History
Framework
- Demographics (Name, Age, Gender, Nationality, Martial, Residency)
- Chief of complaint (Cause of hospitalization + days)
- HOPI (OPERATES NON PAIN | SOCRATES PAIN)
- B-Symptoms
- Systemic Review
- Past history (medical, surgical, medication, allergies, family, social)
- summary
- differential + justify differential
- investigations - appropriate
- treatment - suggestive
Introduction, explain, Permission, Assure privacy, chap. Greetings im Mohammed 5th year medical student; could you tell me your name..“amm ahmad”. im here to take your full history, may i proceed? =-
call nurse, assure privacy.
60 years old male, known case of diabetes mellitus, presented to Emergency Department complaining of fever and Foot discharge.
1) Demographics
venous and lymphatic vascular manifestations more common in females + raynauds
Beurger’s Disease (male + smoker + young <45 age - distal extremities abscence of DM or hyperlipidemia)
2) Chief of Complaint
…
3) HOPI
OPERATES OR SOCRATES
I- Site
Right proximal toe
Venous venous ulcers 70% above malleolus
II- Onset/Progression
Course of the ulcer since appearance (size, shape, discharge, if healed and broken down now)
III- Character
numbness, painful
Chronic Ischemia Cramp like pain felt over muscle - reproducible
Venous Commonly painful varicose veins are dull pain, no pain during rest or early in morning.
IV- Radiation
…
V- Associated Symptoms
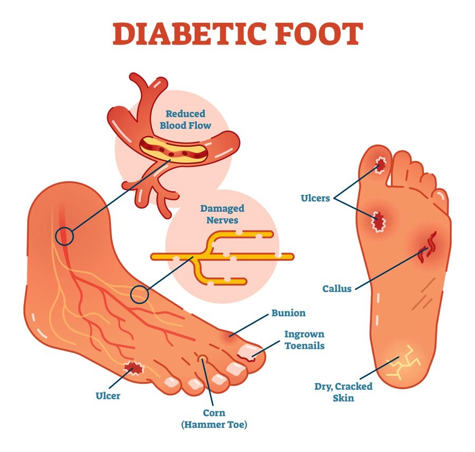
Diabetes
- Associated Sx?(fever, sensation changes) Any other ulcers elsewhere?
Peripheral
- Symptoms indicating vascular disease elsewhere
- Chest pain
- Fainting
- Weakness in limbs
- Paresthesia
- Blurring of vision
Acute ischemia - Five “P” of Acute Ischemia
- Pain
- Pallor
- Pulseless
- Paresthesia
- Paralysis
Chronic ischemia - Five “P” of Acute Ischemia
- claudication
- Gangrene, ulcer formations (chronic nature)
- Hair, nail, skin detioration (chronic nature)
-
- 5 Ps
- Rest Pain
Rest Pain is the pain felt even at rest. It is due to the Ischemia of the somatic nerves(cry of the dying nerves)
- Felt in the foot (most distal parts)
- Exacerbate on lying down or elevation of foot
- Worse at night; patient sits in “hen-holding” position
- Pressure of even bed clothes worsens the pain
- Lessened by hanging the foot down or sleeping on a chair as the gravity aids in the blood flow to the nerves.
- Patient may commit suicide
VI- Timing/Episode
…
VII- Relieving/ Exacerbating Factors
-
Aggravating factors: Ischemia activity
-
Relieving factors: Chronic Ischemia Taking rest
Venous foot elevation
VIII- Severity
…
4) B Symptoms
…
5) Systemic Review
- nephropathy
- retinopathy
- microangiopathy
6) Past Hx
Past medical / Surgical / Family
- DM, HTN. Neuropathic diseases, dyslipidemia
- DM controlled? (since? medication on? Following with endocrinology? Diet?)
- previous truama / burn / bare foot / surgeries-interventions; amputations
- Family members may suffer form vascular disease
Pregnancies, obesity, prolonged standing in varicose veins
Medications / Allergies
- Any Tx had been suggested or administered?
Social smoker
7) Summary
8) Differential, Impression, most likely diagnosis
Diabetic foot
Arterial Conditions
-
Acute Ischemia
-
Chronic Ischemia
-
Thoracic Outlet Syndrome
-
Raynaud’s Disease
-
Beurger’s Disease
-
Gangrene
Common venous diseases:
-
Varicose veins.
