SURGERY
PRINCIPLES OF PERIOPERATIVE CARE
VIII. Acute Pancreatitis:
Serum Amylase can rise over 3-6 hours reach peak 24 hours then cleared in urine (4-8 days), while lipase reabsorbed into the circulation
- Normal: 30-110 U/L
- Pancreatitis suspected: > 200 U/L
Serum lipase peaks at first 24 hours with serum concentration elevated for 8 – 14 days. So Elevated lipase levels are more specific to the pancreas than elevated amylase levels.
- A normal lipase level can range from 0-160 U/L. Pancreatitis suspected: > 200 U/L
- {Testing both discouraged for cost-effectiveness}
Investigations
- The key to diagnosis:
- a high index of suspicion
- measurement of the serum amylase concentration. (*3). Serum lipase is an alternative and more specific.
- Other underlying causes of hyperamylasemia:
- mesenteric vascular ischemia, bowel strangulation,
- perforated duodenal ulcer,
- ruptured aortic aneurysm,
- ruptured ectopic pregnancy,
- acute cholecystitis.
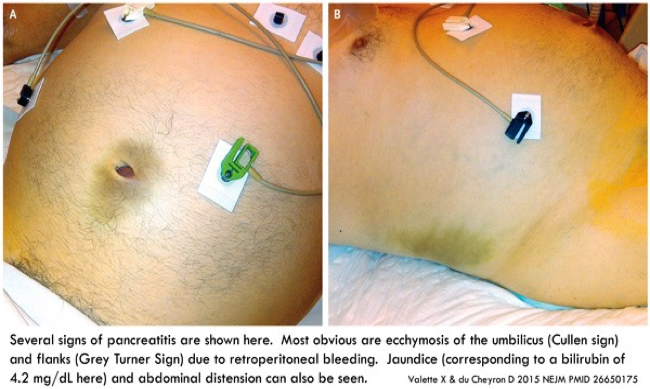
Cullen sign and Grey Turner sign
Amylase and Lipase in Acute pancreatitis
The diagnosis of acute pancreatitis is best supported by a three-fold increase in amylase and lipase.
The lipase is considered a little more specific than amylase but situations other than pancreatitis can cause lipase elevations.
Serum amylase may be elevated for many reasons other than acute pancreatitis (eg, mumps, perforated viscus, tubo-ovarian abscess,), as can the serum lipase (eg, intestinal infarction and perforation, severe peptic ulcer disease).
The severity of pancreatitis does not correlate well with the magnitude of the elevation of the serum amylase or lipase.
Lipase and amylase levels also do not correlate with recovery or prognosis. Z
-
CBC, urea, electrolytes, liver function test, LDH, lipid profile, coagulation profile, serum calcium, C-reactive protein, blood glucose.
-
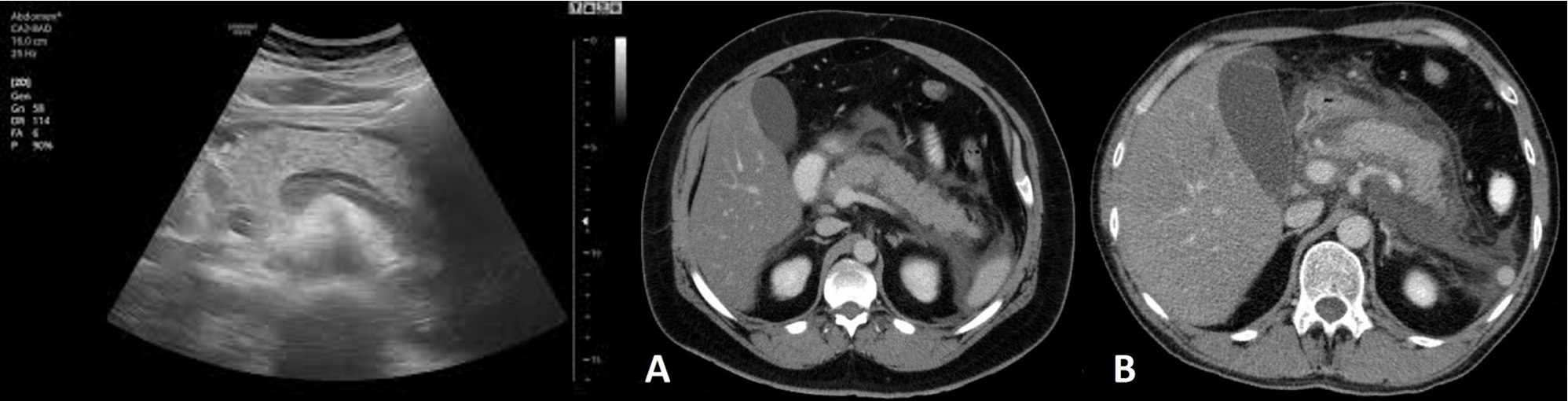
Imaging:
- Chest X-ray: look for pleural effusion, air under the diaphragm in cases of perforated peptic ulcer.
