Herbert pits
 #Y
#Y
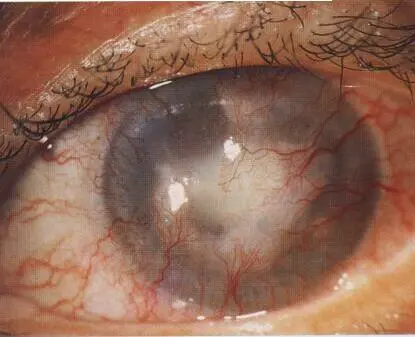
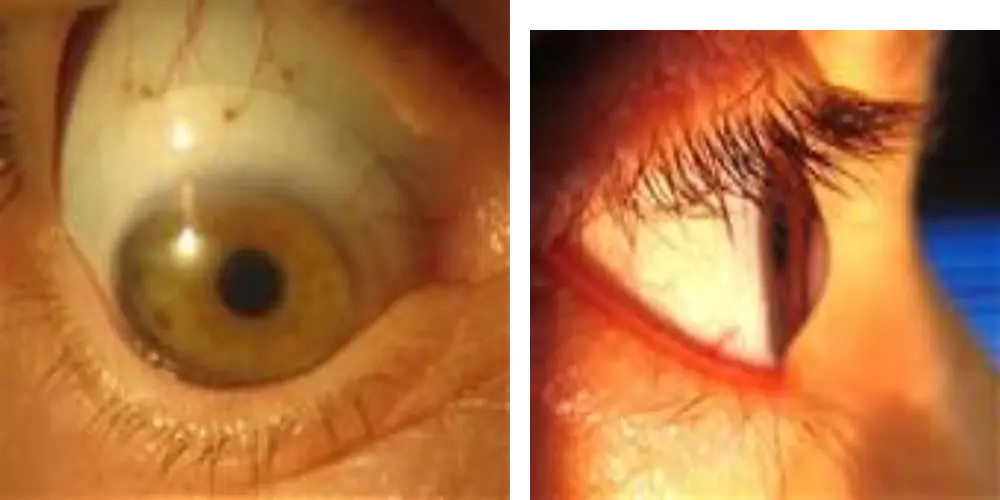
Corneal pannus
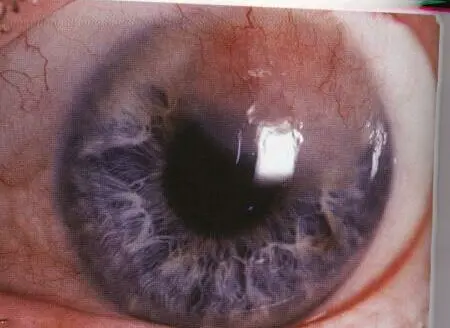
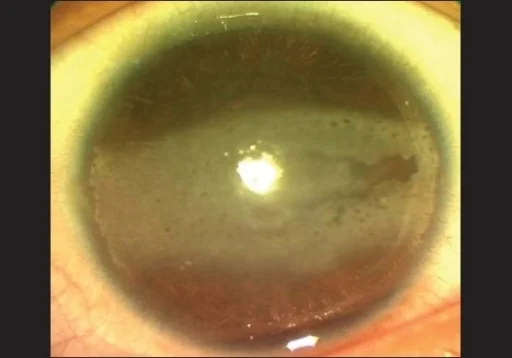
Arcus Senilis
Pathology/Cause: It is caused by lipid (fat) deposits deep in the edge of the cornea. This condition is common in older adults and is generally considered a normal part of aging. It does not typically affect vision or require
If juvenile suspected hyperlipidemia


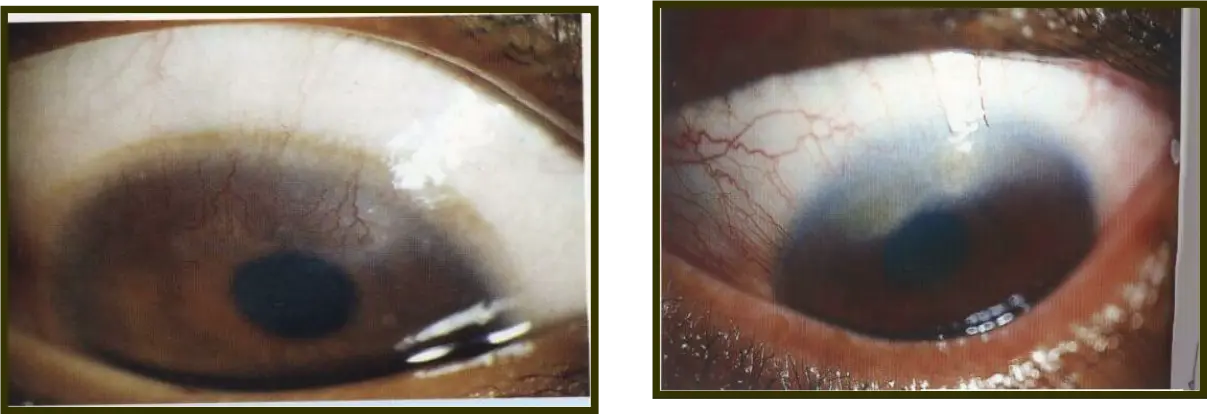
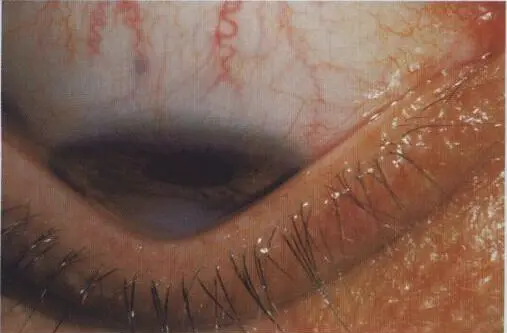
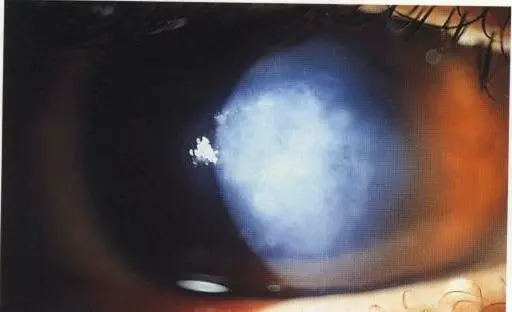