-
Deep venous thrombosis. (DVT)
-
Superficial thrombophlebitis.
-
Venous ulcer
Lymphatic disease
- Lymphangitis (infection): Pain, swelling of acute onset
- Lymphedema: Chronic extremity swelling
- Absence of renal, cardiac, abdominal and venous diseases helps in the diagnosis of lymphedema
9) Investigations
Diabetic Foot
- Blood test (CBC, KFT, Alb, C-RP, ESR, culture)
- Wound Culture
- X-ray
- periosteal reaction / elevation
- cortical irregularity / thickening
- Demineralization, osteopenia
- MRI
- ABI
- Angiography
Peripheral vascular diseases
- CBC
- Sample
- Urine
- Doppler / Dopplux / angiography
10) Treatment Plan
Treat the participating factor
Diabetic foot Patient education
- Wear comfortable, supportive footwear
- Avoid walking ‘barefoot’
- Wash the feet once a day in warm (not hot) soapy water
- If the skin is dry, use a regular emollient to reduce risk of fissuring
- Never fail to remove a foreign body from the shoe immediately after it is noticed
- Do not warm the feet using hot water bottles or by direct contact with a radiator
- Never attempt to ‘self-manage’ callosities using sharp paring instruments
- Do not apply adherent dressings such as corn plasters to the feet
Rx
- Local wound care: - Clean - Debride infected necrotic devitalized tissue - Wet dressing
- Broad spectrum, covering G+ve, -ve & Anareobic
- In case of mild infection, duration of 1-2 weeks.
- In case of sever infection, duration of 2-4 weeks.
- In case of Osteomylitis, duration of 4-6 weeks IV.
- Control sugar, blood pressure, lipids
- Prevention (proper shoes, instructions, … )
Amputation
- Ray amputation, which involves the excision of the toe and part of the metatarsal
- below or above knee amputation
- hip disarticulation