- Ultrasound abdomen: gallstone.
- Abdominal CT: diagnosis, complications of acute pancreatitis, evidence of necrotizing pancreatitis.
CT abdomen Pancreatitis
-
Although a CT scan may eventually be useful, it will not be as helpful as the other choices at this point. It is best used at 72 hours of illness to assess the degree of pancreatic necrosis in patients with predicted severe disease.
-
A cardiogram and troponin will help to rule in or rule out a myocardial infarction while the serum amylase and lipase will give information about pancreatitis.
-
The gallbladder ultrasound will be important in this patient with a strong family history for cholelithiasis and cholecystitis
Pancreatitis: Initial Management
-
All patients with acute pancreatitis should initially be made NPO
-
If they continue to vomit, nasogastric aspiration may be indicated. Vigorous hydration with isotonic fluids (Ringer’s lactate or normal saline) is indicated to maintain blood volume, especially in the face of severe pancreatitis in which patients may sequester large amounts of fluids in the retroperitoneal space.
-
Use of IV antibiotics is controversial. In this patient, antibiotics are not indicated, as the severity of the disease has not been established. Immediate IV hyperalimentation is not required, especially in patients with mild pancreatitis.
Assessment of severity of acute pancreatitis
The aim of severity assessment is the early recognition of the patients with severe pancreatitis and to ensure that they are admitted to a high dependency unit or critical care unit for intensive management.
Ranson’s Criteria Z
The criteria for point assignment is that a certain breakpoint be met at any time during that 48-hour period, so that in some situations it can be calculated shortly after admission. It is applicable to non-gallstone pancreatitis.
1) For non-gallstone pancreatitis, parameters are:
At admission: < 24 HR Z
- Age in years > 55 years
- (WBC) White blood cell count > 16000 cells/mm3
- Blood glucose > 10 mmol/L (> 200 mg/dL)
- Serum AST > 250 IU/L
- Serum LDH > 350 IU/L
Within 48 hours:
- Serum calcium < 2.0 mmol/L (< 8.0 mg/dL)
- Hematocrit fall > 10%
- Oxygen (hypoxemia PaO2 < 60 mmHg)
- BUN increased by 1.8 or more mmol/L (5 or more mg/dL) after IV fluid hydration
- Base deficit (negative base excess) > 4 mEq/L
- Sequestration of fluids > 6 L
2) For gallstone pancreatitis, the parameters are:
At admission:
