Congenital Heart Disease
Dr. Mansour Alqurashi
Consultant Pediatric Cardiologist
Objectives
- Describe the clinical features that point to the presence of a congenital heart malformation.
- Describe the general classification of heart diseases in pediatrics.
- Differentiate cyanotic from non-cyanotic heart disease.
- Understand the anatomy and physiology of common congenital cardiac defects.
- Discuss the clinical presentation and outline the management of acyanotic and cyanotic heart diseases.
Fetal Circulation
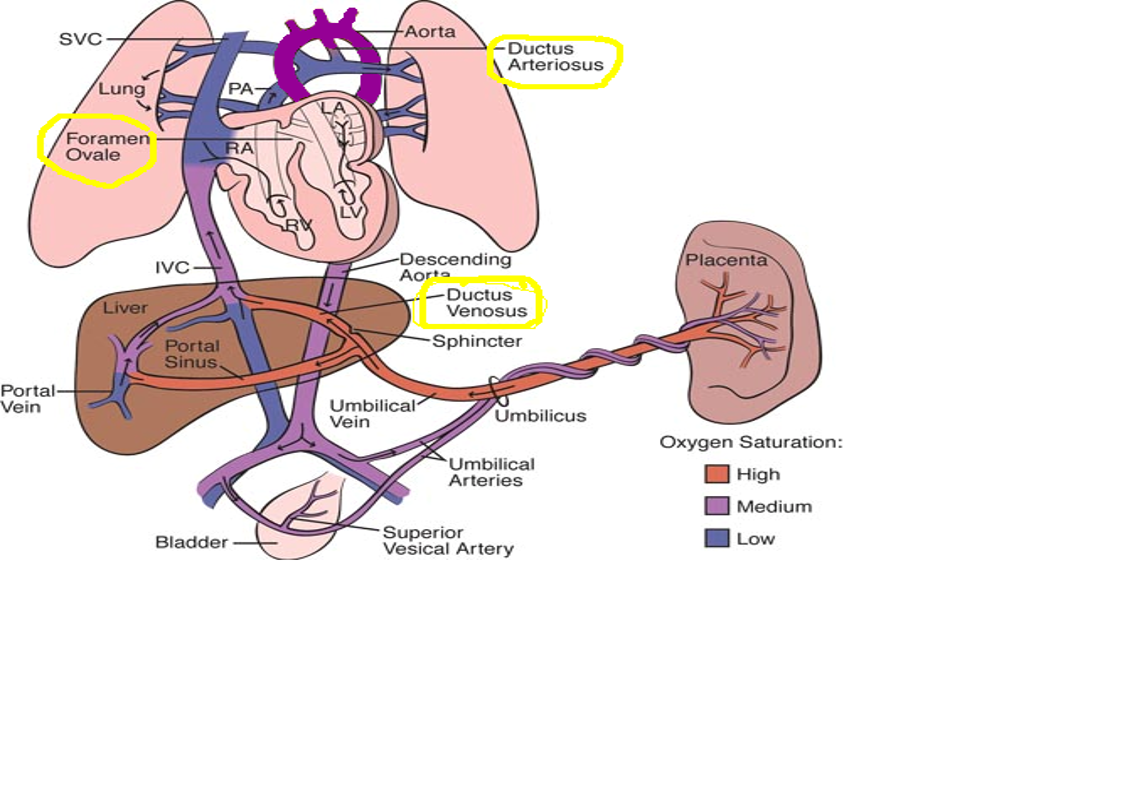
Fetal Shunts
- Foramen ovale: Shunts mixed blood from right atrium to left atrium (hole in the atrial septum).
- Ductus arteriosus: Accessory (extra) artery, shunts mixed blood away from lungs to descending aorta.
- Ductus venosus: Accessory (extra) vein, carries oxygenated blood from umbilical vein into lower venous system.