Band shaped keratopathy
Horizontal opacity
Pathology/Cause: Hyaline degeneration + Ca deposition
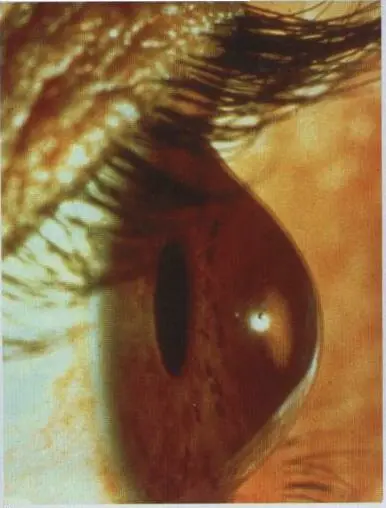


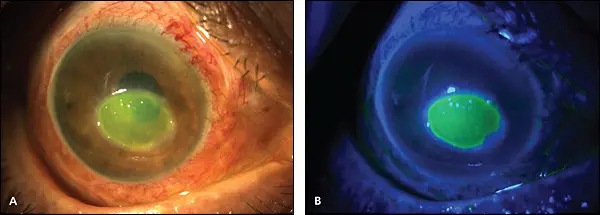
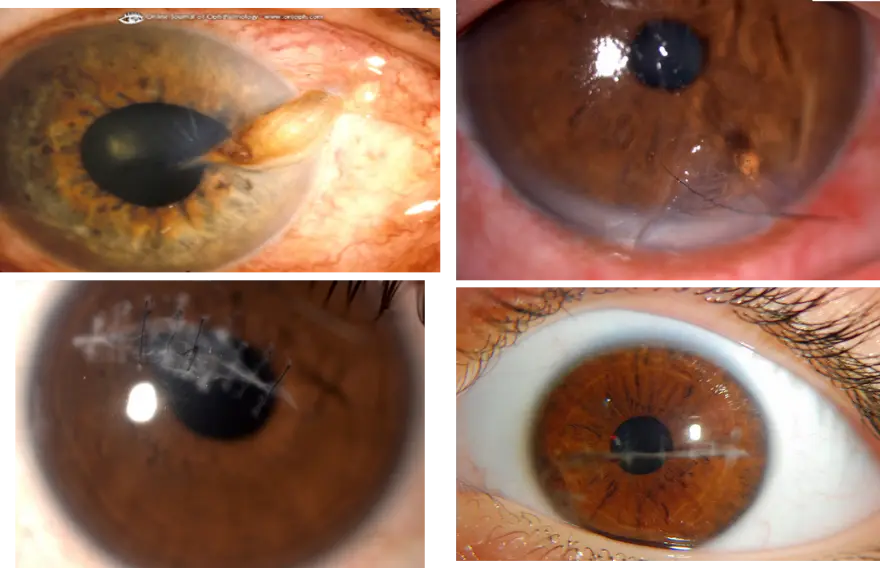
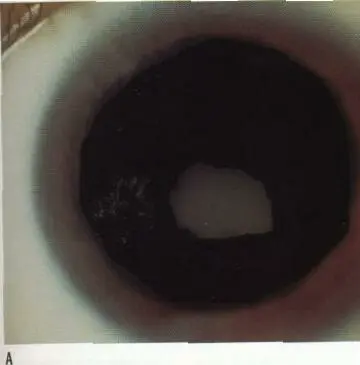
Keratoconus
Cornea/name condition:
- Keratoconus
Pathology: progressive stromal thinning, leading to conical protrusion of the cornea
Refractive error type: associated with irregular astigmatism + irregular myopia
Characteristic sign: Munson’s sign
Treatment:
- if early: cross-linking (to stop progression) + correction of astigmatism / glasses