- Age in years > 70 years
- White blood cell count > 18000 cells/mm3
- Blood glucose > 12.2 mmol/L (> 220 mg/dL)
- Serum AST > 250 IU/L
- Serum LDH > 400 IU/L
Within 48 hours:
- Serum calcium < 2.0 mmol/L (< 8.0 mg/dL)
- Hematocrit fall > 10%
- Oxygen (hypoxemia PaO2 < 60 mmHg)
- BUN increased by 1.8 or more mmol/L (5 or more mg/dL) after IV fluid hydration
- Base deficit (negative base excess) > 5 mEq/L
- Sequestration of fluids > 4 L
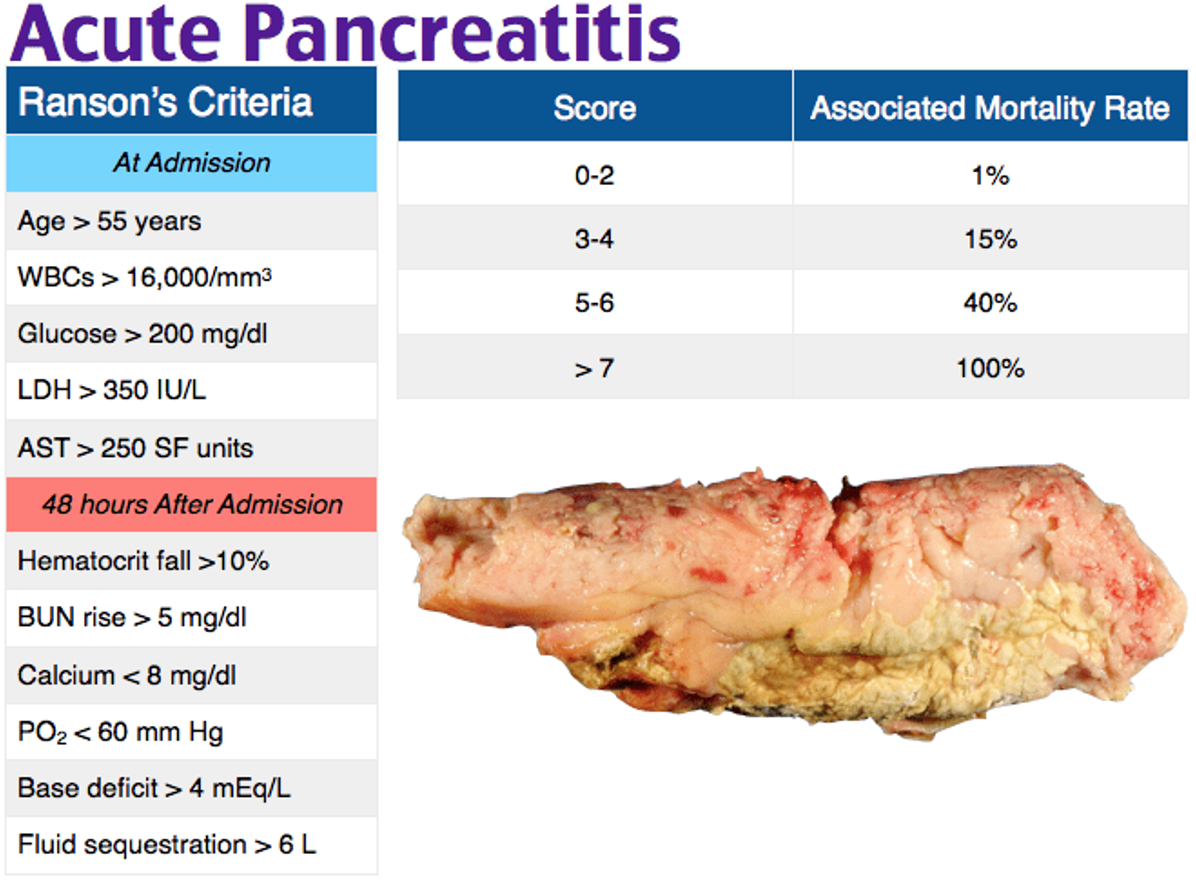
Interpretation of Ranson’s criteria
- If the score ≥ 3, severe pancreatitis is likely.
- If the score < 3, severe pancreatitis is unlikely Or
- Score 0 to 2: 2% mortality
- Score 3 to 4: 15% mortality
- Score 5 to 6: 40% mortality
- Score 7 to 8: 100% mortality..
Alternatively, pancreatitis severity can be assessed by any of the following: Y
- APACHE II score ≥ 8
- Organ failure
- Substantial pancreatic necrosis (at least 30% glandular necrosis according to contrast-enhanced CT)
Treatment
Most attacks of acute pancreatitis will settle with conservative treatment including:
-
NPO +/- NG tube
-
Pain relief: opiates administration
-
Fluid resuscitation: patients with severe pancreatitis require large volumes of fluid to maintain adequate urine output and blood pressure. Adequate early resuscitation in such cases is the most important consideration in early treatment.
-
Antibiotics prophylaxis: it is indicated in severe necrotizing pancreatitis and the recommended antibiotic is imipenem or meropenem
-
Nutritional support: patients with severe pancreatitis who are unable to resume normal oral diets within 72 hours require nutritional support. This is best delivered by an enteral rather than parenteral route.
-
Endoscopic treatment: gallstone pancreatitis is due to the transient impaction of a stone at the papilla causing pancreatic duct obstruction. ERCP with sphincterotomy is indicated in patients with acute pancreatitis with persistent obstructive jaundice with or without cholangitis.
-
Surgical treatment: patients with gallstone-related acute pancreatitis should undergo cholecystectomy (mild pancreatitis during the index admission while severe pancreatitis interval cholecystectomy in 8 – 12 weeks after resolution of the attack of severe acute pancreatitis).
Note: Surgery is indicated in patients with infected necrotizing pancreatitis or in patients with sterile necrotizing pancreatitis who deteriorate and develop progressive multi-organ failure.