NEONATAL JAUNDICE
Prepared by : DR. SALMA ELGAZZAR MRCPI in pediatrics Master’s degree in Pediatrics Alexandria University
OBJECTIVES:
- Define hyperbillirubenimeia.
- Recall the physiological steps in the metabolism of bilirubin.
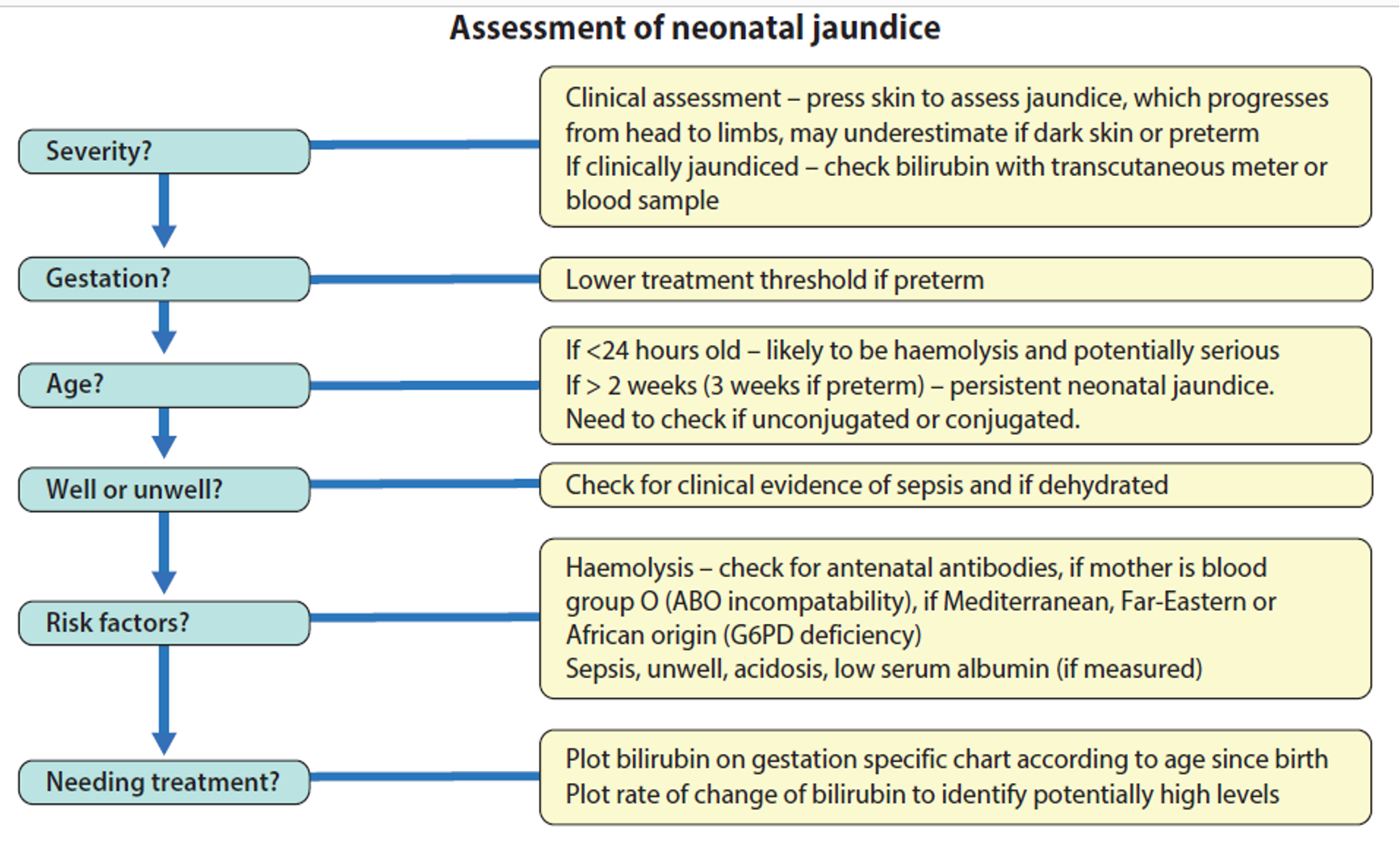
- List the key component from the history and physical examination in patient with jaundice.
- Differentiate between physiological and pathological causes of jaundice.
- Discuses the differential diagnosis of both direct and indirect hyperbillrubinemia.
- Define and enumerate the laboratory findings in cholestatic jaundice.
- List the commonest causes of cholestatic jaundice in infancy and childhood.
- Discuss the pathogenesis, clinical presentation and outline the management of biliary atresia.
- Elaborate on the different treatment modalities in jaundice and list the common indications and side effects of each.
- Describe the most fatal complications of hyperbillrubinemia.
Other Presentation
COMMON CAUSES OF UNCONJUGATED HYPERBILIRUBINEMIA
1- Pathological Jaundice
2- Physiological Jaundice
3- Jaundice breast milk
4- Hemolytic disease of the newborn
5- Syndromes of Jaundice
CONJUGATED HYPERBILIRUBINEMIA
DEFINITION
Jaundice is yellow discoloration of the skin, sclera and mucous membranes due to increased level of bilirubin in the blood. Jaundice is clinically observed in the newborn when the total serum bilirubin reaches 5-7 mg/dl (86 μmol per L)
Over 60% of term and 80% of preterm infants develop jaundice in the first week of life, few have significant underlying disease.
