Pathogenesis of DKA
- A reduction in the net effective concentration of insulin
- Elevation in counter-regulatory hormones:
- Glucagon
- Cortisol
- Growth hormone
- Catecholamines
The main factor in the pathogenesis of DKA is a reduction in the net effective concentration of insulin. And there is usually an elevation in the levels of the counter-regulatory hormones to insulin, which include glucagon, cortisol, growth hormone, and the catecholamines.
Pathophysiology
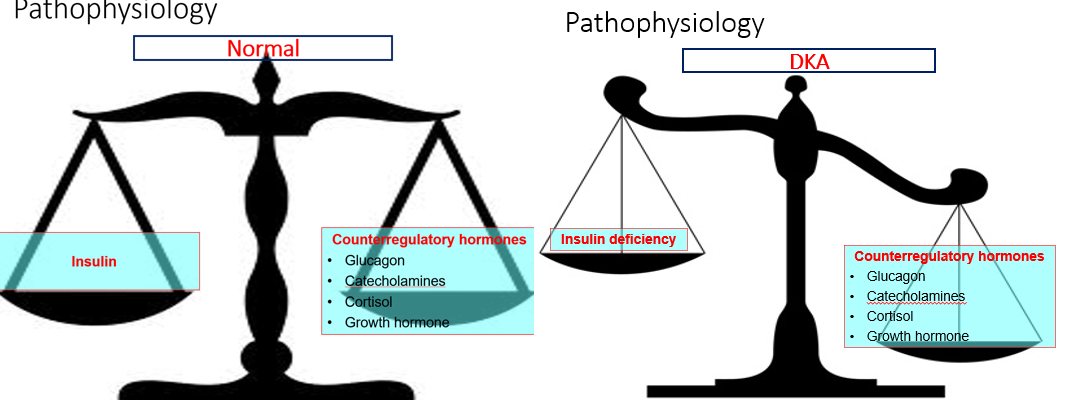 Normal:
Insulin ⇐→ Counterregulatory hormones (Glucagon, Catecholamines, Cortisol, Growth hormone)
Normal:
Insulin ⇐→ Counterregulatory hormones (Glucagon, Catecholamines, Cortisol, Growth hormone)
So in the normal situation, there is usually a balance between the activity of insulin and those of these counter-regulatory hormones.
DKA: Insulin deficiency -⇒ Counterregulatory hormones (Glucagon, Catecholamines, Cortisol, Growth hormone)
And what happens in DKA is that there is a disturbance of this balance by the absolute deficiency of insulin and the increase in concentration of these counter-regulatory hormones.
Definitions
- Gluconeogenesis: formation in the liver of glucose from substrates such as amino acids (from protein breakdown) or glycerol (from fat breakdown).
- Glycogenolysis: breakdown of glycogen in the liver to form glucose.
- Ketogenesis: formation of ketone bodies in the liver from fatty acids.
Before talking about the details of the pathogenesis of DKA, this is a quick reminder of the definition of some terms that are involved in this process.
Gluconeogenesis is the formation in the liver of glucose, which is made from substrates like amino acids that come from the breakdown of proteins and glycerol, which comes from the breakdown of fat.
Glycogenolysis is the term used for the breakdown of glycogen in the liver into glucose.
And ketogenesis is another process that happens in the liver in which ketone bodies are made from fatty acids.
