Risk factors
include immobility, inherited hypercoagulability disorders, pregnancy, postpartum period, and recent surgery.
clinical presentation
can range from asymptomatic to obstructive shock, depending on the extent of pulmonary artery obstruction.
Because symptoms are often nonspecific (e.g.,chest pain , coughing, shortness of breath, and tachycardia), PE should be considered in all patients with acute dyspnea.
diagnosis
is usually based on history and clinical suspicion, then confirmed with CT pulmonary angiography (CTPA) (the preferred test )
Characteristic findings:
in Chest X-ray - PA View:
A peripheral opacity (Hampton hump; obscures the adjacent margin of the right hemidiaphragm. The appearance is often wedge-shaped.
-
Hampton hump: a wedge-shaped opacity in the peripheral lung with its base at the thoracic wall; caused by pulmonary infarction and not specific for PE.
-
Westermark sign: an area of lung parenchyma lucency caused by oligemia secondary to occlusion of blood flow.
-
Fleischner sign: a prominent pulmonary artery caused by vessel distention due to a large pulmonary embolus (common in massive PE)
-
Nonspecific findings: Atelectasis, Pleural effusions, Cardiomegaly
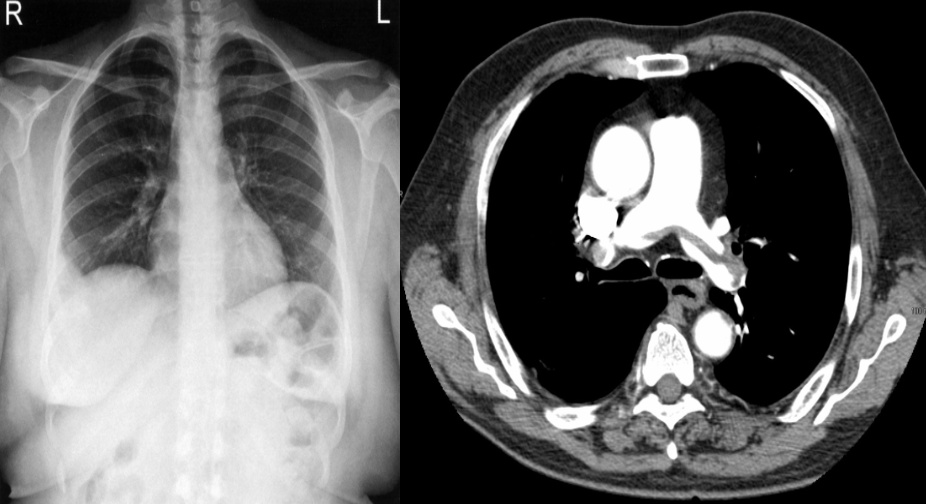
CT chest (with contrast; axial plane)
A large embolism is seen, with extension across the bifurcation of the pulmonary trunk into the right and left pulmonary arteries. Straddling of the pulmonary trunk bifurcation by pulmonary embolism is sometimes referred to as saddle embolism.