Metabolism of bilirubin
peleverdin peroxidase to unconjugated billirubin (water insoluble / lipid soluble; can pass brain barrier)
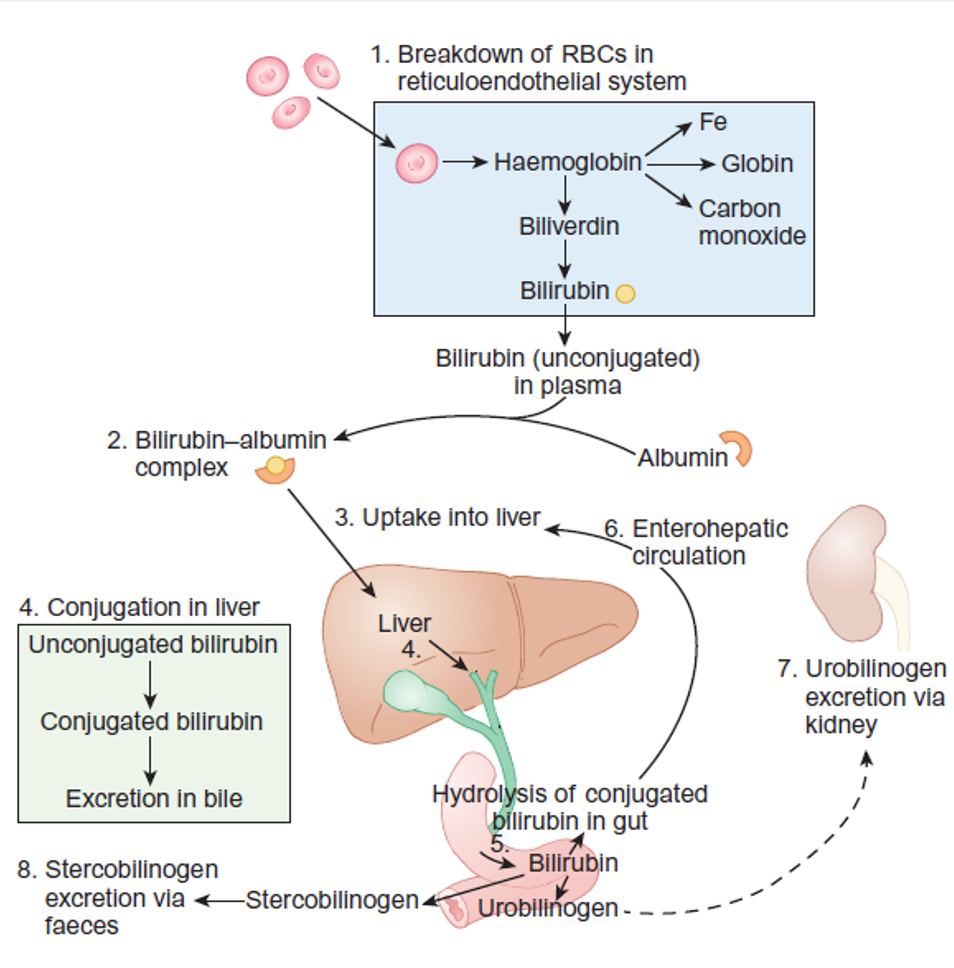
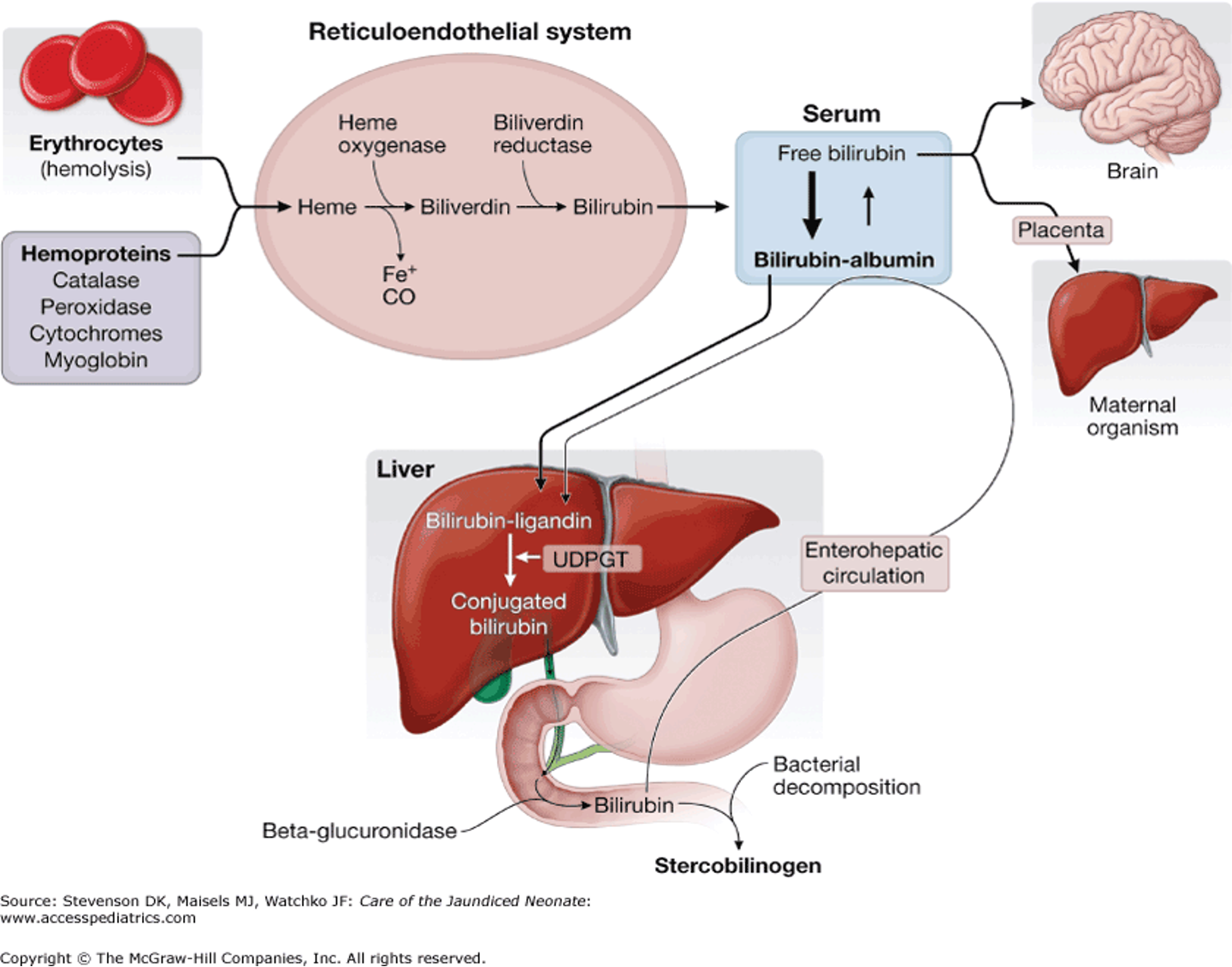
PATHOGENESIS OF HYPERBILIRUBINEMIA
- Increased bilirubin production due to high red cell turn over.
- Delayed bilirubin clearance.
- Conjugated hyperbilirubinemia.
Classification of jaundice
CAUSES OF HYPERBILIRUBINEMIA
Unconjugated Hyperbilirubinemia:
- ABO incompatibility
- Rh isoimmunization
- G6PD deficiency
- Cephalhematoma or extensive bruising
- Hemoglobinopathies or other RBC membrane defects
- Gilbert’s syndrome & Crigler-Najjar syndrome
- Hypothyroidism
- Breastfeeding jaundice
- Breast milk jaundice
- Ileus
- Intestinal obstruction
- UTI
Conjugated Hyperbilirubinemia:
- Biliary atresia
- Choledochal cyst
- Alagille syndrome
- Tyrosinemia
- Galactosemia
- Sepsis
- TORCH infection
- Idiopathic neonatal hepatitis
- Parenteral nutrition related cholestasis
Jaundice starting at <24 hours of age:
- Haemolytic disorders:
- Rhesus incompatibility
- ABO incompatibility
- G6PD deficiency
- Spherocytosis, pyruvate kinase deficiency
- Congenital infection
Jaundice at 24 hours to 2 weeks of age:
- Physiological jaundice
- Breast milk jaundice
- Infection, e.g., urinary tract infection