- transmetatarsal amputation
//////
Peripheral Daflon … treat the cause
Examination
-
WIPER
- Wash hands
- Introduce
- Right side of bed
- Explain Procedure
- Permission for examination
- Position & Exposure
-
Preliminary examination
- General Appearance (man, comfortable, comatose, connected device)
- General examination (Vitals, hand/arm/axilla, hair, face, neck, chest, abd,leg)
-
Focused Examination + (correct technique)
- Specific System Exam - IPPA
- Inspection
- Palpation
- Percussion
- Auscultation
- Lesion/Swelling/Ulcer if present - SSSS TTEDC
- Specific System Exam - IPPA
-
Describe correct physical findings
1) WIPER
Exposure | position | privacy | Ask for vitals
- W ash hands (before and after)
- I ntroduce yourself to the patient and seek his or her consent
- P osition the patient correctly.
- E xpose the patient as needed (e.g. ‘Please take off your shirt for me now, if that is all right’)
- R ight side of the bed
Position & Exposure Peripheral Vascular Disease exam: Normal intro than exposure (bilateral lower limb and cover genitalia position is sitting or semi sitting)
Intro
Greet, Introduce (5th year med), assure privacy (curtain, nurse), explain procedure, position (mention good position - supine semisitting) & exposure (from midchest to midthigh - cover genatelia)
2) General Appearance
- Conscious and alert
- features
- connected devices
elderly male with good build lying comfortable to be - connected to cannula - not connected oxygen. (note general exam findings)
“Now i will do focused examination after general apperance, should i do general examination?“
3) General Examination
dont touch patient until needed
-
Hand: organized explaination from distal to proximal
- Clubbing -