- if late/advanced stage: keratoplasty (KP) or corneal transplant
Hard contact lens
Infective keratitis
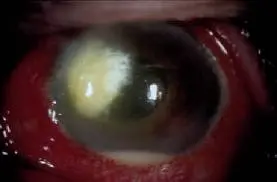
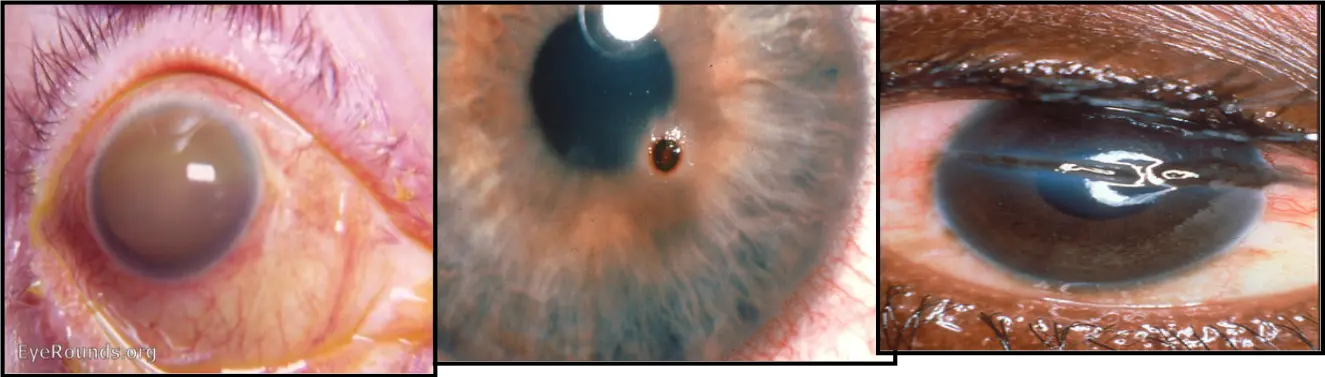
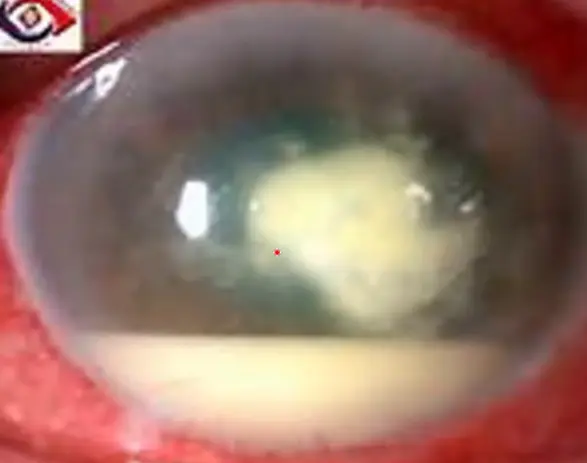 1- Hypopyon ulcer:
1- Hypopyon ulcer:
Causative organism:
Pneumococci
What is hypopyon:
Pus in the anterior chamber
Is it sterile?
Yes
When does it become infected?
After perforation

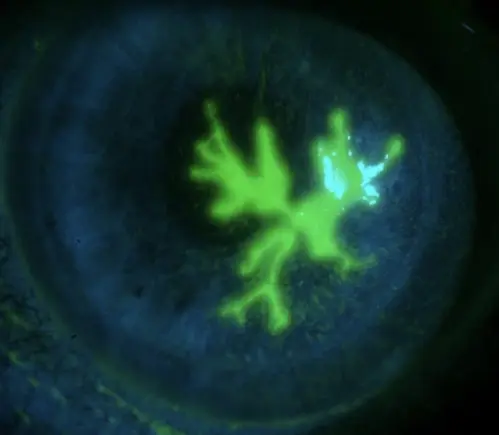 2- Herpetic ulcer:
2- Herpetic ulcer:
Signs:
Dendritic Herpes
Cause:
Herpes simplex or zoster virus
