a
 Scalp psoriasis Z
Scalp psoriasis Z


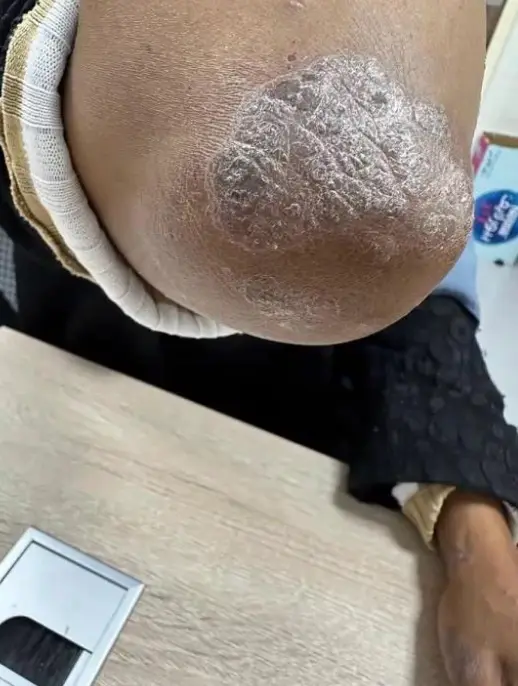
 Plaque psoriasis (Psoriasis vulgaris) The sign is Auspitz’s sign
Plaque psoriasis (Psoriasis vulgaris) The sign is Auspitz’s sign
 Generalized Psoriasis
Generalized Psoriasis
Psoriasis CS-OSPE
Well demarcated + extensive + erythematous = always psoriasis until proven otherwise In the extensor parts of knee or elbow, red patches of skin maybe pain.
Description of Lesions: Z
- Silvery plaque scales localized in extensor surfaces (e.g., knees, elbows).
- Well-demarcated.
- Erythematous.
- Plaque with silvery scales (micaceous scale).
- Dry, scaly plaques.
- Crusted (can be).
- For Scalp Psoriasis: Erythematous Silvery scaly plaques extending beyond the hair lines; typically no hair loss.
- Nail involvement: Pitting nails.
Diagnosis:
- Psoriasis
- Scalp psoriasis
- Plaque psoriasis (Psoriasis vulgaris)
- Generalized Psoriasis
Differential Diagnosis (DDx):
- Chronic eczema / Chronic Dermatitis
- Chronic Allergic Contact Eczema (Related to slippers, especially if itchy)
- Seborrheic Dermatitis
- Pityriasis rosea
- Lichen planus
- Drug eruption
Signs & Confirmation:
- Ausbitz sign (pin point bleeding)
- Crown sign (for Scalp psoriasis)
- Psoriasis is characterized by: Acanthosis
Koebner Phenomenon:
- It is induction of lesion in normal skin after trauma. It is seen in lichen planus, wart, psoriasis and vitiligo.
Treatment (Tt) / Management:
- Full History & Examination
- Education
- Topical:
- Vit D (e.g., Calcipotriol)
- Salicylic acid
- PUVA Tac (Topical PUVA/Calcineurin inhibitors)
- Topical CS super potent / Topical CS (Corticosteroids)
- Emollients (for dryness) - Ointment is used because dry skin needs moisturizing.
- Light Therapy:
- Excimer laser
- PUVA (Psoralen plus UVA)
- Laser therapy
- Systemic (If generalized): Z
- Systemic immunosuppressives
- Biologics
- Cyclosporine
- General Advice:
- Avoidants (if related to contact irritants)
Complications:
- Erythroderma / Erythrodermic psoriasis (skin failure)
- Psoriatic arthritis
- Obesity
Variants / Types:
- Plaque Or vulgaris
- Pustular; Sterile pus (can occur after withdrawal of systemic steroid)
- Guttate;
- Age: adolescents
- Post-streptococcal
- Tt: PUVA
- Inverse (Inversus); In moist areas
- Generalized
- Palmoplantar
- Arthritis (Psoriatic arthritis)
- Erythrodermic psoriasis
Important Sites to Examine for Confirmation: Z
- Other elbow
- Knees
- Back
- Scalp
- Nails - nail pitting (associated with psoaritic arthritis)
- Genitals
- Hidden areas like between fingers or toes
Special Considerations / Questions:
- Can we give prednisolone?
- Contraindicated, may cause pustular exacerbation.
- To treat it we could use all these topical except?
- Metronidazole