Pathophysiology of DKA
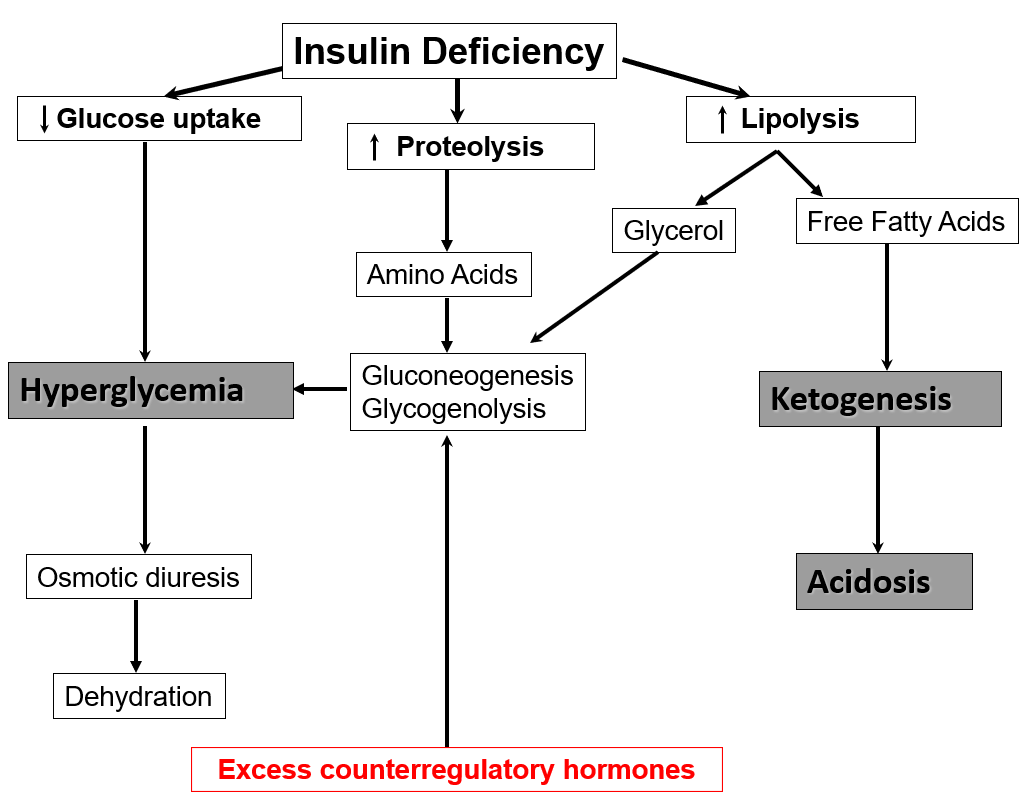
The central mechanism in DKA is the absolute insulin deficiency, which leads to reduced uptake of glucose, increased breakdown of both proteins and fat.
The reduced uptake of glucose into cells leads to excess glucose in blood, which in turn leads to osmotic diuresis leading to dehydration.
The increased breakdown of protein in muscle provides amino acids, which are substrates for gluconeogenesis, exacerbating the hyperglycemia.
Glycerol that comes from the breakdown of fats is also a substrate for increased gluconeogenesis.
While the breakdown of fats also provides free fatty acids, which lead to the production of ketones causing the acidosis.
Lastly, the excess of the counter-regulatory hormones to insulin also contributes to gluconeogenesis and also the breakdown of glycogen in the liver, which again contributes to the hyperglycemia.
Precipitating Causes of DKA
| Cause | Percentage |
|---|---|
| Unknown/poor compliance | 43% |
| Infections | 28% |
| Errors in management | 13% |
| New diagnosis of diabetes | 10% |
| Miscellaneous, e.g., MI | 6% |
What are the actual precipitating causes of DKA? These are results from a study done in Birmingham, and most other studies showed more or less similar results.
In the large majority of cases (that is 43% in this study), there is no actual clear precipitating cause for DKA, but there is always suspicion of poor compliance, especially in younger patients who have difficulty coming to terms with their diabetes.
The commonest identifiable cause for DKA is infections, and this is in about 28%.
Errors in management were identified in 13% of cases.
In 10% of cases, DKA was the first presentation of type 1 diabetes.
And there were miscellaneous causes in 6% of cases, including conditions such as myocardial infarction.
DKA or HHS? & Typical Deficits in DKA and HHS
| Feature | DKA | HHS |
|---|---|---|
| Age | Any | Older |
| Diabetes type | T1D (less common in T2D) | T2D |
| Period of development | Hours | Days |
| Glucose | ++ (usually 350-500 mg/dL) | ++++ (usually >800 mg/dL) |
| Hyperosmolality | + | ++++ (>320 mOsmol/kg) |
| Bicarbonate | <15 | ≥15 |
| pH | <7.3 | ≥7.3 |
| Urinary ketones | Moderate/large | Small/absent |
| Water deficit (L) | 4-10 | 8-15 |
| Element | DKA | HHS |
| Water (ml/kg) | 100 | 100-200 |
| Water (L) | 7 | 10 |
| Sodium (mmol/kg) | 7-10 | 5-13 |
| Chloride (mmol/kg) | 3-5 | 5-15 |
| Potassium (mmol/kg) | 3-5 | 4-6 |
| Comparing DKA with HHS: |
- DKA usually affects younger patients but it can affect any age, whereas HHS usually affects the elderly.