- Haemolysis, e.g., G6PD deficiency, ABO incompatibility
- Bruising
- Polycythaemia
- Crigler–Najjar syndrome
Causes of prolonged (persistent) neonatal jaundice
Unconjugated:
- Breastmilk jaundice
- Infection (particularly urinary tract)
- Haemolytic anaemia, e.g., G6PD deficiency
- Hypothyroidism
- High gastrointestinal obstruction
- Crigler–Najjar syndrome
Conjugated (>25 µmol/L): Bile duct obstruction:
- Biliary atresia
- Choledochal cyst
Neonatal hepatitis syndrome:
- Congenital infection
- Inborn errors of metabolism
- α₁-Antitrypsin deficiency
- Galactosaemia
- Tyrosinaemia (type 1)
- Errors of bile acid synthesis
- Progressive familial intrahepatic cholestasis
- Cystic fibrosis
- Intestinal failure-associated liver disease (associated with long-term parenteral nutrition)
Intrahepatic biliary hypoplasia:
- Alagille syndrome
HISTORY
- Onset of jaundice
- Blood group of mother and baby.
- Flu-like illness or skin rash during pregnancy (congenital infection)
- Maternal drug intake.
- Birth trauma with bruising and/or fractures
- Delayed cord clamping.
- Family history of neonatal jaundice.
- Loss of stool color.
- Greater than average weight loss
- Symptoms of hypothyroidism
- Symptoms of metabolic disease (eg, galactosemia)
- Exposure to total parental nutrition
- Types of feeds –breast or bottle.
