Type I
-
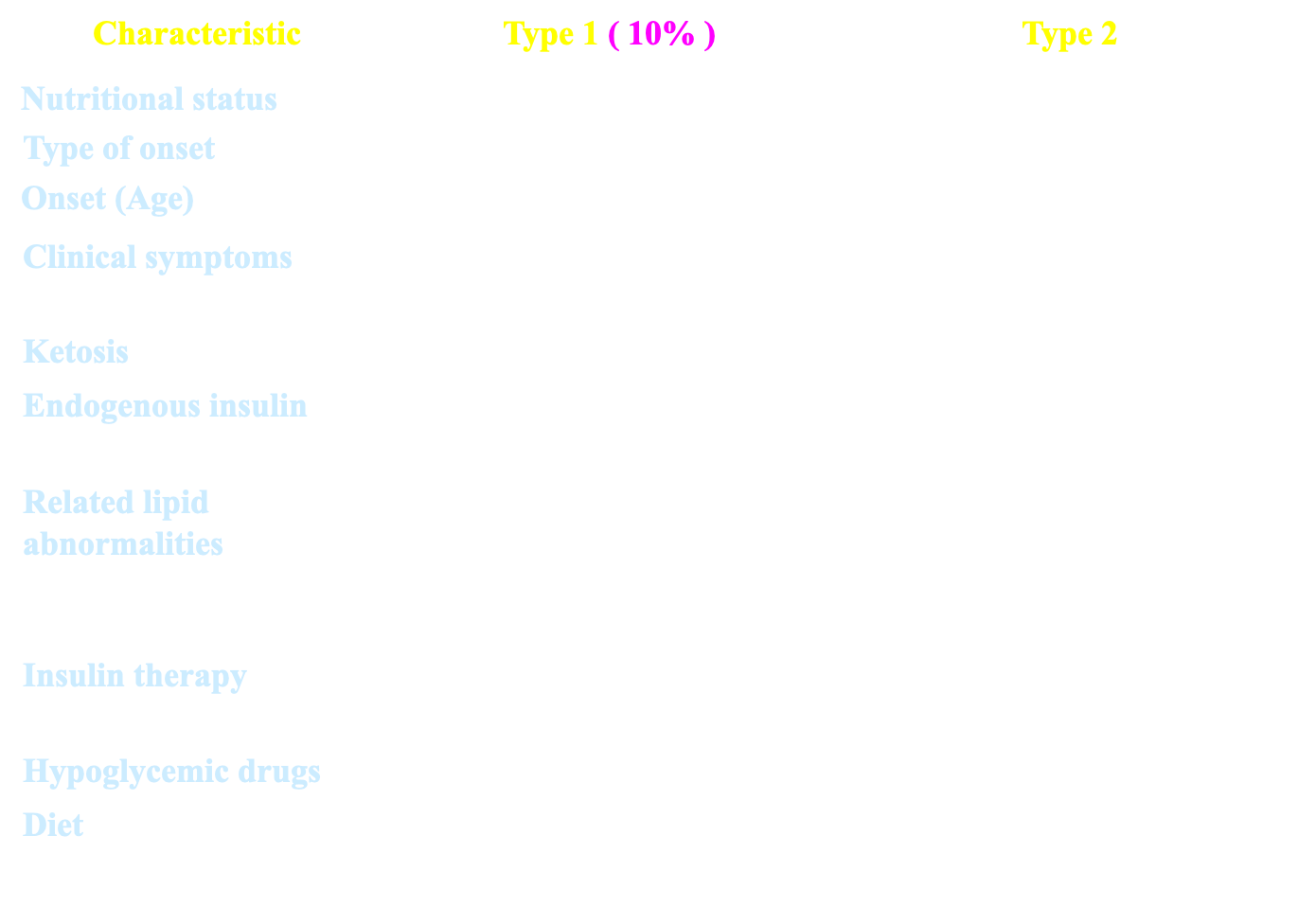
Called insulin-dependent diabetes
-
an autoimmune condition. Occur in childhood -Rapid onset, Complete insulin deficiency
-
Absolute insulin requirement.
-
Autoimmunity is the major factor in the pathophysiology of type 1 DM.
-
Approximately 85% of type 1 DM patients have circulating islet cell antibodies.
-
The most commonly found islet cell antibodies are those directed against glutamic acid decarboxylase (GAD) which is an enzyme found within pancreatic beta cells
-
Once about 80-90% of the beta cells are destroyed, hyperglycaemia develops and diabetes manifests.