- DKA usually occurs in patients with type 1 diabetes and much less commonly it can be seen in type 2 patients, whereas HHS typically occurs in patients with type 2 diabetes.
- DKA develops quickly over hours and usually within less than 24 hours, but HHS develops over a much longer period of usually several days.
- The degree of hyperglycemia is much more marked in HHS compared with DKA, with the typical glucose levels in DKA between 350 and 500 mg/dL, but in HHS, it is usually more than 800 mg/dL.
- There is some hyperosmolality in patients with DKA from hyperglycemia, but the typical feature of HHS is that the degree of hyperosmolality is much higher and usually more than 320 mOsmol/kg.
- The main dividing factor between the two conditions is the presence of acidosis in DKA and its absence in HHS. So bicarbonate and pH will usually be low in DKA and normal in HHS.
- Ketones when checked in urine are usually in moderate to large amounts in DKA, but the presence of small amounts of ketones in the urine does not actually rule out HHS as these patients may have a small amount of ketones in urine due to starvation.
- Lastly, due to the degree of dehydration, there is usually a much larger water deficit in HHS than in DKA.
- In a patient with moderate DKA, these are the typical estimated deficits. There is dehydration with a typical water deficit of 100 ml/kg, which equates to about 7 liters in a 70 kg patient. With water, there are also large deficits of sodium as well as deficits in chloride and potassium.
Diagnosis of DKA
| Criteria | Level for DKA diagnosis |
|---|---|
| Hyperglycemia (D) | Plasma glucose ≥ 200 mg/dl Or Known diabetes |
| Ketonuria (K) | ≥ 2+ on urine dipstick |
| Acidosis (A) | Bicarbonate < 15 mmol/L And/Or Venous/arterial pH < 7.3 |
-
All patients with T1D who present unwell, dehydrated, or with osmotic symptoms should be investigated for DKA.
-
If facilities are limited, check plasma glucose and urine dipstick for ketones.
-
If facilities allow, do venous blood gas for pH and bicarbonate.
-
Arterial blood gas is only needed in critically ill patients (oxygen saturation <90%, hypotension, or reduced level of consciousness).
We should always have a low threshold for suspecting DKA in patients with type 1 diabetes. So if these patients present with being unwell, dehydrated, or they have osmotic symptoms, they should be investigated to rule out DKA.
The investigations, of course, will depend on what facilities are available, but the priority is to do plasma glucose and to do a urine dipstick to look for ketones.
If facilities allow, then doing a venous blood gas to check pH and venous bicarbonate can exclude or confirm acidosis.
In most patients, an arterial blood gas will not be needed; this is only needed in patients who are critically ill, such as those with hypoxia with oxygen saturation of less than 90%, those with hypotension, or with reduced level of consciousness.
For the diagnosis of DKA to be made, 3 criteria must be fulfilled: all three will need to be present, so you need the D (for diabetic) or the hyperglycemia, you need the K (for ketones in urine), and you need the A (for the acidosis).
Hyperglycemia (D): This is defined as a plasma glucose of usually more than 200 mg/dl; however, in any patient who is known to have diabetes, if other features are present, even glucose levels lower than this may be associated with the so-called euglycemic diabetic ketoacidosis.
Ketonuria (K): The other criterion is the presence of ketones in urine, which is identified by the presence of 2 crosses or more of ketones on urine dipstick testing.
Acidosis (A): And the third criterion is to demonstrate the presence of acidosis by showing either a plasma bicarbonate level of less than 15 mmol/L or venous or arterial pH of less than 7.3.
Ketones
-
Beta-hydroxybutyrate
-
Acetoacetate
-
Acetone
-
The nitroprusside test used in urine test strips detects acetoacetate and acetone but not beta-hydroxybutyrate.
-
Beta-hydroxybutyrate is the predominant ketone in DKA.
-
Ketoacidosis may be present without detectable urinary ketones.
-
Blood ketone testing detects beta-hydroxybutyrate.
-
Blood ketone testing (if available) may enable early identification of DKA.
-


A few words about ketones: There are three ketone bodies: beta-hydroxybutyrate, acetoacetate, and acetone.
The most commonly used test for ketones in urine is the nitroprusside test, which is used in the urine test strips. This test detects two ketone bodies in urine, acetoacetate, and acetone, but it does not detect the third ketone body, which is beta-hydroxybutyrate.
This is an important limitation of the nitroprusside test because beta-hydroxybutyrate is the predominant ketone in cases of DKA.
