Treatment of Bipolar Disorder
Therapies
- Bipolar Depression
- Acute Treatment of Mania, Mixed State, Rapid Cycling
- Bipolar & Pregnancy treatment
Treatment Challenges in Bipolar Disorder
- Often unrecognized
- Often untreated
- Often misdiagnosed
- Often inadequately treated
- Exacerbated by incorrect treatment
Akiskal. J Clin Psychopharmacol.
1996;16(suppl 1):4S-14S.
| Medication | Indications | Key Pharmacology | Major Side Effects | Dosage & Monitoring |
|---|---|---|---|---|
| Lithium | Anti-manic, Anti-depressant, Prophylaxis | Not metabolized, kidney clearance | GI distress, thyroid issues, tremor | Start 300 mg BID, monitor levels |
| Valporic Acid | Mania, Bipolar Depression, Prophylaxis | Metabolized by liver, protein bound | GI distress, hepatotoxicity, weight gain | Start 250 mg BID, levels 350-700 μmol/L |
| Lamotrigine | Depression, Prophylaxis | No blood level monitoring | Rash (Stevens-Johnson syndrome) | Start 12.5-25 mg, increase gradually |
| Carbamazepine | Mania, Bipolar Depression, Prophylaxis | Induces CYP 450, liver metabolism | Diplopia, dizziness, blood issues | Start 100 mg BID, therapeutic levels 17-42 μmol/L |
| Olanzapine | Mania, Depression, Prophylaxis | Weight gain, metabolic changes | 5-20 mg/day | |
| Atypical Neuroleptics | Anti-manic, Anti-psychotic | Varies by medication |
| Category | Bipolar Depression | Acute Treatment of Mania, Mixed State, Rapid Cycling | Bipolar & Pregnancy Treatment |
|---|---|---|---|
| Prevalence & Course | - 20% of Bipolar Depressive Episodes run a chronic course | - Rapid Cycling/Mixed: Divalproex | - Postpartum Risk: >50% risk of an episode - Recommendation: Re-start therapy after delivery |
| Symptomatology & Treatment | - Mild depressive symptomatology may be successfully treated with CBT or IPT | - History and Physical Examination - Labwork: - CBC with diff - Lytes, creatinine - LFT’s - TSH - EKG (if >40) - U/A - Pregnancy test if relevant  | - All mood stabilizers are teratogenic - Risk vs. Benefit |
| Medications | - Lithium - Response rates from 64% to 100%. Level I (A) evidence - Antidepressants - Level I (B) evidence - Watch for flips (more common with tricyclics) - Use with concomitant mood stabilizer to avoid flips - Lamotrigine - Sometimes added to lithium as mood stabilizer - Works better from the “bottom up” - Atypical Neuroleptics - Olanzapine (Level I evidence as monotherapy for acute depression) - Quetiapine (now approved for bipolar depression) | - Monotherapy: Lithium, divalproex, Risperidone, Olanzapine, Quetiapine, Ziprasidone, Aripiprazole - Combination: Lithium or divalproex plus Atypicals, except Ziprasidone (increases response by 20%) - Rapid Cycling/Mixed: Divalproex - Discontinue: Antidepressant, stimulant meds | - Lithium - Lower risk (Ebstein’s anomaly, 0.1%) - Tricuspid valve displacement - Sodium Valproate - Neural tube defects may increase to 5% - Avoid in women of childbearing age, especially weeks 1-10 - Use folic acid 5 mg PO OD - Can do serial ultrasounds examining the neural tube - Lamotrigine - Cleft lip and palate - Possibly less teratogenic - Dosage Adjustments - May need to increase dose during pregnancy, especially lithium - Decrease dose after delivery (re: GFR) - Breastfeeding - All medications secreted through breast milk - Data suggests no immediate risk - No data regarding later behavioral effects - Therapies with Lower Risk in 1st Trimester: ECT, SSRI, Neuroleptics |
| Evidence Levels | - Lithium: 64% to 100% response rates. Level I (A) - Antidepressants: Level I (B) - Quetiapine: Level I | - Olanzapine: Level I evidence as monotherapy for acute depression | - Decision Analysis for Maintenance/Prophylactic Phase: - Costs (e.g., lithium exposure) - Benefits (decreased risk of relapse) |
| Combination Therapy | - Monotherapy: Lithium, lamotrigine, quetiapine - Combination Therapy: - Lithium and divalproate - Olanzapine and SSRI | - Monotherapy: Lithium, divalproex, Risperidone, Olanzapine, Quetiapine, Ziprasidone, Aripiprazole - Combination: Lithium or divalproex plus Atypicals, except Ziprasidone (increases response by 20%) | - Maintenance/Prophylactic Phase: - Mood stabilizers help with moderate-severe illness - Subgroup with mild illness may not need prophylaxis (hard to identify) - 1st Line Treatments for Maintenance: - Monotherapy: Lithium, divalproate, lamotrigine, risperidone LA, olanzapine, quetiapine, aripiprazole - Combination: Lithium or divalproate plus risperidone LA, quetiapine, or ziprasidone |
| First Line Treatments | - Monotherapy: Lithium, lamotrigine, quetiapine - Combination Therapy: Lithium and divalproate, Olanzapine and SSRI | - 1st Line Treatments for Mania: - Monotherapy: Lithium, divalproex, Risperidone, Olanzapine, Quetiapine, Ziprasidone, Aripiprazole - Combination: Lithium or divalproex plus Atypicals, except Ziprasidone (increases response by 20%) - Rapid Cycling/Mixed: Divalproex - Discontinue: Antidepressant, stimulant meds | - 1st Line Treatments for Bipolar II: - Depression: Quetiapine (Level I evidence) - Maintenance: Lithium, Lamotrigine (Level II evidence) - Therapy in Pregnancy: - All mood stabilizers are teratogenic - Lithium lower risk (Ebstein’s anomaly, 0.1%) - If illness not severe, consider planned pregnancy without meds - 4-week medication-free period pre-conception - ECT, SSRI, Neuroleptics all lower risk in 1st trimester |