- Capillary refill
- Pulse:
- water hammer pulse
-
Vital signs
-
Face & Neck:
-
Abdomen:
-
Lower Limb: Edema - thumb
Peripheral Vascular Disease: Start with general examination (Inspection and vital along with patients looks) Describe the dressing site and looks (ask the doctor to remove the dressing)
no pallor (check eyes for pallor - look up), hand no tar staining
4) Focused Examination
Diabetic Foot/Ulcer Focused Examination
Comment on Ulcer if found
-
Site (lateral of second toe)
-
Size (2x2 cm)
-
Shape (oval/rounded/irregular)
-
Floor by inspection floor you can see, base you can touch. We must describe the colour of the floor:
i. Red/Pink: This indicates granulation tissue. Granulation tissue indicates healing. - Collagen, fibroblast, capillary, Inflammatory cells and bacteria
ii. Slough/Scab (Yellow Like Cotton): Dead tissue separating; it’s almost going to die. - Sloughed and dried small amount of discharges
iii. eschar - Black: Indicates necrotic tissue. If applicable, we can also say ‘expose tendons or exposed bone’. Layer of dead tissue + DRIED
-
Base (surface) by palpation
- Tenderness
- Arterial Ulcer is painfull
- Venous ulcer less painfull
- Neuropathic usually not
- Temperature
- Base
- Tenderness
-
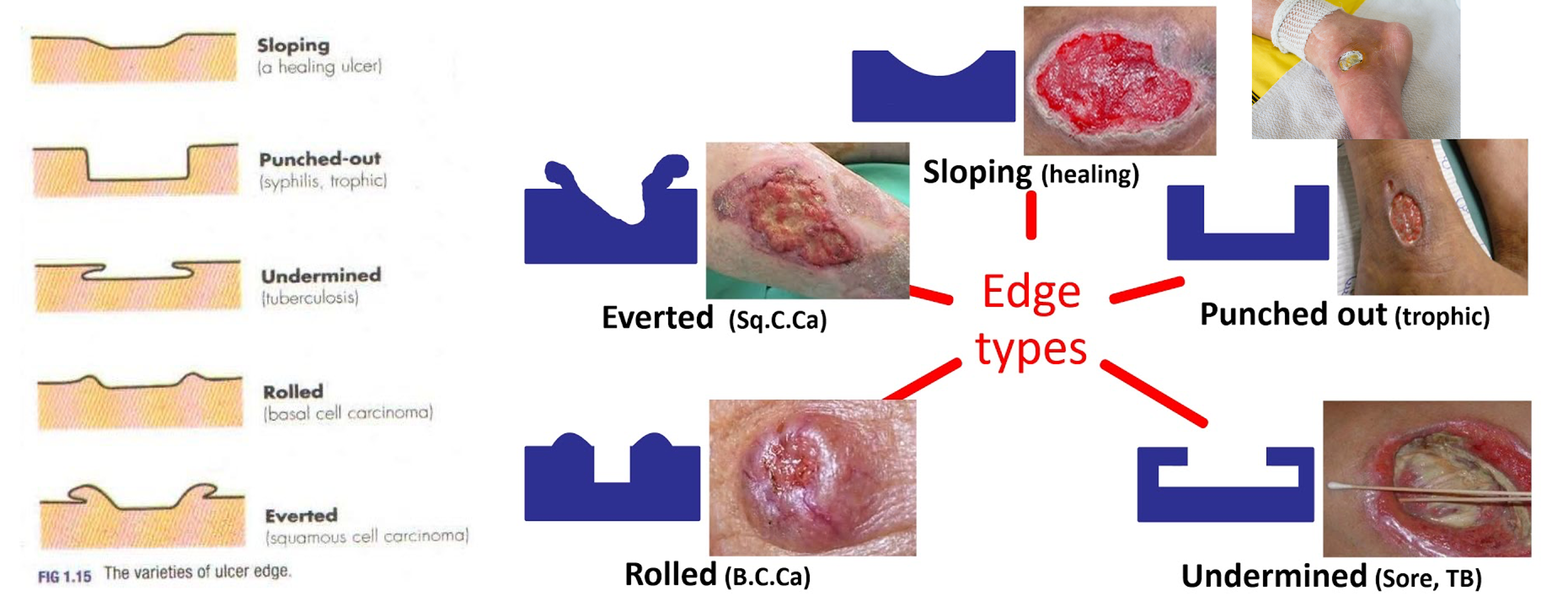
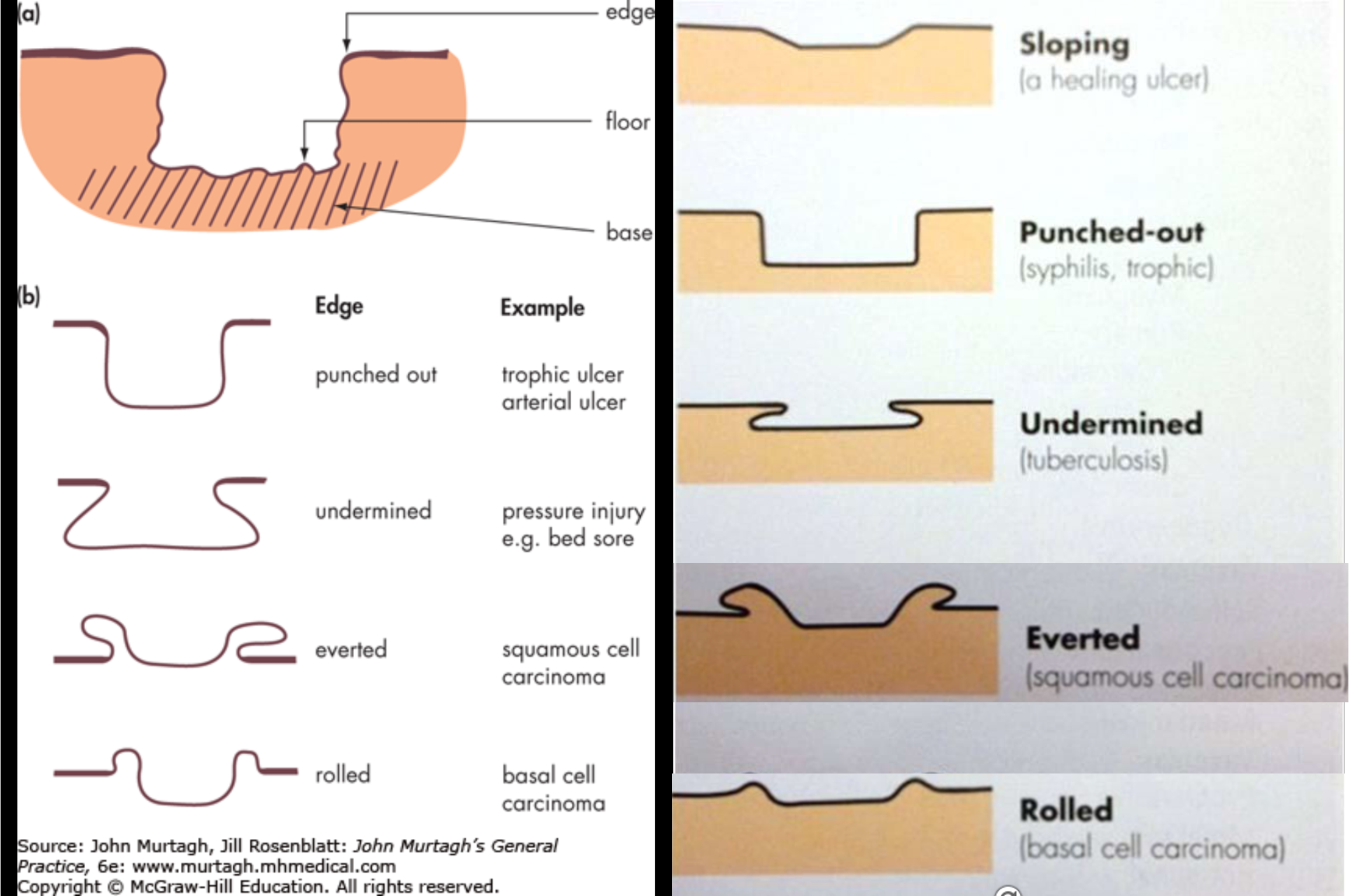
Edge (Punched out or Under Minded?) ALL EDGES IN DIABETIC FOOT ARE SLOPPING EDGE/HEALING
-
Surrounding (edematous, discharges, hair distribution…)
-
Induration (Infection, Trauma)
-
Pigmentation (Venous ulcer mainly)
-
Scaring
-
Edema
- Vascular Assessment
- Skin examination (Atrophy, hair loss, nail changes)
- Capillary refill
- Peripheral pulses (femoral, popliteal, post. tibial, dorsalis pedis)
- Ankle-Brachial index ?