Common Cardiovascular Disorders in Children
- Congenital Heart Defects
- Congestive Heart Failure
- Acquired Heart Disease
Congenital Heart Disease
- 35 different types
- Common to have multiple defects
- Range from mild to life-threatening and fatal
- Genetic and environmental causes
Classification
Acyanotic Congenital Heart Disease
- Ventricular Septal Defect - ACE / Patching / BAnding
- Atrial Septal Defect
- Patent Ductus Arteriosus - PDA -
- Coarctation of Aorta
- Aortic Stenosis
- Pulmonary Stenosis
- Hypoplastic Left Ventricle
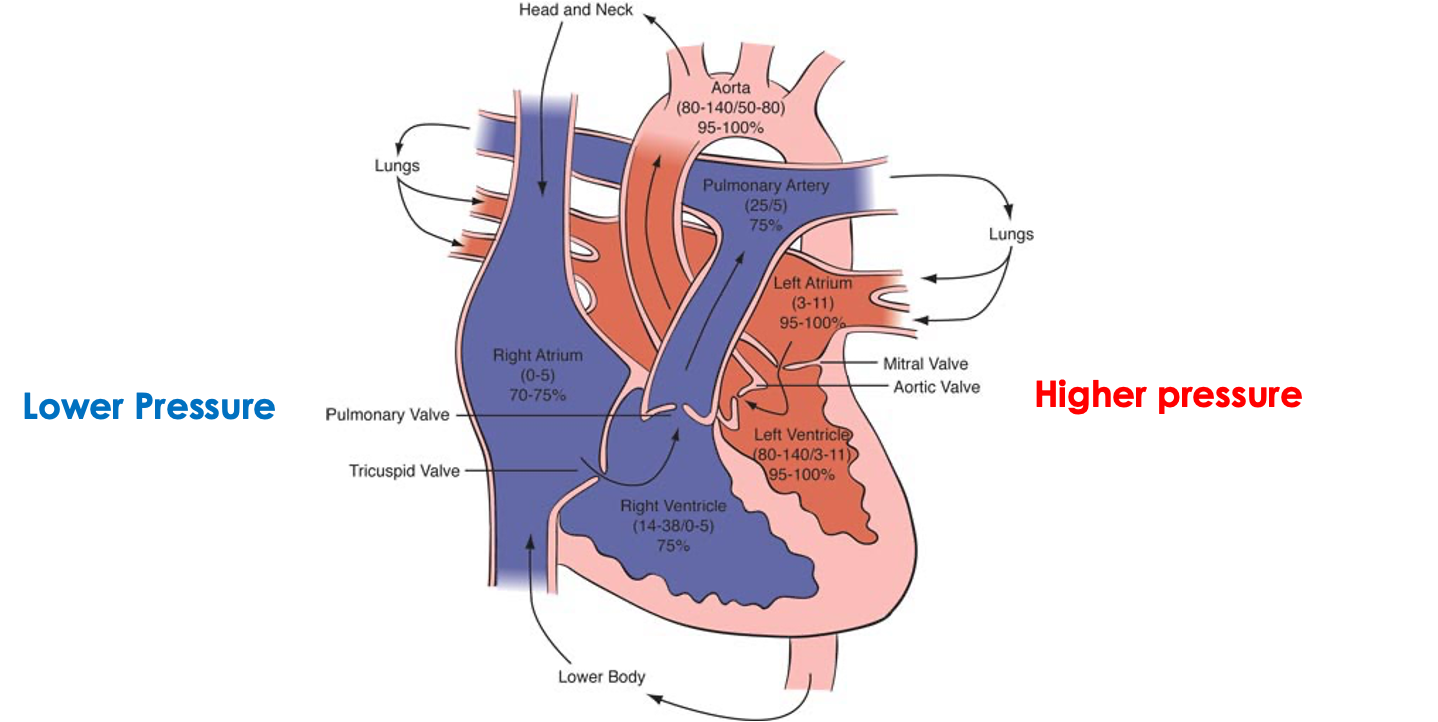
Blood Flows From High to Low Pressure
Cyanotic Congenital Heart Disease
Classification of Cyanosis in Newborn
Central (Best at Tongue): It is blue discolouration of the skin & mucous membranes. - It is detectable when the deoxygenated hemoglobin is more than 5 g/100 ml (capillary). [Oxygen saturation of arterial blood <85%]
- Cardiac
- Pulmonary
- Neuromuscular & C.N.S.
