Nephrotic Syndrome
… By the end of this lecture, the student should be able to:
- Define nephrotic syndrome
- Explain the pathophysiology of nephrotic syndrome
- Outline the aetiology of nephrotic syndrome
- Elaborate on the primary causes of nephrotic syndrome
- Outline the treatment of nephrotic syndrome
Definition
Nephrotic syndrome is a clinical complex characterized by a number of renal and extrarenal features, most prominent of which are:
- Heavy proteinuria > 3.5g/d
- Edema
- Hypoalbuminemia
- Hyperlipidemia
- HTN +/-
Nephrotic Syndrome vs. Nephritic Syndrome
| Feature | Nephrotic Syndrome | Nephritic Syndrome |
|---|---|---|
| Proteinuria | > 3.5 g/d | < 3.5 g/d |
| Oliguria | Usually present (uremia) | |
| HTN | +/- | Present (with edema) |
| Hematuria | Present |
Pathophysiology
- Proteinuria: Increased permeability due to glomerular pathology leads to protein loss in the urine.
- Low serum albumin
- Edema: Decreases oncotic pressure, causing fluid leakage into the interstitium.
- Hyperlipidemia: Increased synthesis of lipids.
 5th - hypoalbumin; Meuchrcke
5th - hypoalbumin; Meuchrcke

Aetiology
Nephrotic syndrome can be classified as primary or secondary.
Primary: Z
Secondary: Z
- Glomerular diseases: Diabetic Nephropathy, Amyloidosis
- Drugs: Gold, heroin, penicillamine, NSAIDs (mal nephropathy) , captopril
- Infectious diseases: PSGN, HBV, HCV, HIV, Malaria, Schistosomiasis, Filaria
- Hereditary: Alport’s syndrome, Nail–patella Syndrome
- Others: Malignancy, Pre-eclampsia, SLE