Complication:
Loss of corneal sensation is common presentation
if you use corticosteroid it will lead to?
Geographic ( Amoeboid ) ulcer

3- Fungal:
Landmark:
Microabscesses (satellite appearance)
Cause:
Older patients, immunocompromised, ocular trauma from organic materials such as plant matter
Treatment:
Usual treatment, Topical/systemic antifungals, Surgical Treatment (PKP)
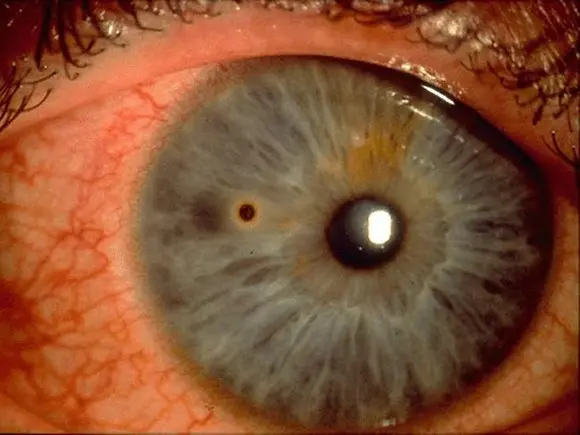
4- Acanthamoeba keratitis:
Sign:
Ring-shaped ulcer/keratitis
Treatment: Corticosteroid
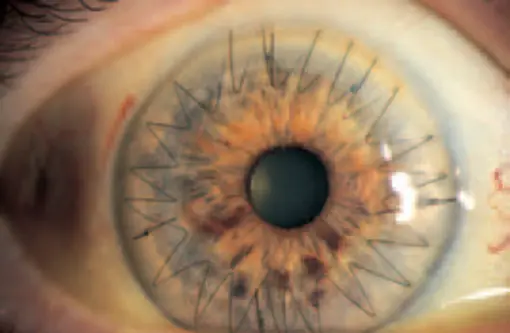

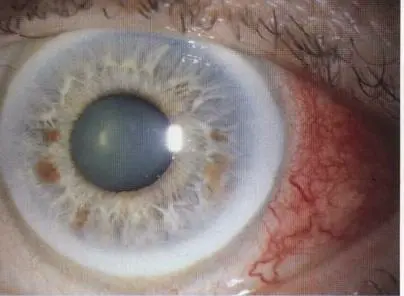
