Vesiculobullous Skin Diseases CS-OSPE






Pemphigus Vulgaris (PV)
Age from 50-60 years, may be associated with other autoimmune diseases, particularly myasthenia gravis and thymoma, new bulla usually are flaccid or become flaccid quickly. Affected skin often is painful but rarely pruritic.
A patient, often an older individual (e.g., 75 Y/O), presents with generalized skin eruption and blisters, which were preceded by oral ulceration (e.g., 3 months prior). The patient complains that the blisters easily rupture and stay intact only for a while. There is typically a burning sensation, and itching is denied.
What is the diagnosis? Pemphigus Vulgaris (PV)
What is the differential diagnosis?
- Bullous Pemphigoid
- Dermatitis Herpetiformis
- Chronic bullous disease of: (if case was child : of childhood - if was adult : of adulthood)
Describe the primary lesion/feature or type of bulla? Blistering of skin and mucosal membrane with flaccid bullae, which usually arises on normal-appearing skin. It is an intraepidermal bulla.
From the scenario/case history and presentation, what makes you choose this diagnosis or mention key features/clues supporting it?
- A. Oral mucosa ulceration (often the initial presentation, preceding skin lesions)
- B. Not itchy
- C. Painful (e.g., burning sensation)
- D. ER case
- Flaccid blisters (thin-walled, easily ruptured)
- Extensive erosions over the body (due to ruptured blisters)
- Lack of itching
- Involvement in flexural areas (though often generalized)
What are the characteristic clinical signs of the disease?
- Nikolsky sign: Dislodgement of intact superficial epidermis by lateral finger pressure on seemingly uninvolved skin adjacent to a blister or erosion. Shearing stresses on normal skin can cause new erosions to form.
- Asboe-Hansen sign: Pressure on an intact bulla causes lateral extension of the blister.
What is the pathophysiology/pathogenesis?
- Pemphigus Vulgaris is an autoimmune disease where IgG autoantibodies (Ab) are produced.
- Blisters in PV are associated with the binding of IgG autoantibodies to keratinocyte cell surface molecules.
- These antibodies target desmoglein 1 and desmoglein 3 (Ag), which are adhesion molecules found in desmosomes, structures responsible for cell-cell adhesion between keratinocytes within the epidermis.
- This antigen-antibody reaction leads to acantholysis (a loss of cell-cell adhesion between keratinocytes).
- Acantholysis results in the formation of intraepidermal bullae.
Tests that may be done / Investigations to confirm the diagnosis and what do you expect to find?
- Nikolsky sign is positive. Dislodging of epidermis by lateral finger pressure in the vicinity of lesions, which leads to an erosion.
Shearing stresses on normal skin can cause new erosions to form

- Asboe-Hansen sign is positive.
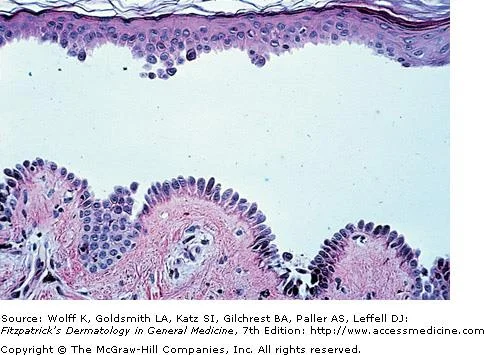
- Histopathology (Skin Biopsy): Intraepidermal bulla, with acantholysis. The basal cells appear as tombstones (basal keratinocytes often remain attached to the basement membrane).
- Direct Immunofluorescence (DIF) on perilesional skin: Intercellular deposition of IgG and/or C3 in a characteristic “net-like” or “fishnet” pattern within the epidermis.
- Indirect Immunofluorescence (IDIF) (Serum – using monkey esophagus): Circulating IgG autoantibodies against the cell surface of squamous epithelial cells (demonstrating anti-desmoglein antibodies).
- ELISA: Detection of anti-desmoglein 1 and 3 antibodies in serum can also be used for diagnosis and monitoring disease activity.
What is the aim of treatment?
- Decrease blister formation
- Promote healing of blisters and erosions
Drugs reported most significantly in association with this disease?
- Penicillamine
- Captopril
How to manage this patient / What is the treatment of choice?
- Full history
- Examination
- Lab tests
- Education
- ==Admit the patient to burn care unit and stop the drug==
- Systemic Corticosteroids: High-dose Prednisone (e.g., 1-1.5 mg/kg/day) is the cornerstone of initial treatment to control severe disease.
- Immunosuppressants (Steroid-sparing agents): Medications like Azathioprine (Imuran) (e.g., 1 mg/kg/day), Mycophenolate Mofetil, Cyclophosphamide, or Rituximab (a biologic agent) are often used in combination with corticosteroids to reduce the steroid dose, prevent side effects, and maintain remission.





