loss of albumin due to protein-losing enteropathies or nephrotic syndrome.
Prothrombin time (PT): Is a measure of the blood’s coagulation tendency, assessing the extrinsic pathway. (I,II,VII,X) In the absence of other secondary causes such as anticoagulant drug use and vitamin K deficiency, an increased PT can indicate liver disease and dysfunction.
Therapeutics
- Hemo-Bilirubin Metabolism
- Jaundice
 https://next.amboss.com/us/article/Ln0wFg?q=liver+function+tests#Zec7198aab35043cf581b97bde4bf916f
https://next.amboss.com/us/article/Ln0wFg?q=liver+function+tests#Zec7198aab35043cf581b97bde4bf916f
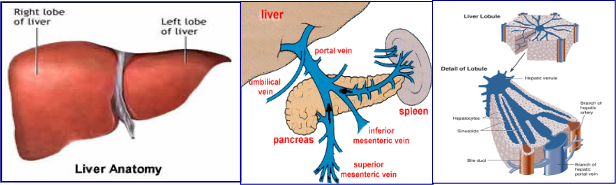
Major Metabolic Functions of the Liver
- Synthetic functions Proteins: plasma proteins albumin, globulins, coagulation factors as prothrombin…etc
Lipids: cholesterol, triglycerides, fatty acids, phospholipids & lipoproteins (VLDL)
Carbohydrates: glycogen synthesis & gluconeogenesis maintain fasting blood glucose
- Detoxification & excretion functions
- Detoxication of ammonia to urea (urea cycle)
- Billirubin conjugation & excretion into bile
- Excretion of cholesterol into bile
- Drug detoxication & excretion into bile (why blood from gut pas through liver before heart)
- Storage Function
- Storage of fat soluble vitamins (vitamins A, D, E & K)
- Storage of vitamin B12
- Digestive Function:
- Production of bile salts
- Help digestion and absorption of lipids and (vitamins A, D, E & K)
Patients with severe hepatic dysfunction are expected to have low plasma urea, low plasma cholesterol ,low glucose, low albumin and high ammonia level
Routine Liver Function Tests (LFTs)
-
plasma proteins mainly Albumin -Chronic
-
Blood Liver Enzymes: parenchymatous and cholestatic
- Alanine amino transferase (ALT) - liver - specific/appear b4 jaundice
- Aspartate amino transferase (AST) - liver - non specific
- Alkaline phosphatase (ALP) -bile nonspecific
- Gamma glutamyl transferase (GGT) bile specific
- 5’-nucleotidase (5’-NT) - Hemolysis
-
Blood Coagulation Factors (Prothrombin) - Acute Prothrombin Time (PT) and INR - Surgery indications
-
Blood Billirubin: see jaundice lecture (total 1 mg%, direct 0.8%& indirect 0.2%)
LFTs can be affected by extrahepatic factors such as nutrition, hemolysis, antibiotic use, systemic illness
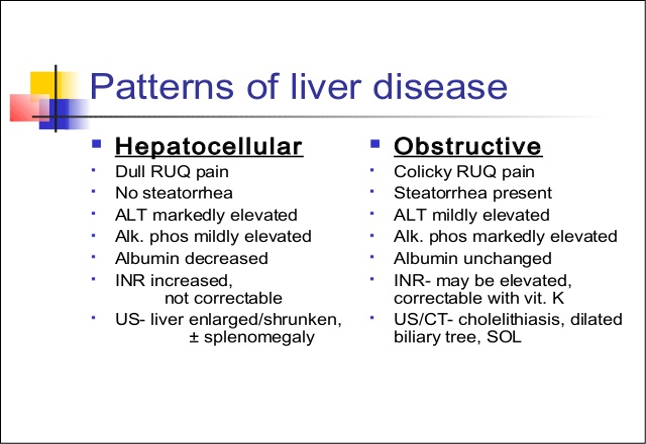 PT ⇒ INR correction - obstructive unchanged due to acute
PT ⇒ INR correction - obstructive unchanged due to acute
- ALT elevated due to extensive death in hepatocellular
- bile salts not present = steatorrhea