Radiology in Gynaecology
By Dr. Mona Ahmed


1st Case
Mrs Huda is 28 years old PG. GA is 36 weeks came for routine follow up. Has no complain was regular follower. you did US you find single cephalic baby fundal placenta with –ve FH.
What is your diagnosis?
IUFD
What are other things you may suspect to be found in ultrasound?
Robert sing./ Buda sign /Spalding sign /oligohydra
Is there any other radiological tools you c Xray
2nd Case
Sammar is 18 years old. came c/o primary Amenorrhoea
you did ultrasound you find no uterus
What is other things you will look & examination
What are other things you will look for?
What is next step to confirm your diagnosis?

MRI Done Revealed
absent uterus and ovaries with short vagina (MERK). No associated renal anomalies
How will you manage?
- Explore diagnosis
- Reassurance
- Hormonal treatment(Induce pupperty)(HRT)
- Surgical treatment.
What is Medical Imaging?
- MEDICAL IMAGING: is the technique and process used to create images of the human body.
- Aiming
- for clinical purposes (medical procedures seeking to reveal, diagnose, or examine disease)
- or medical science (including the study of anatomy and physiology)
Imaging Methods in Gynaecology
- Ultrasonography
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Conventional radiology (PET)
- Angiography.
- Hysterosalpingogram (HSG).
- Cystourethrogram.
- Hysteroscopy.
- X-Ray.
CT Scan
- The diagnostic quality of pelvic scans is improved with use of oral & IV contrast.
- Oral contrast media is used to differentiate between the bowel and adjacent structures.
- IV contrast media used for bloc mass & lymph nodes.
- The fallopian tubes & ovaries

CT Scan
appropriate for detection of
- ovarian tumors
- less appropriate for examination of uterus

MRI
Advantages over CT scan and ultrasonography:
- non-invasiveness.
- Without repositioning the patient.
- More sensitivity to flowing

MRI
- Study of normal uterus and ad
- Myoma.
- Adenomyosis.
- Congenital uterovaginal anomalies.
- Gynaecological cancers.
- Pregnancy --- complicated by
- Endometriosis.
- Retroperitoneal lymph node.
Contraindications for MRI
- prosthetic heart valves
- Claustrophobia.
- Pacemakers.
- Contrast allergy.
- Body weight (MRI tables not suite overweight).
Conventional Radiology Uses
- Calcifications
- Gas distribution
- Skeleton
- IUD detection

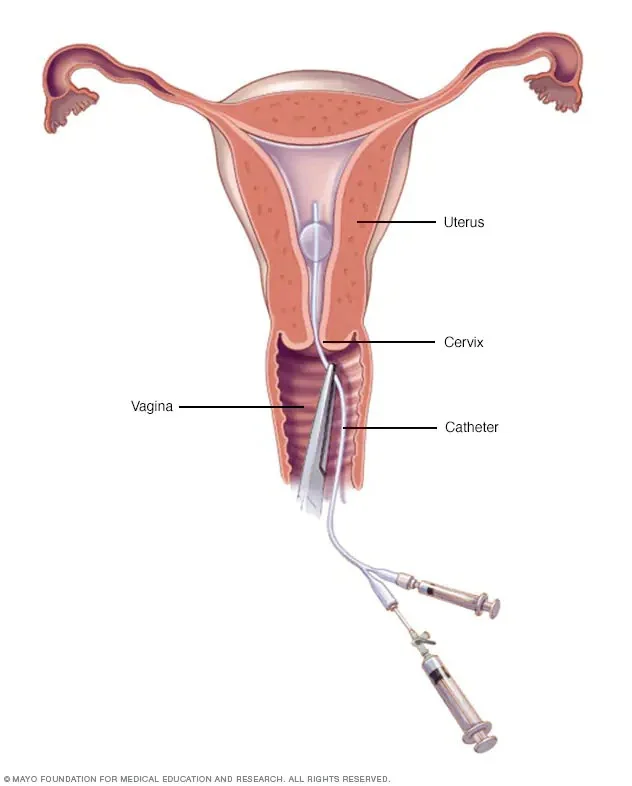
Hysterosalpingography (HSG)
Application of contrast agent into the uterine cavity:
-
Indications :
- infertility to assess :
- uterine morphology
- tubal patency.
- infertility to assess :
-
Contraindications :
- Inflammation (active pelvic infection).
- ✓ Tumor
- ✓ Pregnancy
- ✓ Menses
- ✓ recent uterine or tubal surgery
- ✓
- Inflammation (active pelvic infection).
Technique
- performed during proliferative phase
- the menstrual cycle (days 6-12)
- …when the endometrium is at its thinnest
- patient in the lithotomy position
- Vaginal speculum is inserted with the cervix in view
- the cervix is cleaned with an aseptic solution
- catheterization of the cervix.
- Inject contrast.
Technique
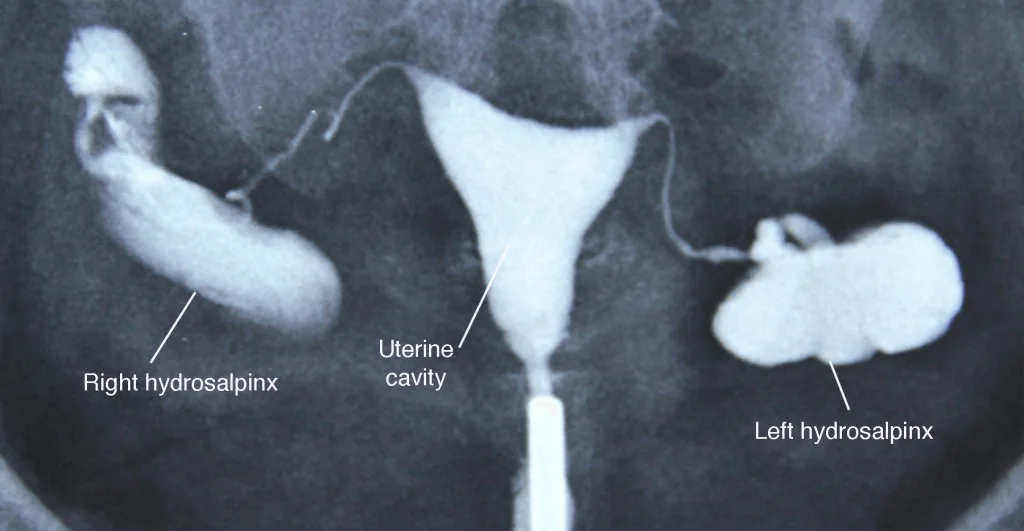
The image contains three X-ray images with labels and annotations.
- The top-left image is labeled with the following text:
- Right hydrosalpinx
- Uterine cavity
- Left hydrosalpinx
Complications
- Common but self-limiting ✓ abdominal cramping ✓ spotting ✓ venous extravasation
- Rare but serious ✓ pelvic infection ✓ contrast reaction
Angiography
- Angiograms can help in detecting blood vessel abnormalities.
- Rarely indicated:
- pathologic vascularization
- Involvement of pelvic vessel