And for this reason, it is possible to have DKA with negative ketones in urine.
Blood ketone testing: And because of this limitation of the nitroprusside test, a blood test that can detect beta-hydroxybutyrate in blood has been developed. Unfortunately, this test is more expensive and is not widely available, but if it can be done, it can be very helpful because it makes it possible to identify DKA early as well as follow patients during treatment with serial testing for plasma beta-hydroxybutyrate.
The Anion Gap
- Sodium – (Chloride + Bicarbonate)
- Normal range: 7-10 mmol/L
- High anion gap metabolic acidosis: >10 mmol/L
Differential diagnosis:
- DKA
- Lactic acidosis
- Salicylate poisoning
- Ethylene glycol ingestion
- Alcoholic ketoacidosis
Beware of Euglycemic DKA
- Plasma glucose < 250 mg/dL
- 10% of cases of DKA
- More in pregnancy
- Poor oral intake
- Partial treatment with insulin
- Use of SGLT2i
It is important to be alert to this condition called Euglycemic DKA. It is defined as DKA with the plasma glucose less than 250 mg/dL. This can be the situation in 10% of cases of DKA. It occurs more in pregnancy and also when there is poor oral intake. In those who have received partial treatment with insulin. And it has been associated with the use of the SGLT2 inhibitors.
History
- Thirst and polyuria
- Nausea / vomiting
- Abdominal pain

Physical Examination
- Tachycardia/hypotension
- Tachypnea
- Kussmaul’s respiration (air hunger)
- Dehydration
- Ketotic breath
- Confusion/coma
Typically in DKA, there is a history of the osmotic symptoms of thirst and polyuria. Nausea and vomiting are common, and some patients have abdominal pain.
On examination of these patients, there is usually tachycardia, and some patients may have hypotension. There is usually a rapid respiratory rate, and some patients may have what is called Kussmaul’s respiration or air hunger. There will be signs of dehydration. Some patients may have the smell of ketotic breath. And there may be impairment of consciousness with confusion, and some patients may present in a coma.
Investigations
Immediate for diagnosis:
- Capillary blood glucose
- Venous pH/bicarbonate
- Urine ketones
 The investigations that are needed immediately to make the diagnosis include a capillary blood glucose using a glucometer. Venous blood for pH or venous bicarbonate to confirm the acidosis. And testing the urine with a dipstick to check for ketones.
The investigations that are needed immediately to make the diagnosis include a capillary blood glucose using a glucometer. Venous blood for pH or venous bicarbonate to confirm the acidosis. And testing the urine with a dipstick to check for ketones.
Urgent for assessment and treatment:
- Plasma glucose
- Creatinine, urea, sodium, and potassium
- Complete blood count
- Midstream urine
Other investigations that are also important urgently include:
- A laboratory plasma glucose done to confirm hyperglycemia.
- Plasma creatinine, urea, sodium, and potassium.
- A complete blood count, mainly to look at the white blood cell count.
- A midstream urine sample to check for infection.
And doing HbA1c will also be helpful as it gives an idea about diabetes control before the acute episode.
Other tests to be considered (if indicated):
- Blood film for malaria
- Urine culture
- Blood culture
- HbA1c
- ECG
- Chest X-ray
Other tests that may be needed in some cases, depending on the circumstances, are:
- A blood film for malaria.
- Culture of urine and blood to look for infection.
- An ECG, and some patients may need a chest X-ray to look for evidence of chest infection.
Management of DKA Z
- IV fluids
- IV (or SC) insulin
- Potassium replacement
- Treatment of precipitating cause
- Transition to subcutaneous insulin
These are the elements of management of DKA: And I will look at each of them individually. They include:
- First resuscitation with intravenous fluids.
- Ideally, insulin should be given by intravenous infusion, but if facilities are not available, it can be given subcutaneously.
- Replacing potassium.
- The underlying cause for DKA should be identified and treated.
- Regular fetal assessment should be performed.
- When the DKA has resolved, there should be a transition to subcutaneous insulin.