Koebner phenomenon of psoriasis Z
Where else would you find Koebner phenomenon?
- Psoriasis
- Lichen planus
- Warts
- Vitiligo
Koebner phenomenon is defined as the appearance of a primary skin condition in the site of a trauma.
Diagnosis:
- Psoriasis due to Koebner Phenomenon.
Clinical Presentation:
- Well demarcated.
- Erythematous plaque.
- Silver scaly.
Investigation/Clinical Sign:
- Auspitz sign.
Pathology:
- Increased rate of epidermal turnover (thickening).
- The accelerated rate of movement through the epidermis doesn’t allow adequate time for differentiation, which is recognized as scale.
Treatment:
- Localized disease: Topical treatments
- Tar.
- Corticosteroids.
- Calcipotriene (vitamin D analogues).
- Tacrolimus and pimecrolimus.
- Tazarotene.
- Intense light or laser therapy (excimer laser 308 nm).
- Generalized disease: Phototherapy & Systemic therapy
- PUVA and Narrow band UVB.
- Methotrexate: immune compressor (stops T-cells).
- Acitretin: vitamin A.
- Cyclosporine: immune suppressor.
- Biologics.
- Humira.









Plaque Psoriasis (Psoriasis Vulgaris)
This is the most common form of psoriasis, characterized by well-demarcated plaques.
Case ScenariosL
- “35 years came with lesions started before years and become thicker his grandpa had same conditions in elbows.”
- “An obese, heavy smoker 35-year-old, a hypertensive far east Asian woman who had well-demarcated plaques on his elbows for more than 2 years. Her chronic dermatology disease is controlled with topical treatments, wanes, and waves throughout this period.”
- “A 27 Y/O male presents with worsening of a prior chronic mild rash. He has no systemic complaints. Skin exam is notable for scaly, red plaques as shown.”
- “Yassir is a 35 Y/O officer came to the dermatology clinic complaining of two lesions each on the knees, the condition started 9 months ago as small elevations enlarged to reach their current size. These lesions are not itchy and he mention that his grandpa has similar lesions on his elbows.”
1. Describe the lesion:
- Well-demarcated (or well-circumscribed)
- Erythematous plaque (red, raised patch)
- With a silvery scale (often thick, silvery-white)
- Common locations: Knees, elbows, gluteal cleft, scalp (below hairline), inside the ear.
2. What is the diagnosis?
- Psoriasis (specifically, Psoriasis Vulgaris or Plaque Psoriasis)
3. Signs to confirm the diagnosis:
- Auspitz sign: Pinpoint bleeding when scales are removed.
4. Two other different areas in the body you have to check for the presence of psoriasis:
- Nails (e.g., pitting, onycholysis)
- Scalp
- Elbows
- Gluteal cleft (intergluteal fold)
5. Two Associated diseases/Risk factors:
- Obesity
- Cardiac condition / Hypertension
- Smoking
- Arthritis (Psoriatic Arthritis)
6. Give at least one general treatment for the case:
- Topical Treatments:
- Topical corticosteroids
- Tar (e.g., Coal tar)
- Calcipotriene (Vitamin D analogues)
- Tacrolimus and pimecrolimus (calcineurin inhibitors)
- Tazarotene (Vitamin A derivative)
- Phototherapy:
- Excimer laser (308 nm wavelength)
- PUVA (Psoralen plus Ultraviolet A)
- Narrow band UVB
- Systemic Treatments (for moderate to severe cases or complications):
- Methotrexate (immunosuppressant) Z
- Acitretin (oral retinoid, Vitamin A derivative)
- Cyclosporine (immunosuppressant)
- Biologics (e.g., Humira, Adalimumab, which target specific parts of the immune system like IL-23).
7. Patient Education:
- The disease is not curable but manageable.
- It is not contagious.