Potential Risks and Complications
- Heart attack.
- Stroke.
- Injury to the catheterized artery.
- Arrhythmias.
- Allergic to the dye or medications.
- Renal damage.
- Infection.
Cystourethrogram
- Dynamic test used to Demonstrate:
- the lower urinary tract
- Vesico-ureteral reflux.
- bladder pathology
- Congenital anomalies of bladder.
Indications
- Children:
- Urinary tract infection
- voiding difficulties.
- Baseline study prior to lower UT surgery.
- Urinary tract infection
- Adults:
- Trauma to urethra.
- urethral stricture.
- urethral diverticula.
- UTI.
- Reflux nephropathy prior to renal transplant of kidneys.
- Trauma to urethra.
Complications
- UTI.
- Adverse reactions from contrast.
- Trauma causing dysuria, frequency Hematuria and urinary retention.
- perforation.
- Catheterization of vagina or ectopic ureteral orifice.
- Exposes gonads to some radiation.
Ultrasonography
- Ultrasound is not substituting good history & a thorough examination.
- Always do an abdominal scan before using the vaginal probe.

Role of Ultrasound
- To examine the uterus, ovaries, cervix, vagina and adnexae.
- Classification of a mass identified on other modalities eg:
- solid.
- cystic.
- mixed.
Indications
- Vaginal bleeding.
- vaginal discharge.
- Menorrhagia.
- Metrorrhagia (irregular uterine bleeding).
- Amenorrhea.
Limitations
- Transvaginal scanning is contra-indicated:
- if the patient is not yet sexually active.
- or cannot provide informed consent.
Patient Preparation
- Scan the patient in the first 10 days of the cycle.
- Full bladder is required .(Abdominal US) Instruct the patient to drink 1 Litre of water.
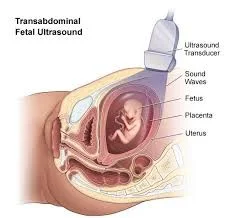
Scanning Technique

Transabdominal
- Full bladder
- Panoramic view
For :
- large masses
- Abdominal organs
- Lymph nodes

Transabdominal Approach
This is a generalised overview to identify the cervix, uterus and ovaries.
- Check for the orientation the uterus (anteverted V’s retroverted)
- Assess the uterine size and shape.
Transvaginal Ultrasound
- Before inserting the probe
- show the patient the TV probe and explain the procedure.

What to Detect in Gynaecology Ultrasound
Vaginal
- Vaginal carcinoma
- Haematocolpos (secondary to imperforate hymen or vaginal stenosis)
- Foreign body
Cervical
- Nabothian (retention) cysts
- Polyps
- Cervical fibroids
Uterine
- Fibroids (leiomyoma)
- submucosal
- intramural
Endometrial
- Endometrial Polyps.
- Endometrial Carcinoma.
- Endometrial hyperplasia.
Ovarian
- Ovarian cysts
- simple complex (haemorrhagic, corpus luteal, ruptured, septated).
- Dermoid cyst.
Pouch of Douglas
- Fluid
- Pus
- Blood
Fallopian Tubes
- Normal fallopian tubes not seen, in a routine scan. Pathological tubes seen as dilated, truncated structures.
- PID.
- Pyosalynx.
A Pelvic Series Should Include
- Uterus - longitudinal, transverse (with measurements)
- Endometrial thickness measured in the longitudinal plane
- Cervix
- Both ovaries- longitudinal, transverse
Obstetric Ultrasound
Ultrasonography
- Method of the first choice
- Recognition of multiple pregnancy
- vitality
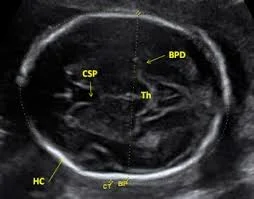
2nd and 3rd Trimester
- ✔ 3-5 week - gestational
- ✔ 6. - 7. week - heart
- Fetal biometry
Dead Fetus
- Absence of flow and heart movements
- Oligohydramnios
- Superposition of skull bones
Spalding sign

3D Ultrasound
- most frequently used in ob
- Commercial use

MRI
- congenital disorders (in case of unclear US finding)
- examination of mother (instead of X-ray or CT)
Plain Film
- Dead fetus
- Distortion of vertebral column
- Superposition of skull bones


Thank You
Questions

