Difficult Airway Algorithm

OXYGENATION Positive VENTILATION With bag mask No intubation (wasting of time and patient will develop hypoxia)
Physical Examination
- Vital Signs: BP, HR, Spo2, Temp
- BMI: Obesity
- General Look: Signs of trauma, burn, deformity, abnormal movement, airway feature, neck and thyroid goiter, fat distribution, lower limb oedema, skin abnormality or abnormal color, assess for difficult cannulation.
- CVS: S1+S2+ murmur
- Respiratory: Clear or wheezing or decrease air entry, crepitation, transmitted sound, Stridor, Grunting
- Joint or Back Deformity
- CNS: Muscle weakness and power examination
All must be documented.
General Emergency Airway Management
- Learn Technique
- Open Airway
- Mask Bag Ventilation (BLS)
- 100% Oxygen
- Call for Help
- Intubation May Waste Time
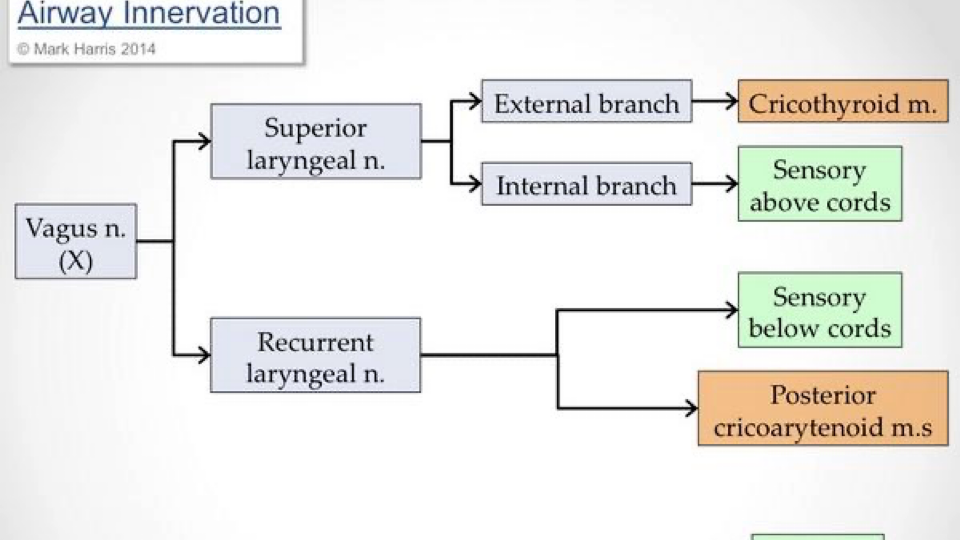
Important Airway Anatomy innervation for awake intubation
The larynx is innervated bilaterally by the superior laryngeal nerve (supplies mucosa from the epiglottis to the level of the cords) and the recurrent laryngeal nerve (supplies mucosa below the cords), both branches of the vagus nerve(CN X).
The recurrent laryngeal nerves supply all of the intrinsic muscles of the larynx except for the cricothyroid muscle and any damage to the recurrent laryngeal can result in vocal cord dysfunction. The cricothyroid muscle is innervated by the external branch of the superior laryngeal nerve. Other nerves which may need to be anesthetized for awake fiberoptic intubations include the maxillary branch of the trigeminal nerve which supplies sensory innervations to the nasopharynx and
the glossopharyngeal nerve which supplies sensory innervations to the post 1/3 of the tongue, pharynx, and areas above the epiglottis.