Type 2 diabetes mellitus
- Ranges from predominantly insulin resistance with relative insulin deficiency to a predominantly secretory defect with insulin resistance
- Insulin required in 20-30% of patients
- Heterogeneous polygenic disease
- Progression gradual
- It develops when the body cells are unable to efficiently use the insulin (insulin resistance) .
- The pancreas initially tries to make more insulin (hyperinsulinemia) in order to overcome insulin resistance, but eventually there is beta cell exhaustion and failure and then the beta cells don’t make enough insulin leading to relative or absolute insulin deficiency (especially if Type 2 DM has been present for a long time)
- Called non-insulin dependent
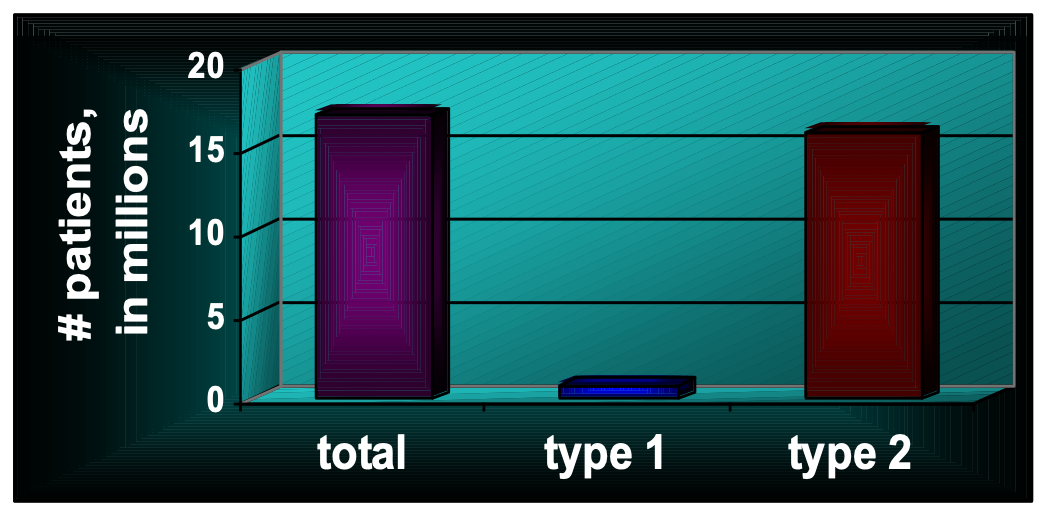
- Most common
- Used to be called adult-onset diabetes, but with the epidemic of obese and overweight kids, more teenagers are now developing type 2 diabetes
- often a milder form of diabetes than type 1
Risk Factors
- Weight.
- Inactivity.
- Family history.
- Age
- Gestational diabetes. 60% may become diabetic after second confirmed hypoglycemia due pregnancy Diabetes that’s triggered by pregnancy Often diagnosed in middle or late pregnancy Having gestational diabetes does, however, put mothers at risk for developing type 2 diabetes later in life Can occur anywhere from a few weeks after delivery to months or years later
- Polycystic ovary syndrome.
Insulin Resistance and the Metabolic Syndrome (Syndrome X) .
- *Hyperglycemia
- *Intra-abdominal obesity,
- *high levels of plasma triglycerides and low levels of high density lipoproteins (HDLs),
- *hypertension
Manifestations of diabetes mellitus:
- Acute manifestations
- Asymptomatic
- Polyurea.
- Polydepsia.
- Weigh Loss despite of food intake (polyphagia).
- Formation of ketone bodies.
- Fatigue and loss of concentration.
- Recurrent infection e.g. vaginitis or pruritis valvae in female (glucose is an excellent medium for macro-organism).
- Increased lipolysis leads to formation of ketone bodies in the body due to lack of insulin (more common in type I).
- Blurred vision due to osmotically induced changes in the eye lens.
Laboratory investigations:
Urine analysis for glucosuria & ketonuria.
