Inflammatory Optic Neuropathy (Optic Neuritis)
It is caused by a number of underlying conditions:
- Systemic infection.
- Vaccination.
- Autoimmune disease.
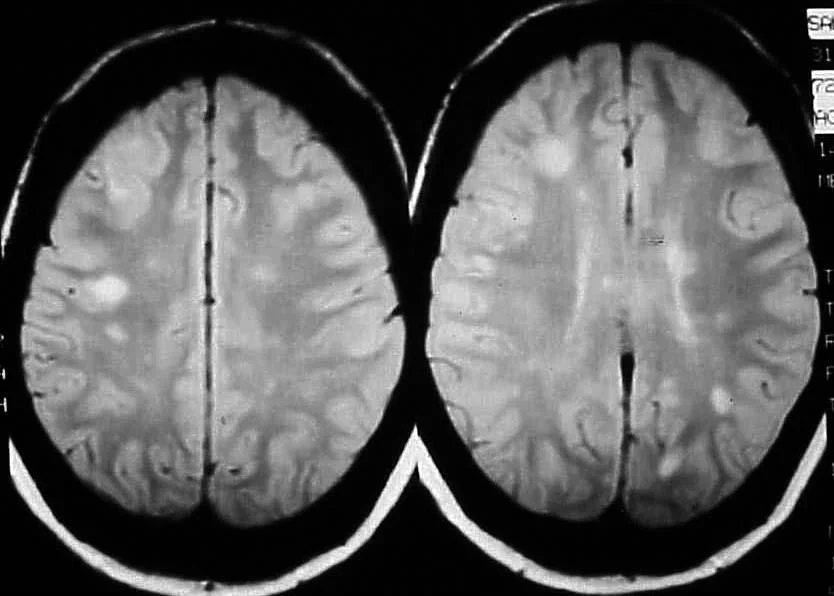
The most commonly associated cause of inflammatory optic neuropathy is demyelinating optic neuritis secondary to multiple sclerosis (MS).
-
A complex cascade of inflammatory events begins peripherally in the body.
-
Activation of T lymphocytes.
-
The activated cells cross the blood-brain barrier and gain access to the central nervous system.
-
The initial inflammatory cascade leads to phagocytosis of the myelin sheath.
-
As a result, gliotic tissue is laid down in place of missing myelin.
-
This substitutive tissue lacks the conduction properties of myelin, leading to nerve impulse interruption.
Multiple Sclerosis
Symptomatology:
-
Patient is typically female, white, age 20 to 40 years.
-
Typically present with mild to moderate ocular pain (exaggerated upon eye movement).
-
Noticeable changes in color vision in the affected eye.
-
Variable unilateral loss of vision, ranging from 20/30 to no light perception.
-
This is often accompanied by an afferent pupillary defect (APD).
-
Visual field defect in form of cecocentral scotomas
Management:
- Intravenous steroid (methylprednisone), administered over the course of three days followed by an 11-day course of oral prednisone.
Signs:
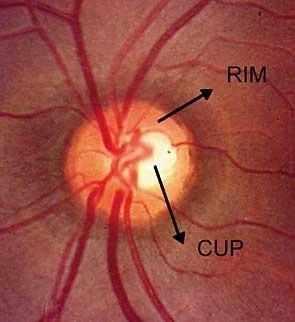
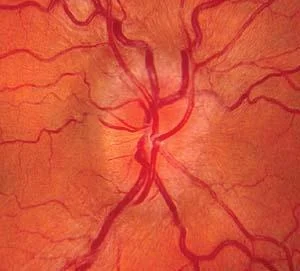
- In acute optic neuritis:
- Disc edema
- Disc hemorrhages
- Segmental or diffuse optic disc pallor
- 2/3 of pts have normal appearance of optic disc.
- Dyschromatopsia, red color desaturation defects
- APD