- Use of drugs and herbal remedies in the lactating mother
EXAMINATION
Signs to Look For
| Category | Signs |
|---|---|
| Jaundice | Jaundice first appears in the sclera and face and progresses cephalocaudally, appearing last on the feet and soles. Examination of blanched skin in natural light may be helpful. It is more difficult to detect in preterm and dark-skinned infants. Dermal pressure may reveal the anatomic progression of jaundice (face, approximately 5 mg/dL; mid-abdomen, 15 mg/dL; soles, 20 mg/dL). |
| General | - Dysmorphic features (Alagille syndrome) - Obese and plethoric (infant of diabetic mother) |
| Head | - Microcephaly (congenital infections) - Cephalhematoma - Large fontanelle (hypothyroidism) |
| Eye | - Cataract (galactosemia) - Chorioretinitis (congenital infections) |
| Mouth | - Large protruding tongue (hypothyroidism) |
| Skin | - Bruises - Purpura - Petechiae (congenital infections) |
| Abdomen | - Hepatosplenomegaly (congenital infections, hemolytic anemia) |
| Umbilicus | - Infection - Hernia (hypothyroidism) |
 |
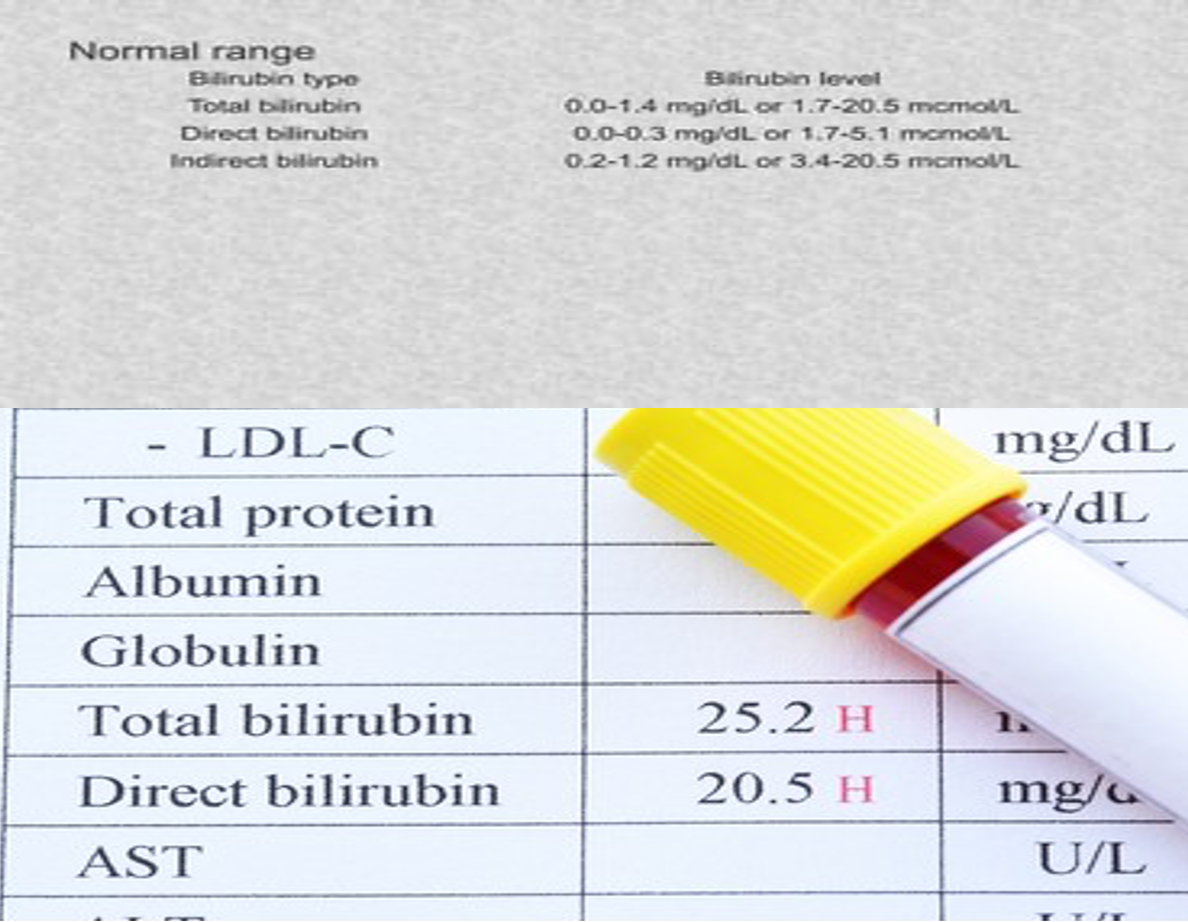
INVESTIGATIONS
- Serum bilirubin
- Hematocrit
- Blood group and Rh type of mother and baby
- Direct agglutination (Coombs) test
- Investigations to determine the underlying pathology should include:
- Full blood count
- Peripheral blood film
- Sepsis work-up to include culture of blood, urine, and cerebrospinal fluid (as indicated)
- G6PD levels depending on ethnicity of parents
The transcutaneous bilirubin meter
 The transcutaneous bilirubin meter:
Can be used in babies of 35 weeks’ gestation or more after 24 hours of age.
It uses multi wavelength reflectance.
The transcutaneous bilirubin meter:
Can be used in babies of 35 weeks’ gestation or more after 24 hours of age.
It uses multi wavelength reflectance.
There is good correlation with serum bilirubin level up to 250 μmol/L. It is a useful screening tool and can be helpful in community and postnatal wards.