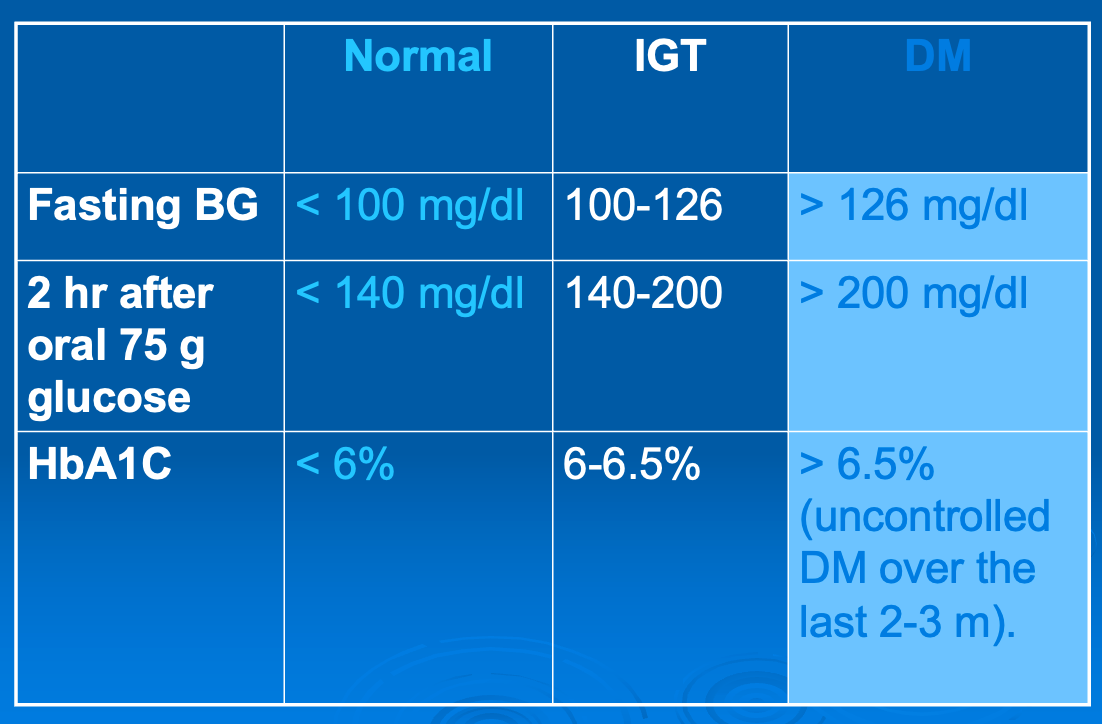
2. Blood glucose: fasting and 2-hr after oral 75 g glucose. Fasting BG > 126 mg/dl OR 2 hr postprandial BG > 200 mg/dl.
3. Glycated hemoglobin (HbA1C): Indicates average blood sugar level for the past 2-3 months. > 8% (elevated levels mean uncontrolled DM for long period).
4. Test for lipid profile especially triglycerides and cholesterol.
Goals of therapy:
- Try to maintain patient as close to euglycemia as possible.
- Try to keep the patient free of symptoms associated with hyperglycemia.
- Try to eliminate or minimize all cardiovascular risk factors and other complications of diabetes.
- Normal growth and development should be maintained in Children (Type I) i.e no restrict diet control.
Lines of treatment:
- Patient education about the disease and its complications.
- Exercise: promotes peripheral utilization of glucose and ↓ insulin requirements, improves utilization of fat. It also prevents CVS complications.
- Diet control.
- Diet + insulin (type 1).
- Diet + oral antidiabetic drugs ± insulin (type 2).
Intensive patient education about: Y
- Manifestations of disease and its complications (including hyper and hypoglycemic manifestations).
- How to test urine for glucose.
- Disease treatment (non-drug therapy, type of drug therapy, where and how to inject insulin preparations).
- Personal hygiene with regard of skin, feet and teeth
- Simple pathophysiology
- Treatment modalities
- Recognition, treatment and prevention of acute complications
- When to call the doctor
- Foot care, eye care, general hygiene, risk factor management
Diet regime
-
Children and underweight patients need 40 calories /kg/day.
-
Middle age (non-obese) need 30 calories /kg/day.
-
Overweight (obese) adult needs 20 calories /kg/clay.
Distribution of diet is as follows:
-
20% of calories from proteins
-
(1.5 gm/kg/day)
-
(Igm=4calories).
-
40% of calories from carbohydrates
-
(2.5 gm/kg/day)
-
(Igm=4 calories).
-
40% of calories from fat
-
(1 gm/kg/day)
-
(Igm = 9 calories).
Indications of insulin:
- IDDM.
- NIDDM in some conditions:
- In combination with diet and oral hypoglycemics after their failure
- Stress conditions e.g. infections, surgery, and pregnancy.
- Diabetic ketoacidosis: regular insulin is the only type used i.v.
Other uses: 7. Hyperkalemia (insulin + glucose): insulin ↑K+ shift from blood to cells. 8. Anorexia nervosa: to stimulate appetite.