Erythrodermic Psoriasis
This is a severe, widespread form of psoriasis involving generalized erythema and scaling, often covering more than 90% of the body surface. It is a dermatological emergency.
Case Scenarios (Examples):
- “An obese, heavy smoker 35-year old woman who had well-circumscribed plaque on her elbow for the last two years. Her chronic dermatology disease is controlled with topical treatment. She presented to the ER with generalized erythema all over her body. 12 days ago she developed respiratory allergy responded to a shot regimen of oral prednisolone by a respiratory physician.”
- “A 40-year-old man presented to the ER with generalized redness involving all the body. The condition started gradually throughout the last week and got worse. One week before the current situation, he completed a course of oral systemic Prednisolone (steroid) prescribed by a chest physician due to allergy. He is shivering and the body is full of scales. There are thick, well-demarcated plaques on his elbows and knees for ten months.”
- “At midnight you have been called by the ER – resident to consult you about a 35 Y/O man who brought in by his brother due to generalized redness of the body that almost involved all his body… When you examined him, he was shivering. With a lot of scales on his body and you noticed small two thick well demarcated plaques on his elbows, he said they were here for six months.”
1. What is the diagnosis of the acute case?
- Erythrodermic Psoriasis (or Psoriatic Erythroderma).
2. What is the probable cause of the condition?
- Withdrawal of systemic corticosteroids (e.g., oral prednisolone) in a patient with pre-existing psoriasis. This can trigger a rebound flare leading to erythrodermia.
3. Name two other conditions that can be complicated with generalized skin redness (erythrodermia):
- Drug Eruption (Drug Hypersensitivity Syndrome)
- Atopic Dermatitis (Severe/Chronic Eczema)
- T-cell cutaneous lymphoma (e.g., Mycosis fungoides)
- Leukemia
- Lymphoma
4. What is the most serious complication that may develop / Leading cause of death among these types of patients?
- High cardiac output failure
- Septicemia (due to skin barrier breakdown and infection)
- Fluid and electrolyte imbalance
- Hypothermia (due to extensive skin involvement and heat loss)
5. How would you manage the patient?
- Admission to ICU/Hospitalization: For close monitoring and supportive care.
- Monitor Hemodynamic Changes: Assess vital signs, blood pressure, pulse.
- Fluid and Electrolyte Replacement: Correct fluid and electrolyte imbalances (e.g., due to increased evaporative loss through damaged skin).
- Thermoregulation: Maintain body temperature (patients are prone to hypothermia or hyperthermia).
- Prevention of Complications: Watch for signs of infection, cardiac issues.
- Topical Therapy: Emollients to soothe and moisturize; mild topical steroids may be used cautiously.
- Systemic Treatment (for the underlying psoriasis, once stable):
- Systemic immunosuppressants (e.g., Methotrexate, Cyclosporine) Z
- Biologics
- Oral retinoids (e.g., Acitretin)
- Phototherapy (e.g., PUVA) can be considered once the acute phase is controlled and temperature is stabilized.

 Generalized pustular psoriasis (admission); acute skin failure
Generalized pustular psoriasis (admission); acute skin failure
 Localized pustural psoriasis
Localized pustural psoriasis



Pustular Psoriasis
A severe form of psoriasis characterized by widespread pustules (small, yellow-white, non-infectious bumps filled with pus).
Case Scenario (Example):
- “An obese, heavy smoker 35-year-old… She presented to the ER unit with generalized fatigue, fever, and widespread yellowish eruption. Twelve days before her current presentation, she developed a respiratory allergy responded to a short regimen of oral prednisolone by a respiratory physician.”
1. What is the diagnosis of her acute dermatological condition?
- Pustular Psoriasis.
2. Generally, what are the two types of this acute condition?
- Generalized Pustular Psoriasis (GPP): Can involve the entire body, often associated with systemic symptoms like fever and fatigue.
- Localized Pustular Psoriasis: Typically affects specific areas like palms and soles (Palmoplantar Pustulosis).
3. What is possible causes/Explain the development of the acute condition?
- Withdrawal of systemic corticosteroids (common trigger).
- Infections
- Pregnancy
- Strong topical irritants
4. The common causes of death are:
- Septicemia
- Fluid and electrolyte imbalance
- Cardiac complications
5. Mention two treatments you can use to treat her acute dermatological condition:
- Systemic treatments are often required for generalized forms:
- Oral retinoids (Acitretin)
- Methotrexate
- Cyclosporine
- Biologics
- Supportive care: Fluid and electrolyte balance, infection control.
- Phototherapy: May be used cautiously, sometimes combined with systemic treatments.
- Topical steroids: Can be used as adjuncts for localized disease or milder flares._
- Vitamin D derivatives: (e.g., calcipotriene) for milder or localized forms.