The value should be plotted on the nomogram to assess the risk level and if treatment is indicated
TREATMENT OF NEONATAL JAUNDICE
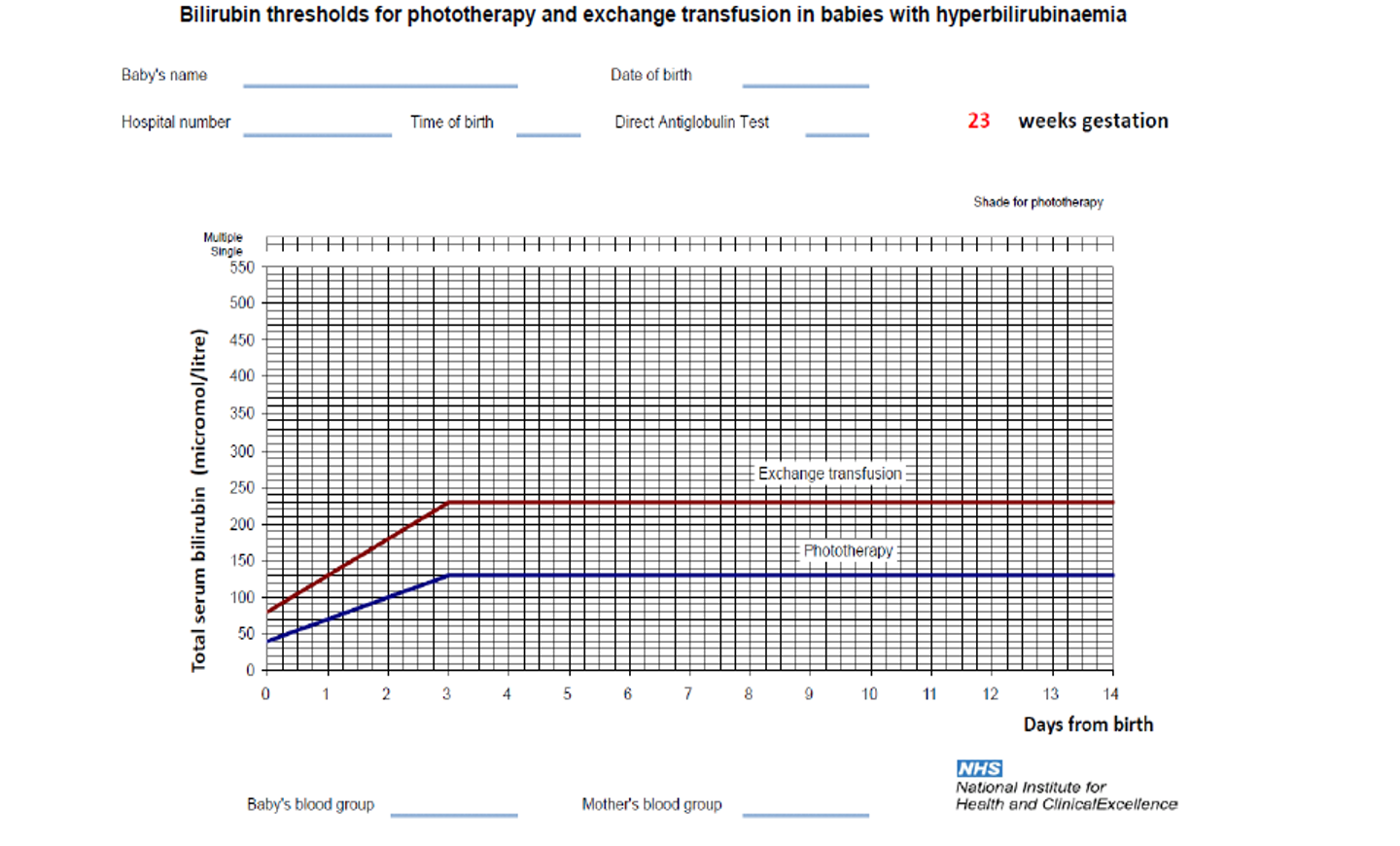
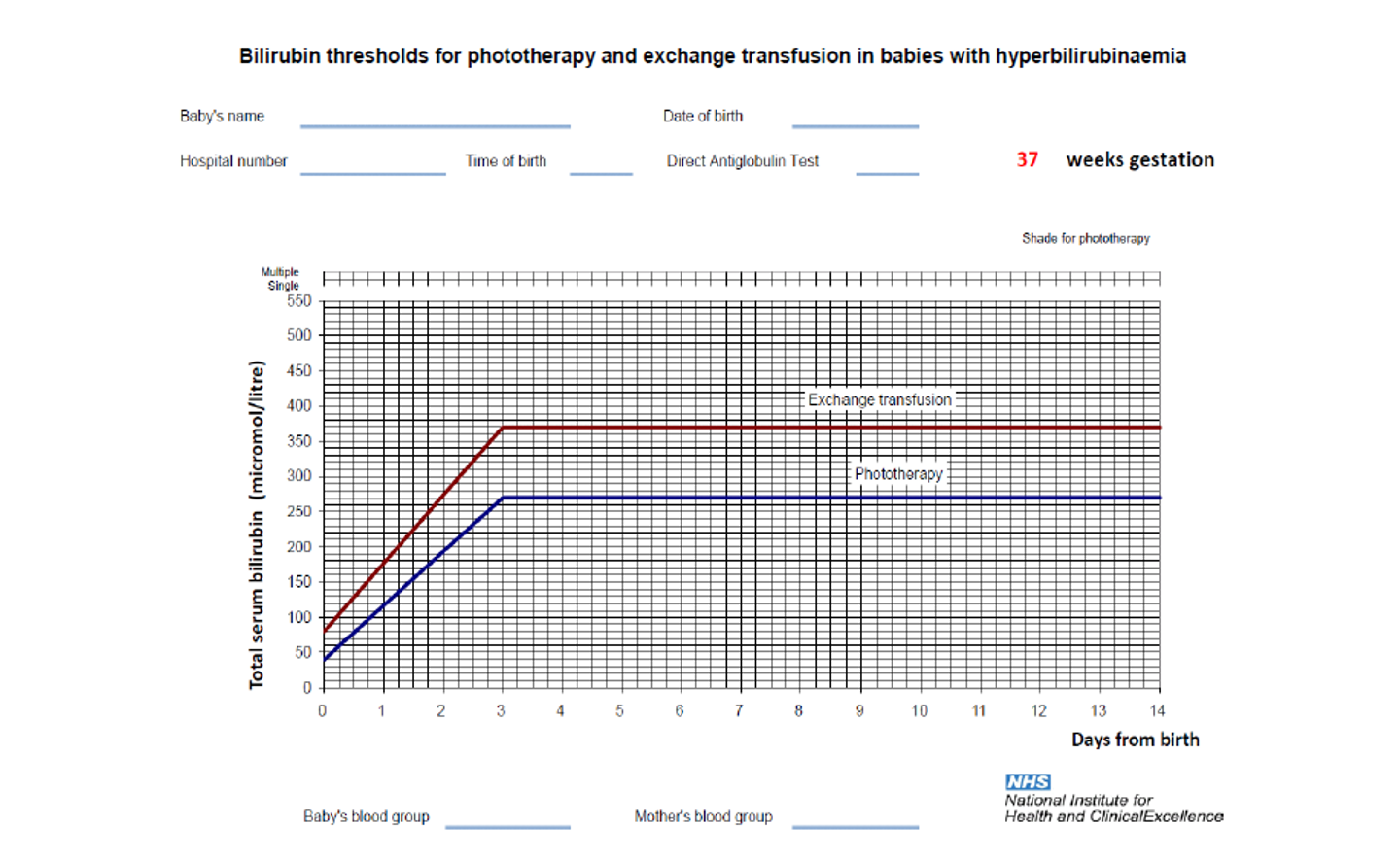