Bullous Pemphigoid (BP)
Onset usually after 60 years of age. Usually itchy, blistering, not affect the mucosa only skin, flexures are often affected. An 80-year-old man presents with a two-week history of tense, fluid-filled blisters on his shins. He denies any oral ulcers or mucosal involvement. The blisters developed spontaneously, with no preceding trauma or known triggers. He reports mild itching but no significant pain. His past medical history is unremarkable, and he has never experienced similar symptoms before.
What is the diagnosis? Bullous Pemphigoid (BP)
What is the differential diagnosis?
- Pemphigus Vulgaris (PV)
- Dermatitis Herpetiformis
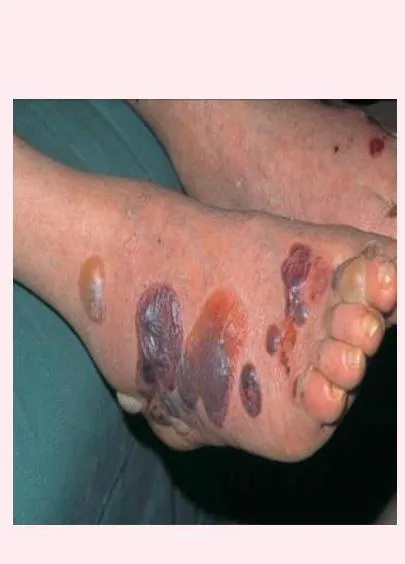
Describe the primary lesion? / What is the clinical presentation? Bullae may be centered on erythematous and urticated base. Pruritus is a primary symptom. Lesions are typically multiple, blustering, tense bullae, sometimes observed on areas like the RT dorsum aspect.
List clinical clues supporting this diagnosis:
- A: No oral lesions
- B: Older patient
- C: Tense bullae on the shin
- D: No history of previous episodes; patient appears well
- Usually itchy
- Not affect the mucosa only skin
- Flexures are often affected
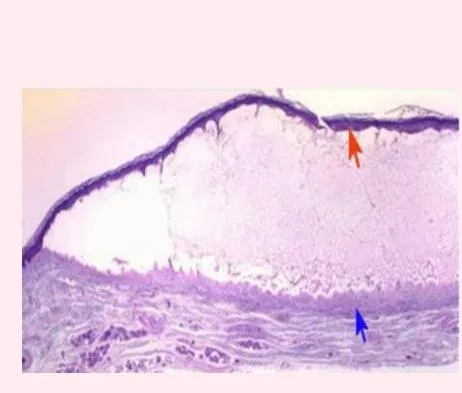
What is the pathophysiology? / What is the pathology? Autoantibodies (Igs & complement factors) form to antigens (BP Ag type 1 and BP Ag type 2 / PB1,2 antigen, specifically IgG) directly beneath the basal layer of the epidermis, at the dermo-epidermal junction (hemidesmosomes and in the lamina lucida). There is linear deposition of these Igs & complement factors. Complement is then activated, starting an inflammatory cascade which results on separation at lamina lucida, causing loss of adhesion and leading to subepidermal, non-acantholytic bullae.
write two differential and their histopathology findings
- A- PV : suprabasal epidermal cells separate from the basal cells to form clefts and blisters (tombstone appearance in the basal cells
- B - TEN : supepidermal bullea with widespread epidermal necrosis, apoptosis of keratinocytes
Tests that may be done / Diagnostic findings?
- Nikolsky sign is negative.
- Asboe-Hansen sign is negative.
- Histopathology: Separation at lamina lucida. - Subepidermal bulla. The epidermis forms: the roof of the blister. The dermis forms: the base of the blister.
- Direct Immunofluorescence (DIF): A specific test on the left has been requested. It shows a characteristic linear deposition of IgG and/or C3 at the dermo-epidermal junction (basement membrane zone). If it is positive, this confirms the diagnosis of Bullous Pemphigoid.
How to manage this patient / Treatment? The disease is self-limiting within 6 months-1 year. Management includes:
- Full history
- Examination
- Lab tests
- Education
- Oral low-dose systemic steroids (e.g., 30-40 mg/day of prednisone) are commonly used.
- High-potency topical corticosteroids can be effective for localized disease or as an initial treatment.
- Other immunosuppressants (e.g., Azathioprine (Imuran), Methotrexate, Mycophenolate Mofetil) may be used for severe or refractory cases, or to allow for steroid tapering.
Complications ?
- A- Bacterial infection
- B- cosmetic problem