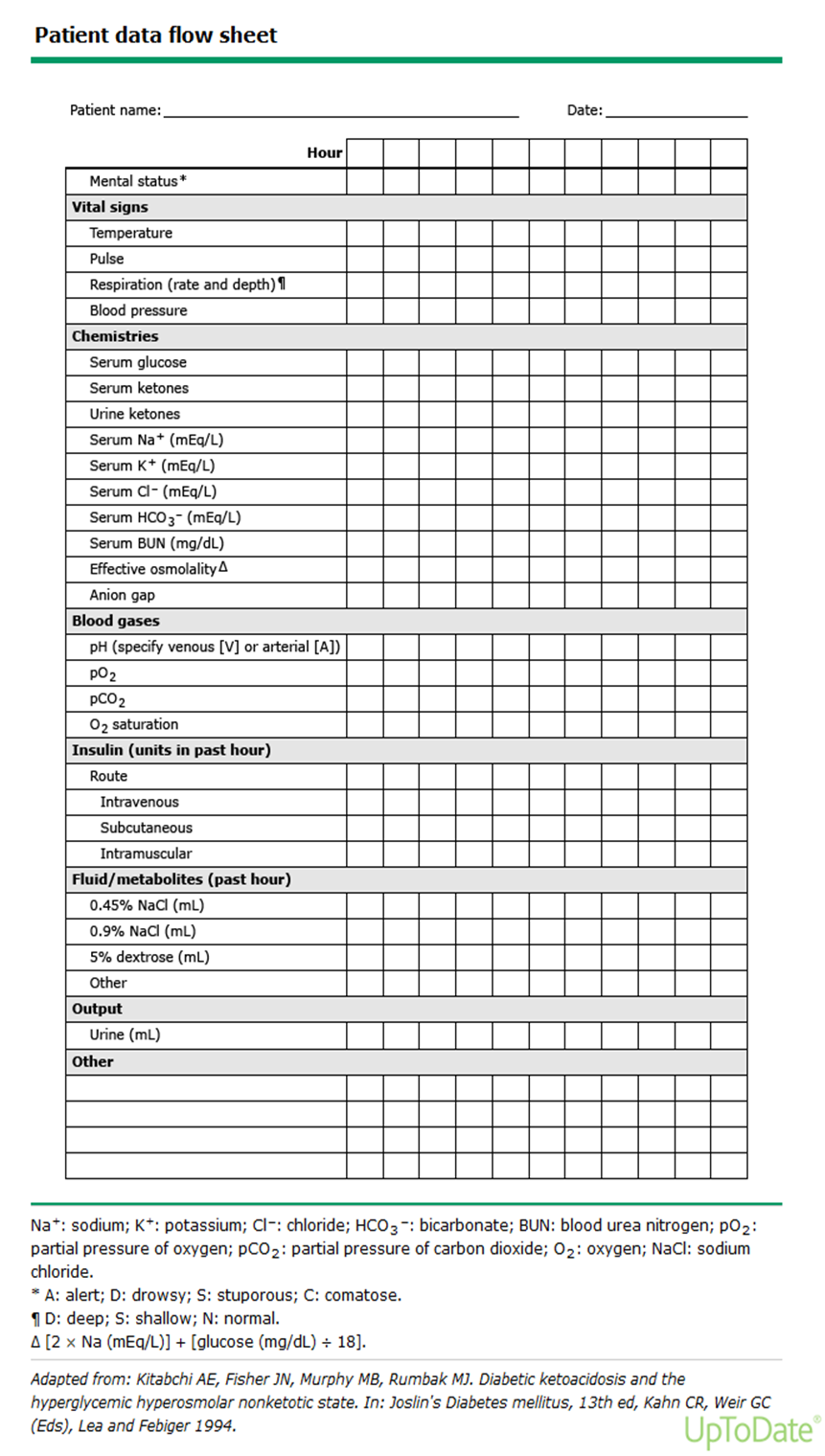
Monitoring
Hourly:
- Pulse
- BP
- RR
- Fluid input/output
- Capillary glucose
Four Hourly:
- Potassium
- Bicarbonate
- Urine dipstick for ketones
Regular monitoring of the patient includes checking hourly the pulse rate, blood pressure, respiratory rate, fluid input and output, and capillary glucose.
While potassium, venous bicarbonate level, and urine dipstick for ketones should be checked at least every 4 hours.
Indications for Admission to ICU
(dependent on available facilities)
- Bicarbonate < 5 mmol/L
- pH (venous or arterial) < 7.0
- Glasgow coma scale < 10
- Systolic BP < 90 mmHg
The criteria for admission to ICU are, of course, subjective and will always depend on what facilities are available. So generally speaking, patients who have severe DKA and may be considered for ICU treatment include:
- Those who have a very low bicarbonate of less than 5 mmol/L.
- Those who have a very low pH at less than 7.