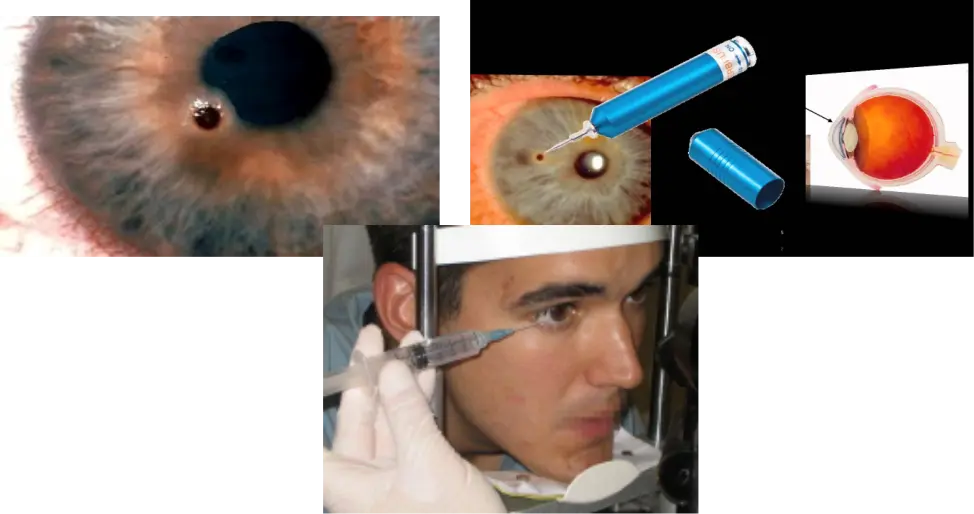
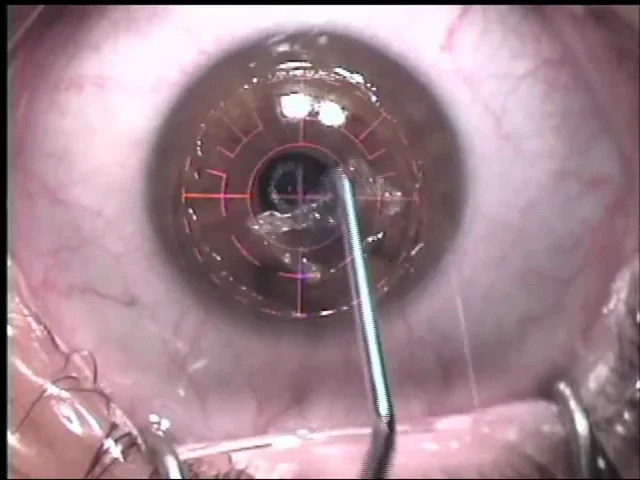
Corneal transplant
Corneal transplant: Sutures placed all around the cornea (7- and 8-point appearance or straight interrupted)
Donor tissue coming from what: A deceased person (cadaveric)
Indications: Any corneal condition affecting vision or the visual axis;
- e.g., Advanced keratoconus,
- Keratomalacia
- Fuchs’ endothelial dystrophy,
- corneal scarring,
- bullous keratopathy.

Keratoplasty
Corneal Foreign Body
Removal by: Slit-lamp-guided removal with a sterile needle or spud under topical anesthesia.