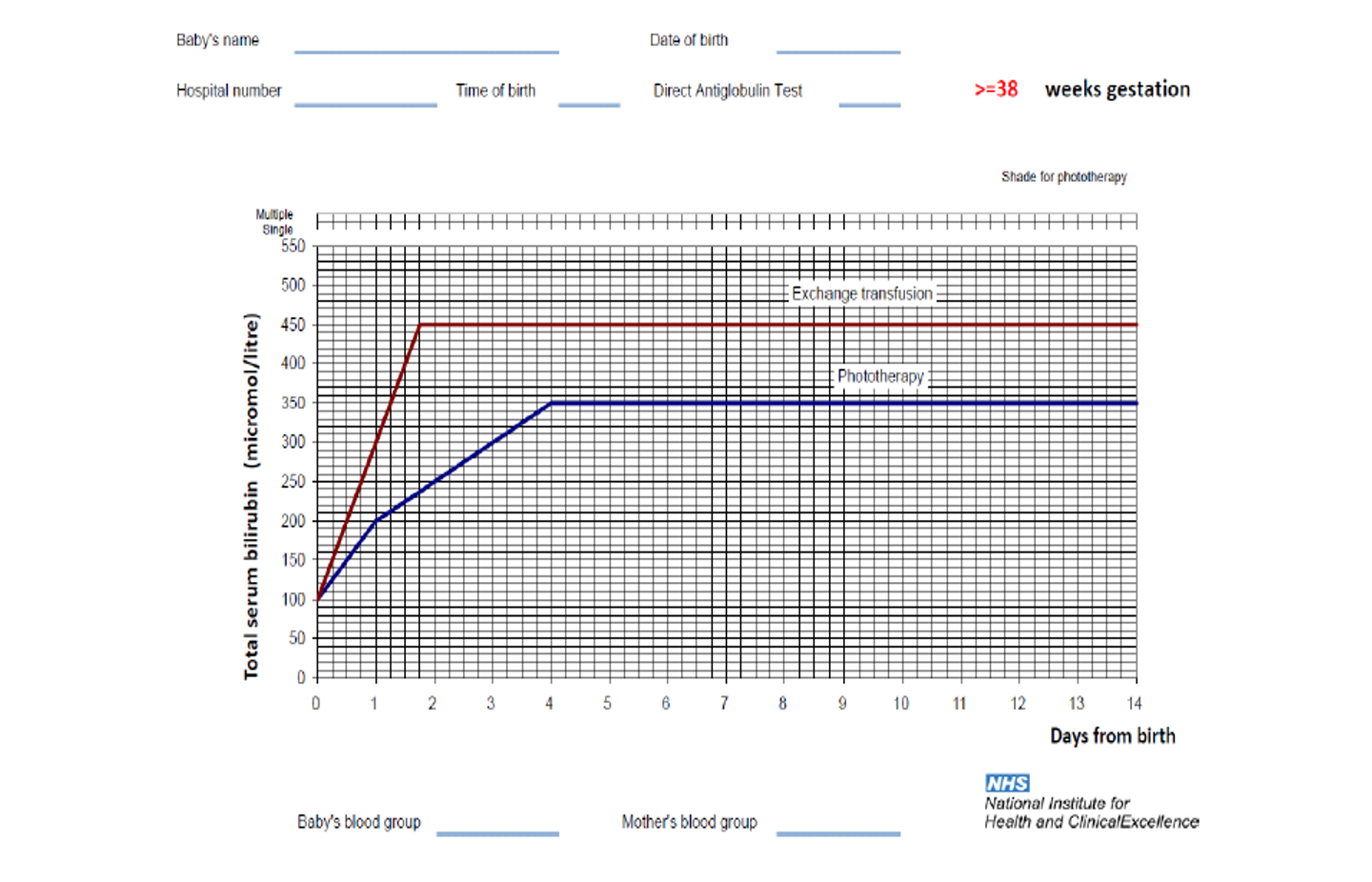
The type of treatment depends on the bilirubin level and its rate of rise, gestational age, and if other risk factors are present.