- Persistent Pulmonary Hypertension
- Methaemoglobinaemia
- Pulmonary Arteriovenous Fistula
Peripheral (Fingers & Toes):
- Physiological (Cold)
- Reduced Cardiac Output
Cyanotic Defect
- Tetralogy of Fallot
- D-transposition of great arteries
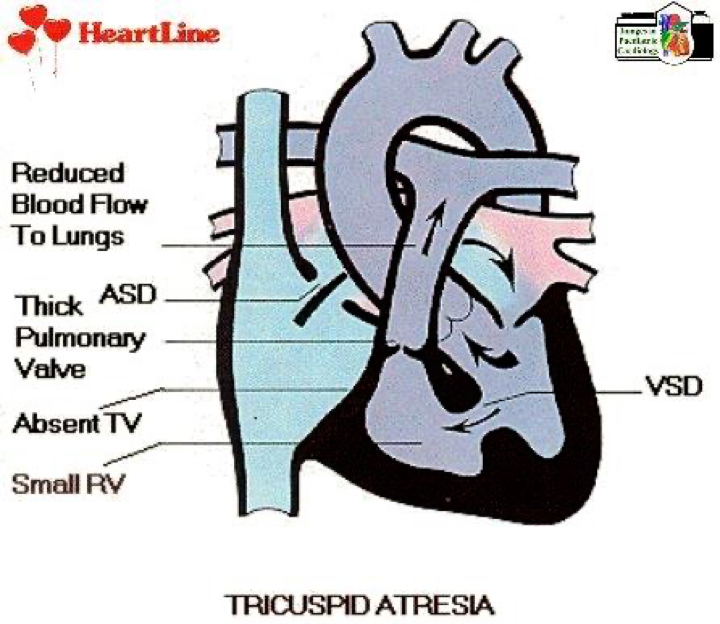
- Tricuspid atresia
Cyanosis causes
- Cyanosis with obstructive pulmonary flow:
- Tricuspid Atresia
- Pulmonary Atresia
- Critical Pulmonary Stenosis
- Ebstein’s Anomaly
- T.O.F.
Shock
- Coarctation of the Aorta
- Critical Aortic Stenosis
- Hypoplastic Left Heart Syndrome (may be acyanotic or cyanotic )
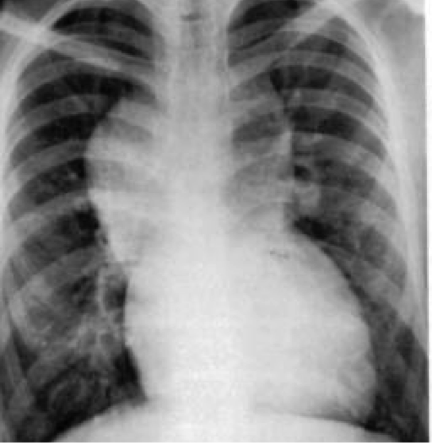
4 Month Old Infant with Heart Failure
- Describe chest x-ray and what is likely diagnosis?
Clinical
Congenital Heart Disease Prostaglandin Indication
-
Cyanotic cardiac lesion with obstruction to pulmonary blood flow:
- Pulmonary Atresia
- Tricuspid Atresia
- Critical Pulmonary Valve Stenosis
- Complex Cyanotic C.H.D.
-
Cyanotic lesions with closed pulmonary recirculation:
- Transposition of Great Arteries
- Total Anomalous Pulmonary Venous Drainage (Obstructive)
-
Acyanotic lesions with obstruction of systemic flow:
- Coarctation of Aorta
- Interruption of Aortic Arch
- Critical Aortic Stenosis
- Hypoplastic Left Heart Syndrome
Congenital Heart Disease Diagnostic Approach
- History
- Examination
- Investigation (Chest X-ray, ECG)
- Hyperoxic Test
- Echocardiography
Congenital Heart Disease Chest X-ray
- Abnormal Heart Size
- Abnormal Heart Position
- Pulmonary Vascular Markings
- Abnormal Heart Shape
- Boat-shaped heart: T.O.F., Tricuspid Atresia
- Egg on side: T.G.A.
- Snowman: T.A.P.V.D.