Never remove foreign body from eye in emergency room, only in operating room in sterile conditions
Chemical reactions
Siderosis: FE rust Chaliosis: CU
Alkaline is worst - results in rapid penetration of ocular tissue Acidic = coagulation of protein
Irrigate eye with normal saline at least 15 minutes In chemical burn then refer do not cover and refer to ophth
Corneal Trauma
Treatment:
- Cover and refer to an ophthalmologist
- Suture and repair according to the duration of iris prolapse
Investigations:
- X-ray
- CT
- Ultrasound
- Never use MRI
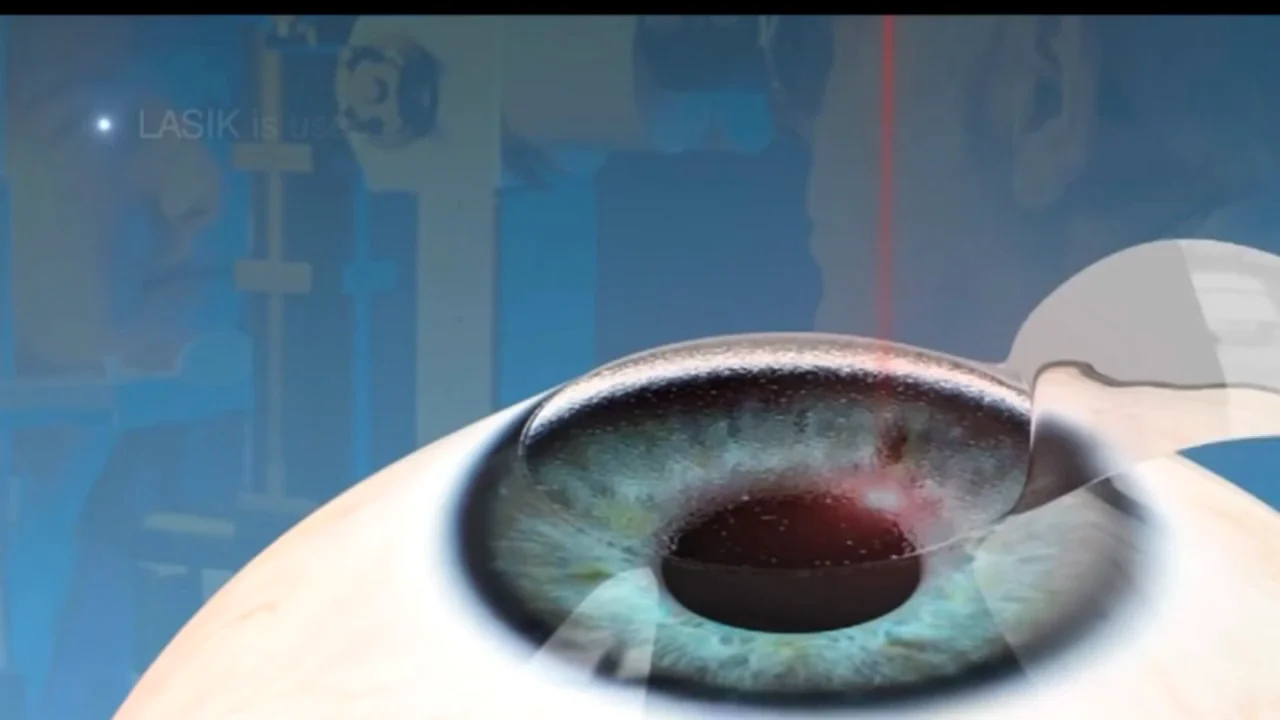
PRK: (corneal epithelium removal; by alcohol specific concentration, special spatula, after removal of epithelium wash the stroma by saline and then apply laser; Exciemer laser = ablation i.e. reshaping of corneal stroma
Keratectasia Y

Corneal opacity Y
Corneal nebula Y

Corneal macula Y
Corneal vascularization Y