Guttate Psoriasis
- Diagnosis:
- Guttate Psoriasis.
- Clinical Presentation:
- Well demarcated.
- Small drop-like erythematous plaque.
- Silver scaly.
- In trunk.
- Investigation/Clinical Sign:
- Auspitz sign.
- Pathology:
- Increased rate of epidermal turnover (thickening).
- The accelerated rate of movement through the epidermis doesn’t allow adequate time for differentiation, which is recognized as scale.
- Group A beta hemolytic streptococcal infections.
- URTI (Upper Respiratory Tract Infection).
- Treatment:
- Localized disease: Topical treatments.
- Tar.
- Corticosteroids.
- Calcipotriene (vitamin D analogues).
- Tacrolimus and pimecrolimus.
- Tazarotene.
- Intense light or laser therapy (excimer laser 308 nm).
- Generalized disease: Phototherapy & Systemic therapy.
- PUVA and Narrow band UVB.
- Methotrexate: immune suppressor (stops the T cells).
- Acitretin: vitamin A.
- Cyclosporine: immune suppressor.
- Biologics.
- Humira.
- Localized disease: Topical treatments.
Characterized by small, drop-like (guttate) lesions, often triggered by a bacterial infection like strep throat.
1. Give 2 different variants (including Guttate):
- Guttate Psoriasis
- Pustular Psoriasis
- Erythrodermic Psoriasis
- Inverse Psoriasis (affects skin folds)
- Psoriatic Arthritis
Psoriatic Arthritis
An inflammatory arthritis associated with psoriasis, affecting joints and often presenting with dactylitis (sausage fingers/toes) or nail changes.
Patient Case
30 years old patient presented to rheumatology department complaining of joint inflammation and morning stiffness, rheumatoid factor was negative. After full examination the doctor found scaly lesion on erythematous base in the lower back the patient mentioned she had this lesion for several months and was responding to topical treatment
Q1 - write to differential diagnosis?
- A- Psoriasis
- B- Lichen planus
Q2 - another place you should examine?
- A- Nails
Q3 - What is the diagnosis?
- Psoriatic arthritis
Describe?
- Well demarcated.
- Symmetrical.
- Bilateral.
- Erythematous plaque.
- Silver scaly.
- Nails: pitting nails, nails with hyperkeratosis.
Investigation/Clinical Sign:
- Auspitz sign.
- X-ray: pencil in cup appearance.
Treatment:
- Localized disease:
- Topical treatments:
- Tar.
- Corticosteroids.
- Calcipotriene (vitamin D analogues).
- Tacrolimus and pimecrolimus.
- Tazarotene.
- Intense light or laser therapy (excimer laser 308 nm).
- Topical treatments:
- Generalized disease:
- Phototherapy & Systemic therapy
- PUVA and Narrow band UVB.
- Methotrexate: immune suppressor (stops the T cell).
- Acitretin: vitamin A.
- Cyclosporine: immune suppressor.
- Biologics.
- Humira.
- Phototherapy & Systemic therapy
Q5 - Mention findings in histopathology?
- Parakeratosis
- Munro microabscess
- Rete ridges
- Loss of granular layer
- Increased rate of epidermal turnover (thickening).
- The accelerated rate of movement through the epidermis doesn’t allow adequate time for differentiation, which is recognized as scale.
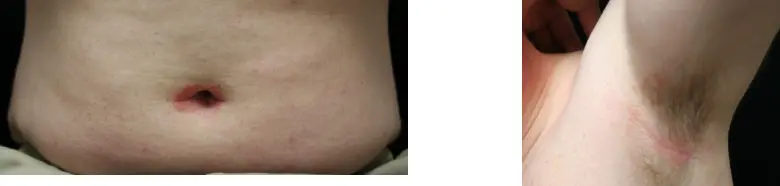


Inverse psoriasis (in the folds)
What is the diagnosis?
- Inverse psoriasis (in the folds).
What is the clinical presentation?
- Erythematous plaque.
- Silver scaly.
What are the key investigations/clinical signs?
- Auspitz sign.
What is the pathology?
- Increased rate of epidermal turnover (thickening).
- The accelerated rate of movement through the epidermis doesn’t allow adequate time for differentiation, which is recognized as scale.
What is the treatment?
- Localized disease: Topical treatments.
- Tar.
- Corticosteroids.
- Calcipotriene (vitamin D analogues).
- Tacrolimus and pimecrolimus.
- Tazarotene.
- Intense light or laser therapy (excimer laser 308 nm).
- Generalized disease: Phototherapy & Systemic therapy.
- PUVA and Narrow band UVB.
- Methotrexate: immune suppressor (stops T cell activity).
- Acitretin: vitamin A derivative.
- Cyclosporine: immune suppressor.
- Biologics.
- Humira.

 -
-  -
- 