Investigations
General:
- Urine dipstick analysis
- Midstream urine for microscopy, culture and sensitivities
- Quantify proteinuria (early morning urinary protein:creatinine ratio or albumin:creatinine ratio)
- FBC and coagulation screen
- Renal function and electrolytes
- LFTs
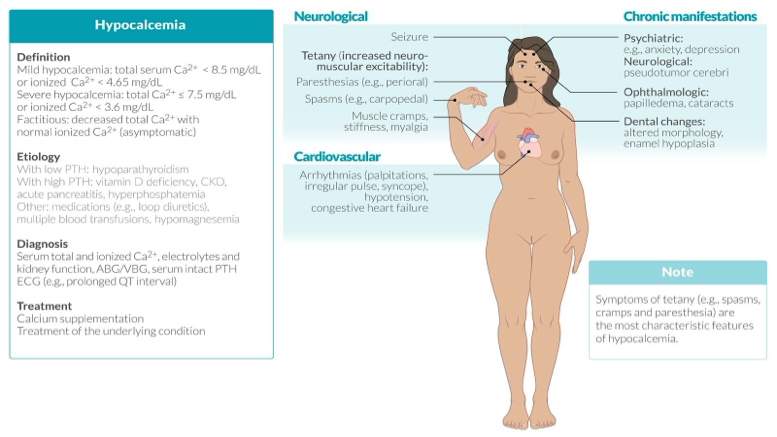
- Bone profile (calcium, phosphate, alkaline phosphatase)
- Fasting glucose
- Lipid profile
Other systemic diseases and causes of nephrotic syndrome:
- ESR and CRP,
- Immunoglobulins,
- serum and urine electrophoresis,
- Autoimmune screen,
- Hepatitis B and hepatitis C; HIV,
- Thyroid function tests.
Imaging:
- Chest X-ray
- Abdominal ultrasound
- Renal ultrasound scan
- Doppler ultrasound of leg veins - Renal vein thrombosis
- Renal vein Doppler scan, CT and MRI scanning of the abdomen if renal vein thrombosis is suspected.
- CT, pulmonary angiography for pulmonary embolism.
Renal biopsy under ultrasound
Complications of Nephrotic Syndrome
-
Increased risk of thromboembolism: Related to loss of antithrombin III, protein C, protein S and plasminogen in the urine.
-
Deep vein thrombosis, pulmonary embolism, resulting in a sudden deterioration in renal function.
-
Renal vein thrombosis presenting with sudden-onset unilateral flank pain, acute deterioration in renal function and new haematuria. ↑ LDH.
Treated with heparin and then warfarin. If no history of thrombosis in a nephrotic patient, “usually” no prophylactic warfarin given.
- Hyperlipidaemia: ↑ Plasma levels of cholesterol, LDL, triglycerides, and lipoproteins (mainly LPA) to compensate for the loss of albumin → lipiduria (fatty casts) increasing risk of ACS, stroke.
- Chronic kidney disease
- Hypocalcemia: (Vitamin D deficiency and binding protein lost in urine)
- Protein malnutrition
- Anemia
- Infections/Sepsis: Streptococcus pneumoniae due to
- urinary loss of immunoglobulins.
- Treat infections aggressively.
- Common cause of death in nephrotic syndrome.
Diagnosis of Nephrotic Syndrome
-
Confirmation of nephrotic-range proteinuria:
- Qualitative assessment by urine dipstick (commonly used for screening)
- Quantitative assessment of urine protein excretion:
- 24-hour urine protein (test of choice): > 3.5 g/24 hours
- Spot urine protein/creatinine ratio: > 3.5 g/g
-
Urine sediment microscopy:
- Nephrotic sediment:
- Lipiduria, fatty casts with Maltese cross appearance under polarized light,
- Renal tubular epithelial cell casts
- Nephrotic sediment:
-
Additional laboratory studies:
- ↓ total protein; ↓ albumin (< 3 g/dL)
- ↓ ATIII
- Hyperlipidemia
-
Renal biopsy:
- Indication: to confirm the diagnosis when the etiology of NS is unclear
General Management of Nephrotic Syndrome
- Salt & water restriction
- Diuretics: Furosemide (Lasix), + amiloride
- Normal protein diet: Protein < 80g/d. Don’t take high protein diet as it will worsen proteinuria & renal damage.
- ACE inhibitors (1st choice) or ARBs HTN if present
- High cholesterol: Diet & drugs (statins)
- Thrombosis: Anticoagulants (↑ risk in Membranous GN & ↓ albumin). Treatment: warfarin or LMWH.
- Pneumovax vaccine (against pneumococci) every 5 years & annual flu vaccine
Electrocardiogram (ECG) changes in hyperkalemia:
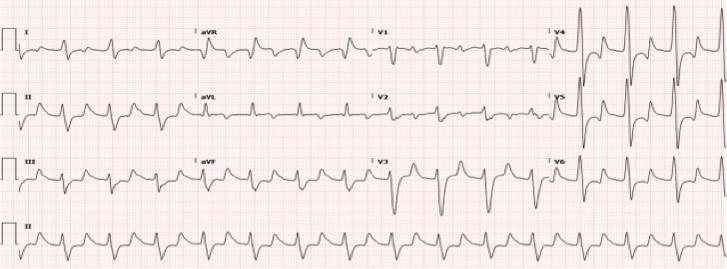
- Peaked or ‘tall-tented’ T waves
- Loss of P waves
- Broad QRS complexes
- Sinusoidal wave pattern
Causes of nephrotic syndrome at a glance
- Minimal Change Disease (can be primary or secondary to Hodgkin’s, NSAIDs)
- Membranous nephropathy (primary or secondary to SLE, Hep B, malignancies, drugs like gold)
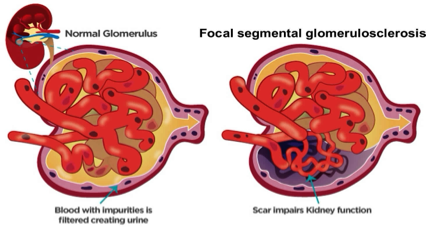
- FSGS (HIV)
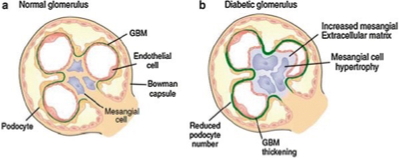
- Diabetic Nephropathy
- Deposition Disorders (amyloidosis, Multiple myeloma)
Case scenario CC
An 18-year-old woman with a history of presumed minimal change disease as a child presents to the renal outpatient department with recurrent nephrotic syndrome. She is commenced on a loop diuretic and high-dose corticosteroids, but after 2 months remission has not been achieved.
What will you do? CC Atypical for minimal change disease to fail to remit by this point, and because the diagnosis had never before been histologically proven, a renal biopsy is carried out.
What is to be expected? CC Focal segmental glomerulosclerosis
Clinical scenario CC
A 54-year-old woman presents with worsening peripheral oedema. She had been diagnosed with type 2 diabetes 6 months earlier, but remained well until 4 weeks ago, when she suddenly noted frothy urine and mild peripheral oedema. Over the following weeks the oedema had worsened and she noted some abdominal distension. Her only regular medication is gliclazide.
Examination
- Pitting oedema to her lumbar spine, with bilateral small pleural effusions
- JVP not elevated and heart sounds normal.
- Mild erythema over right ankle and lower leg.
Take Away Message
Causes of nephrotic syndrome at a glance
- Minimal Change Disease( can be primary or secondary to Hodgkin’s, NSAIDs)
- Membranous nephropathy(primary or secondary to SLE, Hep B, malignancies, drugs like gold,)
- FSGS ( HIV)
- Diabetic Nephropathy
- Deposition Disorders( amyloidosis, Multiple myeloma)

 zzi.sh/rpa27958
zzi.sh/rpa27958