- Neurosensory Assessment
- Light touch, pin prick, temperature, proprioception, vibration
- Reflexes, Babinski, achilleas, patellar
- Lymph nodes
- Local (lymphatic / venous obstruction)
- General (Liver, Cardiac, Renal, low Alb)
-
SSSS BEFS
Then look for any discharge by squeezing above and below ulcer looking for discharge also look for base and edge again also fluctuation test looking for tenderness and temprature
Types of Edge:
- Flat sloping ( healing / venous)
- Punched out (Syphilis / DM (more commonly) / Ischemic)
- Undermined (pressure necrosis, carbuncle, Tuberculous)
- Rolled (BCC)
- Everted (SCC / Ulcerated AdenoCA)
- Sloping edge: pale/pink consistent of new healthy epithelium growing over the base of the ulcer
Also in “Look” you can comment on the surrounding of the ulcer, like: dry skin, scars, hair loss, pigmentation, …
Note
Sloping edge: pale/pink consistent of new healthy epithelium growing over the base of the ulcer
Also in “Look” you can comment on the surrounding of the ulcer, like: dry skin, scars, hair loss, pigmentation, …
results of ABPI normally 1.0-1.2 - less than 0.5 indicate stenosis
Peripheral vascular Focused Examination
Inspection
- Inspect infront bed patient,
- Check symmetry between legs (DVT, PAD)
- to inspect, check between foot fingers,
- raise legs to see any hidden ulcer
General findings of Peripheral vascular disease (typically pale hair loss atrophy erythema skin break down wound nail changes )
theres gauze medial on surface of foot, the gauze is soaked with (pus yellow, clear fluid) dressing is clean? (clean) - ask examiner if you can remove the gauze..
Comment on
- hair loss and muscle wasting
- Venous filling- empty in ischemia (guttering of veins)
-
no ulcer look between toes and under the heal (usually ulcer is punched out in DM look for edge and floor most importantly than others also site and etc) (move everywhere)
-
Amputations, lumps, scars, scratch marks, muscle atrophy, symmetry
- Skin color- shiny skin in ischemia
- Thickening of nail, loss of leg hair
- Discoloration ?patches of gangrene
- Rubor on dependency- red flushed foot returns to normal after some time
- Muscle wasting
- Ulceration- tip of toes
- Pulsatile mass (femoral, popliteal)
- Swelling (DVT)
Features of chronic venous insufficiency (CVI): Oedema, leg induration, pigmentation, eczema, ulceration, skin thickness & redness- lipodermatosclerosis
Palpation
I- check tenderness & temperature on all levels of lower limb from foot tibia thigh right and left (compare both limbs with dorsum of hands) (press on each level look patient eyes, ask patient if he noted any pain)
- Temperature: warm (DVT, infection)
- Tense and tender calf (DVT)
II- Pulse examination (examine one side each) Palpation of Aorta
- Supine position with the knees raised
- Abdominal muscles relaxed
Palpation: Upper limb pulses
- Axillary: in the axilla and medial upper arm.
- Brachial: antecubital fossa immediately medial to the biceps tendon.
- Radial: at wrist anterior to the radius.
- Ulnar: on medial side of the wrist.
Lower limb pulses
-
Femoral: At midinguinal point (midway between the anterior superior iliac spine and the top of the pubic symphysis
- Midpoint of the inguinal ligament – halfway between the pubic tubercle and the anterior superior iliac spine (the two attachments of the inguinal ligament). The opening to the inguinal canal is located just above this point.
-
Popliteal: Knee flexed to 45 degrees. Foot flat on the examination table. Bimanual technique. Both thumbs are placed on the tibial tuberosity anteriorly and the fingers are placed into the popliteal fossa between the two heads of the gastrocnemius muscle and compressing it against the posterior aspect of the tibia just below the knee
-
Posterior tibial: 2 cm posterior to the medial malleolus.
-
Dorsalis pedis 1 cm lateral to the extensor hallucis longus tendon or in the cleft between 1st and 2nd metatarsals (use 3 fingers)
Peripheral scaling
- 0= abbsent
- 1= diminished
- 2= normal
- 3= bounding (aneurysm or AI)
III- Capillary Refill
- compress finger (hold finger then compress nail bed - 2-4 seconds)
IV- Edema assess levels from tarsal prominence, medial mal, tibia, thigh, sacrum
Venous
- Pitting edema in venous diseases
- Skin thickening, redness
- Groin LNs – cough impulse
- Abdominal masses
V- Beurgers test
-
Patient Position: Supine (lying flat on their back).