- If the Glasgow coma scale is low at less than 10.
- And if systolic blood pressure is less than 90 mmHg.
IV Fluids
Aims:
- Correct hypotension by restoring circulatory volume
- Clearance of ketones
- Correct electrolyte imbalance
Fluid of choice:
- 0.9% normal saline is the fluid of choice.
- If normal saline is not available, Ringer’s lactate is an acceptable alternative.
- When glucose reaches 250 mg/dL, change to 10% dextrose.
- For euglycemic DKA: replacement fluid should be dextrose 10%.
Composition of IV Fluids
| Element | 0.9% sodium chloride (Normal saline) | Ringer lactate (Hartmann’s solution) |
|---|---|---|
| Sodium | 150 | 131 |
| Chloride | 150 | 111 |
| Potassium | 0 | 5 |
| Lactate | 0 | 29 |
| Calcium | 0 | 2 |
Suggested Guide for Rate of IV Saline Infusion 3L over 3hr 5L over 1st 13hr
| Element | Rate ml/hour |
|---|---|
| 1st liter | 1000 (over 1 hour) |
| 2nd liter | 500 (over 2 hours) |
| 3rd liter | 500 (over 2 hours) |
| 4th liter | 250 (over 4 hours) |
| 5th liter | 250 (over 4 hours) |
Total: 5 liters over first 13 hours On average, 5 litres will be given over the first 12 to 13 hours
Adjusting Fluid Rate:
-
If systolic BP < 90 mmHg, give 500 ml saline over 10-15 minutes.
-
Repeat if systolic BP still < 90 mmHg.
-
Slower rates of infusion in:
- 18-25 years
-
70 years
- Pregnant ladies
- Cardiac or renal failure
The most important therapeutic measure in the treatment of DKA is IV fluid replacement. And the aims of this include:
- First, to correct the hypotension by restoring the circulatory volume.
- To clear the ketones.
- And to correct the electrolyte imbalance.
The fluid of choice for IV fluid replacement is normal saline. If, for any reason, normal saline is not available, then Ringer’s lactate is an acceptable alternative. One liter of this solution contains 131 mmol of sodium, 111 mmol of chloride, and 5 mmol of potassium, which means it is close to the composition of normal saline.
When glucose goes down to 250 mg/dL, the fluid should be changed to 10% dextrose; this can be in addition to continuing saline if it is felt that more IV fluids are needed.
For patients who present with euglycemic ketoacidosis, where the presenting sodium is not high, the fluid given should be dextrose 10% to allow giving insulin and avoid hypoglycemia.
This is a suggested guide for the rate of IV fluid replacement, which may be suitable for most adult patients with DKA. One liter should be given over one hour. Then 2 liters to be given over 2 hours each. And then 2 liters to be given over 4 hours each. On average, 5 liters will be given over the first 12 to 13 hours.
These are just a general guide for the average patient. But judgment and clinical assessment should be used to decide on the rate of fluid to be given, so some patients may need more quick and aggressive fluid replacement, while others may need more gentle and slow fluid replacement.
Potassium Replacement
- Hypokalemia may cause cardiac arrhythmias.
- In spite of potassium deficit, serum potassium on admission is usually normal.
- Aim to maintain potassium 4-5 mmol/L.
If plasma potassium result available quickly on admission, follow table below:
| Serum potassium | Potassium chloride/liter fluid |
|---|---|
| > 5.5 mmol/L | Give saline with no added KCl |
| 3.3 - 5.5 mmol/L | Add KCl 20 mmol to each 500 ml bag of saline |
| < 3.3 mmol/L | Add KCl 20 mmol to each 500 ml bag of saline and: consider increasing the rate of infusion if fluid balance allows; withhold insulin until potassium ≥ 3.3 |
If plasma potassium result not available on admission:
- The first 2 bags of 500 ml saline should be without added potassium.
- When potassium result known, follow the previous table.
Replacing the potassium deficit is a crucial part of management because hypokalemia may cause cardiac arrhythmias, which sometimes can be life-threatening. It is important to remember that in spite of the overall potassium deficit, when we measure serum potassium on admission, it may be normal. The aim of potassium replacement is to maintain the serum potassium at a level of between 4 and 5 mmol/L.
If we can get a plasma potassium done and the result available quickly, we should follow these recommendations from the joint British societies guideline for the management of DKA.
If the potassium level on admission is more than 5.5 mmol/L, no potassium is added to the saline fluid.