| Continuation Phase | - If Atypical Neuroleptics were used: - Gradually wean and discontinue unless: - (1) Persistent psychosis - (2) Adjunctive prophylaxis - If antidepressants used: - Once depression has passed, if asymptomatic for 6-12 weeks, gradually wean off over several weeks | - 1st Line Treatments for Mania: - Monotherapy and Combination as above | - Maintenance/Prophylactic Phase: - Mood stabilizers help with moderate-severe illness - Subgroup with mild illness may not need prophylaxis (hard to identify) - Indefinite Maintenance Pharmacotherapy supported by “decision analysis” (costs vs. benefits) |
| Maintenance/Prophylactic Phase | - Risk of recurrence: Uncertain - Mood stabilizers help with moderate-severe illness - Subgroup: Mild illness may not need prophylaxis (hard to identify) - Indefinite maintenance pharmacotherapy supported by “decision analysis”: - Costs (e.g., lithium exposure) - Benefits (decreased risk of relapse) - 1st Line Treatments for Maintenance: - Monotherapy: Lithium, divalproate, lamotrigine, risperidone LA, olanzapine, quetiapine, aripiprazole - Combination: Lithium or divalproate plus risperidone LA, quetiapine, or ziprasidone | - Continuation Phase: Not specifically addressed beyond acute treatment | - Maintenance/Prophylactic Phase: - Mood stabilizers and their benefits vs. costs - Indefinite maintenance pharmacotherapy |
| Use in Bipolar II | - 1st Line Treatments for Bipolar II: - Depression: Quetiapine (Level I evidence) - Maintenance: Lithium, Lamotrigine (Level II evidence) | - 1st Line Treatments for Mania applicable to Bipolar I | - 1st Line Treatments for Bipolar II largely overlap with general bipolar treatment, with specific considerations for pregnancy |
| Images |  |  |  |
The Evolution of Therapies for Bipolar Disorder
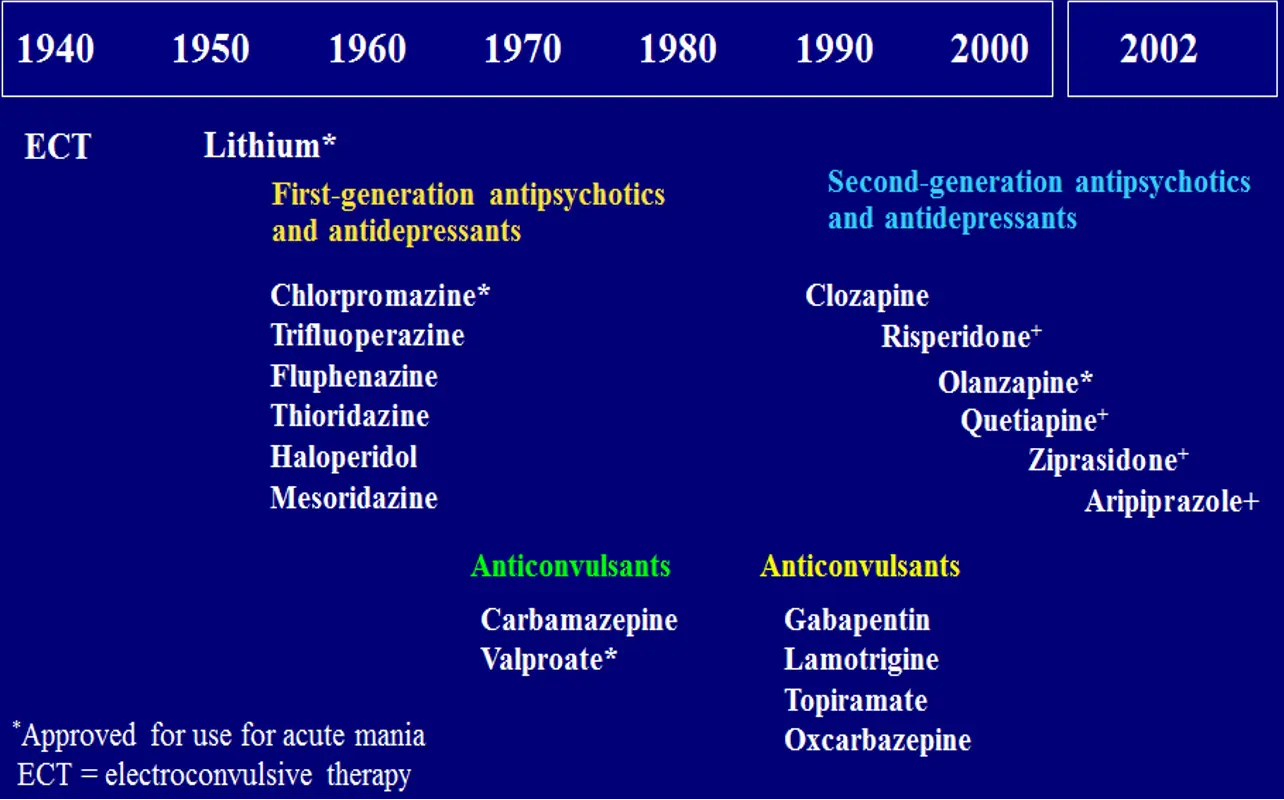
- 1940
- ECT
- 1950
- Lithium*
- 1960
- First-generation antipsychotics and antidepressants
- Chlorpromazine*
- Trifluoperazine
- Fluphenazine
- Thioridazine
- Haloperidol
- Mesoridazine
- First-generation antipsychotics and antidepressants
- 1970
- Anticonvulsants
- Carbamazepine
- Valproate*
- Anticonvulsants
- 1980
- Second-generation antipsychotics and antidepressants
- Clozapine
- Risperidone+
- Olanzapine*
- Quetiapine+
- Ziprasidone+
- Aripiprazole+
- Second-generation antipsychotics and antidepressants
- 1990
- Anticonvulsants
- Gabapentin
- Lamotrigine
- Topiramate
- Oxcarbazepine
- Anticonvulsants
- 2000
- 2002
*Approved for use for acute mania
ECT = electroconvulsive therapy