-
Pain Assessment: Ensure the patient is not experiencing any lower limb pain at rest before starting the test.
-
Leg Elevation:
- Passively elevate the patient’s left leg to 10 degrees.
- Hold for 10 seconds and observe the color of the foot, particularly the plantar surface (sole).
- Incrementally elevate the leg by 10 degrees every 10 seconds until reaching a 45-degree angle - normally at 90 degree there is pallor - ischemia at 20 degrees pallor will appear
- Throughout elevation, watch for pallor (paleness) developing in the foot.
-
Dependency:
- Once the leg is at 45 degrees, ask the patient to sit up and dangle their legs over the edge of the examination table.
- Observe the color of the foot as it becomes dependent (hanging down).
- Look for reactive hyperemia (redness) as blood flow returns to the foot.
-
Interpretation:
-
Positive Buerger’s Test:
- Marked pallor develops during elevation.
- Delayed or absent reactive hyperemia (redness) upon dependency.
- These findings indicate significant arterial insufficiency.
-
Negative Buerger’s Test:
- Minimal or no pallor develops during elevation.
- Rapid reactive hyperemia (redness) upon dependency.
- These findings suggest adequate arterial flow.
-
-
Repeat: Perform the same procedure on the right leg.
VI- Specific Venous tests
- Homan’s sign- stretching calf by foor dorsiflexion resulting pain
- Schwartz / Tapping test (pressure transmission to incompetent distal veins)
- Coughing impulse
- Brodie Trendelenburg test
- Patient’s leg elevated to drain venous blood.
- An elastic tourniquet applied at the sapheno-femoral junction
- The patient then stands with tourniquet in place.
- Rapid filling (<30 seconds) of the great saphenous system- perforator valve incompetent.
- No filling - perforators are competent z
- Now release the tourniquet
- Filling of the great saphenous system from above- sapheno-femoral valve is also incompetent.
- Multiple tourinquet - Triple test
Percussion
No percussion
Auscultation
Auscultation Sites for Peripheral Vascular Disease:
-
Femoral Artery:
-
Location: Auscultate at the mid-inguinal point, which is halfway between the anterior superior iliac spine (ASIS) and the pubic symphysis.
-
Significance: This is the most accessible point to assess the femoral artery for bruits, which are turbulent blood flow sounds indicative of potential stenosis or occlusion.
-
-
Iliac Artery:
- Location: Auscultate in the iliac fossa, a region located deep within the lower abdomen. This requires deeper palpation and may be challenging.
- Significance: Bruits heard here can suggest stenosis in the iliac artery, potentially impacting blood flow to the entire lower limb.
-
Hunter’s Canal (Adductor Canal):
-
Location: Auscultate along the medial surface of the thigh, midway between the groin and the knee. This is where the femoral artery travels deep within the Hunter’s canal.
-
Significance: While not routinely auscultated, bruits here can indicate stenosis within the femoral artery as it passes through this confined space.
-
- Over large veins- murmur in arterio-venous fistula ( veins do not collapse on lying down and can feel pulsation and thrill during palpation)
5) Complete examination with
Peripheral Vascularity Inspect then Motor (power and tone) , Sensory(position and vibration sense, pinprick, cotton test), Reflexes (babinski, achilees, patellar)
Hemodynamic Noninvasive Tests
- Resting Ankle-Brachial Index (ABI)
- Exercise ABI
- Segmental pressure measurement
6) Summarize Findings, Thank patient
…
Other
Describe the following

-
ulcer - if not say discontinuity of skin breakdown representing ulcers involving the second dorsum middle toe, 1x1 cm, circular, granulated healing tissue, edge punched out… shiny skin surrounding edema, erythema
-
Skin disconutiy on left foot between fourth and fifth toe longitudinal 5x2 cm looks like ulcer, floor with dead tissue, undermined edges proximal, punched distal, surrounding looks edematous, hair loss.
-
Ulcer on medial left big toe, 4x4, irregular shape, floor with dead tissue and granulation tissue, with sloping and punched edge, with scar, nair changes, edematous, hair loss.