If the level is between 3.3 and 5.5 mmol/L, 20 mmol of potassium chloride should be added to each 500 ml bag of normal saline.
And if potassium is very low at less than 3.3 mmol/L, two measures should be taken: first, we should consider increasing the rate of the infusion of the fluid containing potassium. And in this situation, also, insulin should be withheld until the potassium has risen to above 3.3 mmol/L as giving insulin will cause further lowering of potassium, which can cause life-threatening arrhythmias.
In case the plasma potassium result is not available on admission, the safe course of action is to give the first two bags without added potassium. And once the result of potassium is known, then one can follow the recommendations in the table I just showed.
Insulin Therapy
If syringe infusion pump available:
- Add 50 units of soluble human insulin (e.g., Actrapid) to 50 ml normal saline; this gives a concentration of 1 unit/ml.
- This should be infused into a separate IV line, and the solution should be changed every 6 hours.
- Infuse at a fixed rate of 0.1 unit/kg/hour, based on estimating the patient’s weight (e.g., 8 units/hour in an 80 kg person).

Now coming to insulin therapy for DKA. And here again, the recommendation to follow will depend on whether a syringe infusion pump is available, which is the ideal situation, or whether it is not available.
If a syringe infusion pump is available, then insulin should be given by IV infusion. The insulin used for IV infusion is usually soluble insulin, and this is prepared by adding 50 units to 50 ml of normal saline, which gives a concentration of 1 unit per ml. This should be given through a separate IV line to that used for the IV fluid replacement, and the solution should be changed at least every 6 hours. The infusion should be at a fixed rate of 0.1 unit per kilogram per hour, which can be based on estimating the patient’s weight, so for example, an 80 kg person can have the insulin infusion at a rate of 8 units per hour.
If syringe infusion pump is not available:
- Give a subcutaneous injection of soluble human insulin (e.g., Actrapid) at a dose of 0.1 unit/kg every hour (or 0.2 units/kg every 2 hours).

With both IV or SC regimes:
- Long-acting basal insulin analogs (glargine or detemir) should be continued.
If a syringe infusion pump is not available, the alternative method is to give insulin through the subcutaneous route. And here the soluble human insulin should be given at a dose of 0.1 unit per kilogram every hour or alternatively, it can be given every 2 hours at a dose of 0.2 units/kg every 2 hours. And with both the IV and the SC regimes, it is now recommended that patients who are on long-acting basal insulin analogs should continue to have these insulins as they provide a background insulin supply that will be helpful after recovery from DKA.
- Aim to reduce plasma glucose gradually by 55-90 mg/dL/hour.
- If the drop of plasma glucose is less than 55 mg/dL/hour: increase insulin (IV or SC) dose by 1 unit/hour every hour until the target is achieved.
- If K < 3.3 mmol/L, withhold insulin until K ≥ 3.3 mmol/L.
A reasonable drop in plasma glucose to aim for is a reduction by 55 to 90 mg per dL every hour. And if the drop is less than 55 mg per dL per hour, then the rate of insulin given, either IV or subcutaneously, should be increased by 1 unit per hour every hour until the target is achieved. And again, a reminder about this important point, which is that if the potassium level on admission is very low at less than 3.3 mmol/L, insulin infusion may actually worsen the hypokalemia leading to arrhythmias, and therefore insulin infusion in these cases should be withheld until potassium has risen to above 3.3 mmol/L.
Signs of Satisfactory Progress
- Venous bicarbonate should rise by 3 mmol/L/hour.
- Capillary glucose should fall by 55 mg/dL/hour.
- Target plasma glucose: 110-250 mg/dL.
The targets to be achieved during treatment of DKA are first:
- Venous bicarbonate should rise by 3 mmol per liter per hour.
- And capillary glucose should fall by 55 mg per deciliter per hour.
- The target plasma glucose to aim for in DKA is a level of between 110 and up to 250 mg per dL.
Bicarbonate
- Rarely necessary and usually if pH < 6.9.
- Should be given very cautiously, only in ICU.
All guidelines agree that bicarbonate is rarely necessary as the acidosis can be corrected by IV fluids and by insulin. The American guideline advises at least considering giving bicarbonate when the pH is very low at less than 6.9. If it is given, this should be done very cautiously, and this should usually be in an intensive care unit setting.
Treatment of Precipitating Cause
- Detailed history and examination to direct investigations for cause.