Congenital Heart Disease Presentation
- Cyanosis
- Cyanosis with distress (Cyanosis with Heart Failure)
- Congestive Heart Failure
- Shock
| Condition | Description | Symptoms | Signs | Treatment |
|---|---|---|---|---|
| Ventricular Septal Defect (VSD) | - Most common CHD. - Defect in ventricular septum. - High Pressure in LV forces oxygenated blood back to RV. - Small defects often close spontaneously in the first 2 years of life while large defects require surgical repair within the 1st year. | - Asymptomatic - Rapid breathing - Excessive Sweating - Poor weight gain - Congestive Heart Failure, usually within 6 to 8 weeks of life if defect is large - Pulmonary Hypertension if defect is large - Eisenmenger’s syndrome | - Depend on the size of the defect - Loud harsh pansystolic heart murmur - Palpable thrill - Parasternal heave (RVH) - Signs of congestive heart failure: tachycardia, tachypnea, respiratory distress (retractions), grunting, difficulty with feeding, diaphoresis, displaced apex beat, and hepatomegaly | - Lasix and Captopril (ACE inhibitors) - Surgery is patching the defect by pericardium or Dacron (open heart surgery with cardiopulmonary bypass) - Pulmonary artery banding to reduce blood flow to lungs if not stable for surgery - Percutaneous Device closure |
| Atrioventricular Septal Defect (ASD) | - Defect in atrial septum - Pressure in LA is greater than RA (blood flows left to right) - Oxygen-rich blood leaks back to RA & RV and is then pumped back to lungs | - Asymptomatic - Large defect may cause symptoms of CHF: - Rapid breathing - Excessive Sweating - Poor feeding, failure to thrive - In adults: - Fatigue and dyspnea on exertion - Palpitations - Syncope - Stroke - Eisenmenger’s syndrome | - Heart murmur resulting from increased blood flow through pulmonary valve (systolic ejection murmur) - Wide and fixed splitting of second heart sound - Parasternal heave (RVH) - Signs of congestive heart failure | - Small defect (less than 5mm), may resolve spontaneously - Medical Management (Lasix, Captopril) for large defects with symptoms of heart failure - Transcatheter devices, such as a septal occluder may be used - Surgical closure is needed for large defects that cannot be closed by Transcatheter devices - Pulmonary artery banding to reduce blood flow to lungs if not stable for surgery |
| Patent Ductus Arteriosus | - Blood flows from aorta to the pulmonary artery, creating a left to right shunt, resulting in left atrium and ventricle overload - Increased pulmonary blood flow can result in pulmonary hypertension and reversal of the shunt, which is known as Eisenmenger’s Syndrome. This results in flow of desaturated blood to the lower extremities. | - Preterm neonate develop CHF and respiratory distress, Full term neonate may be asymptomatic - Infants with Large left to right shunts develop symptoms of congestive heart failure such as tachypnea, tachycardia, poor feeding, and slow growth - Children with small patent ductus are usually asymptomatic | - Continuous murmur heard best at the left sternal border, left subclavicular thrill - Widened pulse pressure and bounding peripheral pulses - Poor growth - Differential cyanosis | - Administration of Indomethacin / nsaids (prostaglandin inhibitor) to stimulate ductus to constrict - Surgical division or ligation of the PDA - Percutaneous device closure by PDA occluder device or coil |
| Coarctation of Aorta | - Constriction of the aorta at or near the insertion site of the ductus arteriosus - Reduces cardiac output - Aortic pressure is high proximal to the constriction and low distal to the constriction - Risk for CVA - Pink Blood - Higher pressure | - Often discovered 3-4 days after birth when the patent ductus arteriosus closes - Symptoms of shock develop very rapidly as no oxygenated blood flows to the lower extremities - Rapid breathing, sweating, and poor feeding often develop during the first week | - Most babies born at term with normal length and weight - Systolic murmur usually heard - Liver may be enlarged - Left arm/leg pulses may be diminished or absent - BP is about 20 mm/Hg higher in arms than in lower extremities - Upper extremity hypertension - Lower extremity cyanosis | - Medical Management (Dopamine, dobutamine, Lasix) - Oxygen - Administration of PGE1 (prostaglandin) infusions, to maintain ductal patency and improve perfusion to lower extremities - although will cause increased pulmonary flow - Surgical repair |
| Pulmonary Stenosis | - | - | - Systolic ejection murmur with a palpable thrill - Right ventricular hypertrophy - Cyanosis from reduced pulmonary blood flow and the right to left shunt of blood at foramen ovale due to high right ventricular pressure - Can lead to right ventricular failure, CHF | - Oxygen - Medical Management (Lasix) - Administration of PGE1 (prostaglandin) infusions, to maintain ductal patency in critical pulmonary stenosis - Pulmonary balloon valvuloplasty via cardiac cath - If unsuccessful, valvotomy |