Callus

Charcot Foot
Charcot neuro‐osteoarthropathy (CNO), a progressive condition of the musculoskeletal system. Characterized by joint dislocations, pathologic fractures and debilitating deformities. It results in a progressive destruction of bone and soft tissues at weight‐bearing joints. It is one of the most serious complications of diabetes.
Treated by immobilization and a reduction of stress to the affected limb
Classic Charcot’s mid-foot ulcer following collapse of the foot arches.

Types of Ulcer
| Feature | Venous | Arterial | Neuropathic Diabetic | Pressure |
|---|---|---|---|---|
| Underlying condition | Varicose veins, previous deep-vein thrombosis, obesity, pregnancy, recurrent phlebitis | Diabetes, hypertension, smoking, previous vascular disease | Diabetes, trauma, prolonged pressure | Limited mobility |
| Ulcer location | Area between the lower calf and the medial malleolus | Pressure points, toes and feet, lateral malleolus and tibial area | Plantar aspect of foot, tip of the toe, lateral to fifth metatarsal | Bony prominences, heel |
| Ulcer characteristic | Shallow and flat margins, moderate-to-heavy exudate, slough at base with granulation tissue | Punched out and deep, irregular shape, unhealthy wound bed, presence of necrotic tissue, minimal exudate unless infected | Deep, surrounded by callus, insensate | Deep, often mace |
| Condition of Leg/Foot | Hemosiderin staining, thickening and fibrosis, skin, limb edema, normal capillary refill | Thin shiny skin, reduced hair growth, cool skin, pallor on leg elevation, absent or weak pulses, delayed capillary refill, gangrene | Dry, cracked, insensate, calluses | Atrophic skin, loss of muscle mass |
| Treatment | Compression therapy, leg elevation, surgical management | Revascularization, Anti-Platelet medications, Management of risk factors | off-loading of pressure, topical growth factors | Off-loading of pressure; Reduction of excessive moisture, shear, and friction; adequate nutrition |
 |
Inspection - Floor
- Red; clean granulation; fibronogen; loop of capilarry
- Black
Palpation - Base ()
Edge
- Sloping - healing ulcer
- Undermined - Bedsores (sacral, trochantric, scalp) - decubitus ulcer, pressure
- Punched-out
- Everted - SCC
- Rolled - BCC
Dry vs wet gang
| Feature | Dry gangrene | Wet gangrene |
|---|---|---|
| Appearance | Dry, shriveled, mummified | Edematous, putrified and discoloured |
| Cause | Occurs due to slow and gradual loss of blood supply | Occurs due to sudden loss of blood supply |
| Infection | Infection not present | Infection present (offensive odor) |
| Symptoms | Cold temp., dull aching pain Skin changes colour to dark brown → dark purplish → completely dark | Offensive odor Swollen, red and warm |
| Demarcation | Clear line of demarcation is present | Vague/ No line of demarcation |
| Extension | No proximal extension | Proximal extension |
| Amputation | Limited amputation | High amputation |
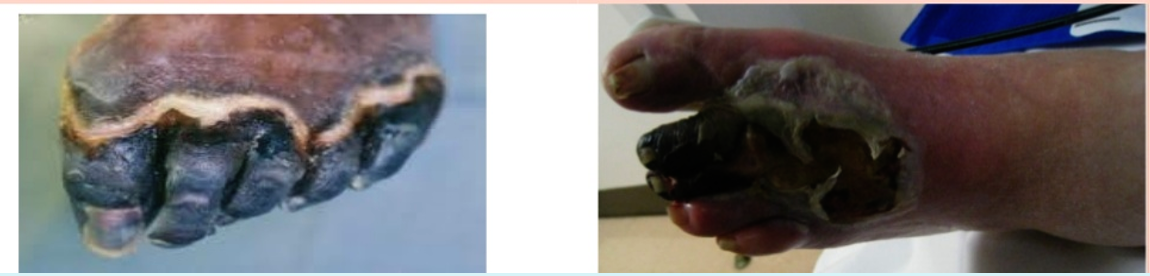 |
diabetic foot
pathogenesis
-
blood supply stenosis
-
neuropathy
-
no immunity
-
most common pathogen staph aureus
Amputation cause septic even afte debribement no improvament
diabetic ulcer arterial venous