- Omission of insulin is a common cause (history).
- Investigate as appropriate for infection; fever is not necessarily present.
- Raised WBC up to 15,000 is common with DKA without infection.
It is also important to address the underlying cause for DKA. And here it is important to take a detailed history and perform an examination so that investigations can be directed appropriately. We should also remember that one of the commonest causes for DKA is omission of insulin, and here the education of the patient is very important to avoid this happening again. When we are thinking about infection, we should remember that fever is not necessarily present in these cases. And it is also important to remember that a raised white cell count does not necessarily represent infection as it may be caused by excess cortisol and catecholamines.
Resolution of DKA
Defined as:
- pH > 7.3 and/or bicarbonate > 18 mmol/L.
- The patient is eating and drinking.
*When DKA has resolved, the patient should be converted to subcutaneous insulin, and the resolution is defined when these criteria are satisfied:
- The pH rises to above 7.3 or the bicarbonate has risen to above 15 mmol per liter.
- And the patient should be able to eat and drink.
Disappearance of ketonuria is not a condition for resolution of DKA: Acetone may remain positive in urine up to 36 hours after the resolution of DKA and clearance of the main ketones, beta-hydroxybutyrate, and acetoacetate.
Here it is also important to point out that we do not put clearance of ketones from urine as a condition for resolution of DKA. And this is because acetoacetate is usually converted to acetone, which is cleared slowly in urine, and for this reason, acetone may remain positive in urine for up to 36 hours after the clearance of the other main ketones, acetoacetate, and beta-hydroxybutyrate.
Management of the Recovery Period from DKA
- Restart usual insulin regime.
- For newly diagnosed diabetes, start basal-bolus insulin at a total dose of 0.5-0.7 units/kg/day.
- Give first SC rapid-acting insulin before the next meal and discontinue IV insulin one hour later.
When the DKA has resolved, the patient’s usual insulin regime should be restarted. For those who are newly diagnosed with diabetes, they should be started on a basal-bolus insulin regime; a usual starting dose is 0.5 to 0.7 units per kilogram per day. And because the half-life of the soluble insulin given intravenously is very short, the first subcutaneous dose of soluble insulin should be given before the next meal, and the IV insulin should be continued for at least an hour before it is stopped.
Complications of DKA
- Hypokalemia and hyperkalemia: Can be life-threatening. Avoid by regular monitoring and careful potassium replacement.
- Hypoglycemia: Avoid by giving dextrose 10% when glucose reaches 250 mg/dL.
- Cerebral edema: Usually in children and adolescents. Avoid by cautious fluid replacement in young patients.
Complications that can occur during treatment of DKA include:
- First, potassium abnormalities, hypokalemia, and hyperkalemia. And these can be quite serious and life-threatening. But they can be avoided by monitoring potassium regularly and replacing it carefully.
- Hypoglycemia can be avoided by giving dextrose 10% when the glucose levels start to drop and reach a level of 250 mg/dL.
- Lastly, cerebral edema, which usually occurs in children or adolescents and is thought to occur when fluid is given too aggressively, can be avoided by giving replacement fluids gently and carefully in the younger patients.
Prevention of DKA
- Educate patients and provide written sick day rules.
- Provide sticks for urine ketone testing and educate on management of ketonuria.
- Warn about potential insulin ineffectiveness, e.g., from expired insulin.
After treatment of the acute episode, one should consider prevention of further episodes of DKA. Any gaps in the patient’s education should be identified, and they should be re-educated, especially about the sick day rules, which I will come to in the next slide. If possible, patients should be provided with sticks for urine ketone testing, and they should be educated on what to do if urine ketones are positive. They should also be alerted to check for the effectiveness of their insulin, for example, by checking the expiry date to make sure it is not expired.
Sick Day Rules:
- Continue your insulin when you are not feeling well
- If vomiting, check glucose levels more frequently
- Take small amounts of carbohydrates in liquid form with short-acting insulin
- Seek help early if you continue to feel unwell
*Patients with type 1 diabetes, in particular, should be reminded about the sick day rules. A very common mistake that patients with type 1 diabetes make is that they stop taking their insulin when they are unwell and not eating for fear of hypoglycemia. It should be stressed to them that they should not stop their insulin when they are not feeling well. If they are vomiting, they need to do more frequent glucose monitoring. It can be helpful for them to take carbohydrates in a liquid form and in small amounts and more often. But if they continue to feel unwell, they should not delay seeking help.