Feeding: More frequent feeding.
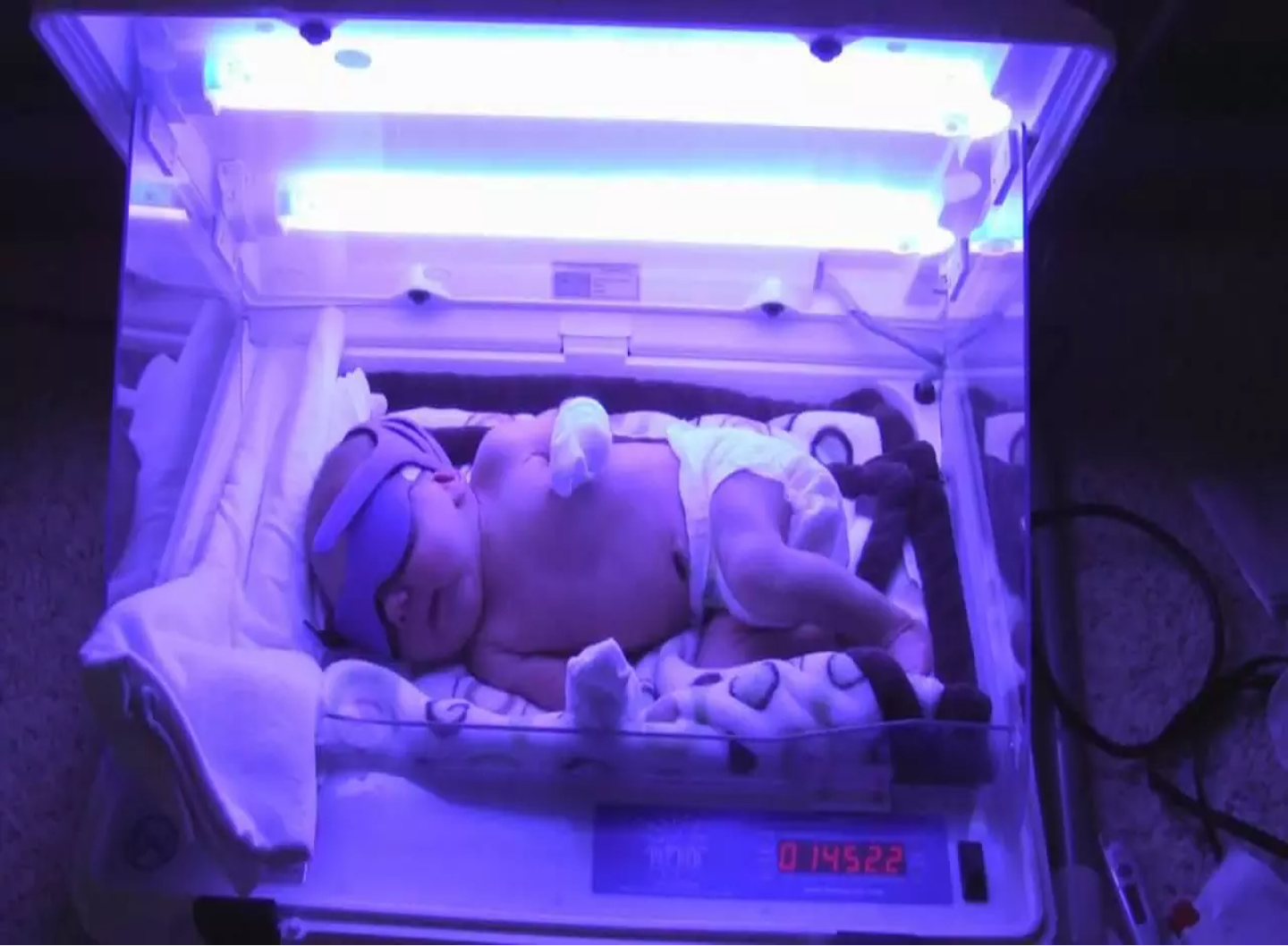
Phototherapy:
-
Clinical jaundice and indirect hyperbilirubinemia are reduced by exposure to high-intensity light in the visible spectrum. Bilirubin absorbs light maximally in the blue range (420-470 nm).
-
Phototherapy works by converting bilirubin into a water soluble compound called lumirubin, which is excreted in the urine or bile.
-
Continuous multiple (intensive) phototherapy is given if the bilirubin is rising rapidly or has reached a high level.
Complications of phototherapy
- Insensible water loss (increase fluid intake or the volume and frequency of feeding).
- Phototherapy may be associated with loose stool.
- Retinal damage (covering the eye is a routine during phototherapy).
- Temperature instability as the infant is undressed.
- A macular rash, and bronze discoloration of the skin if the jaundice is conjugated.
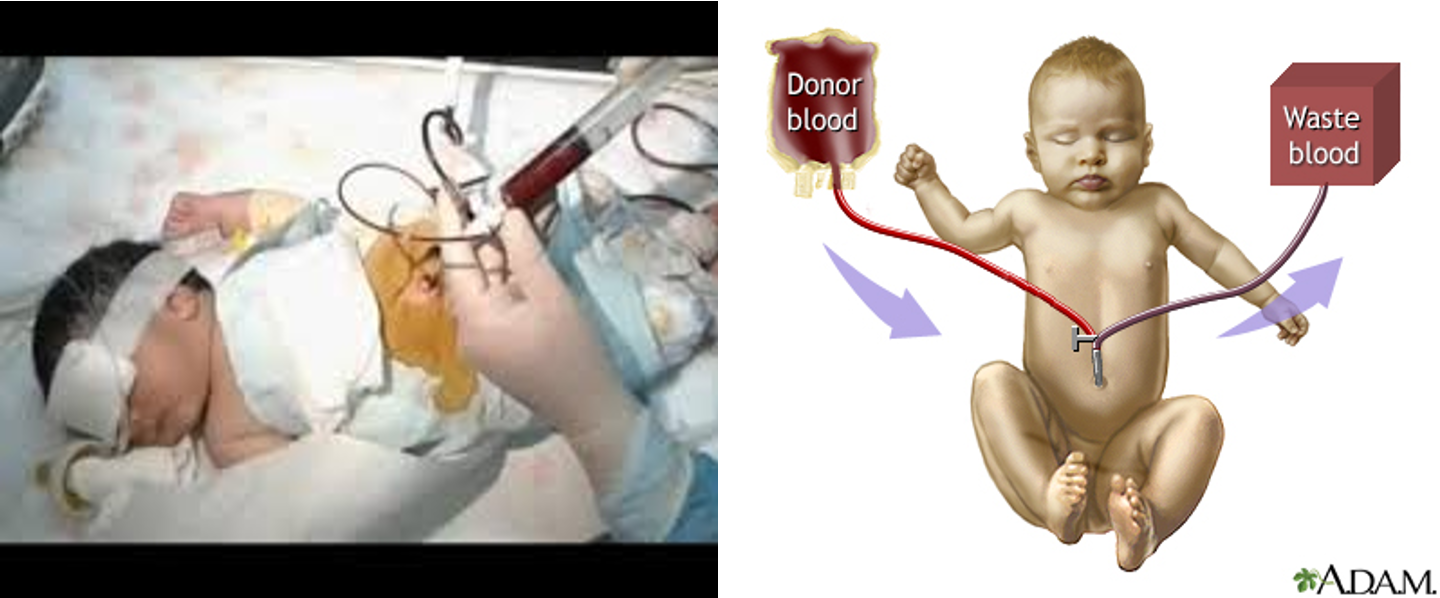
Exchange transfusion
-
Required if the bilirubin rises to levels that are considered potentially dangerous.
-
Blood is removed from the baby in small aliquots (usually from an arterial line or the umbilical vein) and replaced with donor blood (via peripheral or umbilical vein).
-
Usually, twice the infant’s blood volume (2 × 90 ml/kg) is exchanged.
-
Donor blood should be as fresh as possible and screened to exclude cytomegalovirus, hepatitis B and C and HIV infections.
-
The procedure does carry some risk of morbidity and mortality.
-
Phototherapy has been very successful in reducing the need for exchange transfusion.
-
In infants with rhesus hemolytic disease or ABO incompatibility unresponsive to intensive phototherapy, intravenous immunoglobulin reduces the need for exchange transfusion.
PHARMACOLOGICAL TREATMENT OF JAUNDICE
PHENOBARBITONE
- Phenobarbitone induces hepatic UGT enzyme and hence the conjugation of the bilirubin. It may also increase the hepatic uptake of bilirubin.
- It acts very slowly and does not lower serum bilirubin levels fast enough to be clinically helpful.
INTRAVENOUS IMMUNOGLOBULIN
- High-dose intravenous immunoglobulin (IVIG) is effective in reducing the bilirubin levels and reduces the need for exchange transfusion in neonates with Rhesus or ABO immune hemolytic disease.
- Used as an adjunct to intensive phototherapy if the serum bilirubin continues to increase more than 8.5 μmol/L/hour.
- In isoimmune haemolysis, red blood cells are destroyed by an antibody dependent cytotoxic mechanism mediated by Fcreceptor-bearing cells of the neonatal reticuloendothelial system.
- The mechanism of IVIG action is nonspecific blockade of Fc receptors, which reduces red cell breakdown.
- Maternal IVIG administration also reduces fetal hemolysis.