Functions of Bone Tissue
Mechanical Functions
- Give shape to the body
- Load transmission
- Mediate movement
- Support & protect soft tissue
Mineral Reservoir
- Largest reservoir of
- Regulation of
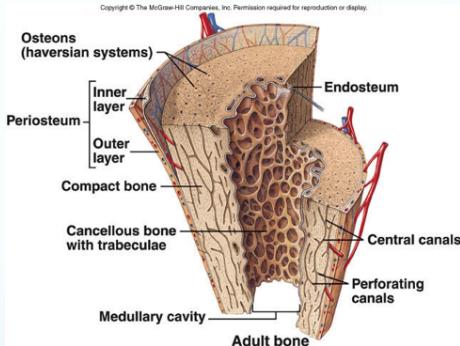
Bone Components
A: Matrix
- Organic (40% of dry weight):
- Collagen fibers
- Inorganic (Minerals) (60%):
- Ca++ hydroxyapatite, Ca++ phosphate
B: Cells
- Osteoblasts: bone-forming cells (hyperactivation produces tumors)
- Osteoclasts: bone-resorbing cells (hyperactivation produces osteoporosis)
- Osteocytes: normal mature bone cells
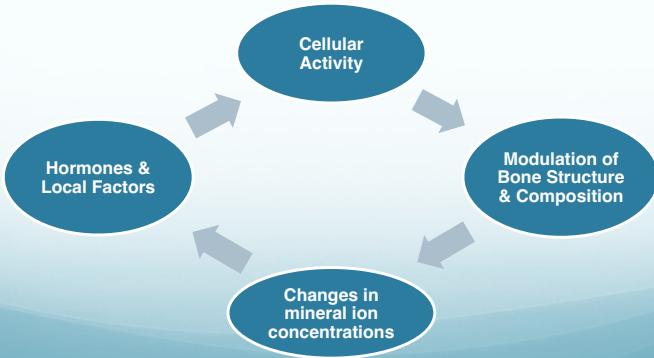
Bone is Active
- Continuous activity & flow
- Structure & composition changing all the time
- Regulation by cellular activity:
- Osteoclasts & Osteoblasts
Diagram: Regulation of Bone Activity
The diagram shows a cyclical relationship between:
- Cellular Activity
- Modulation of Bone Structure & Composition
- Changes in mineral ion concentrations
- Hormones & Local Factors
Bone Growth & Remodeling
Growth Processes
- Epiphyseal growth: Endochondral ossification
- Surface growth: Appositional ossification
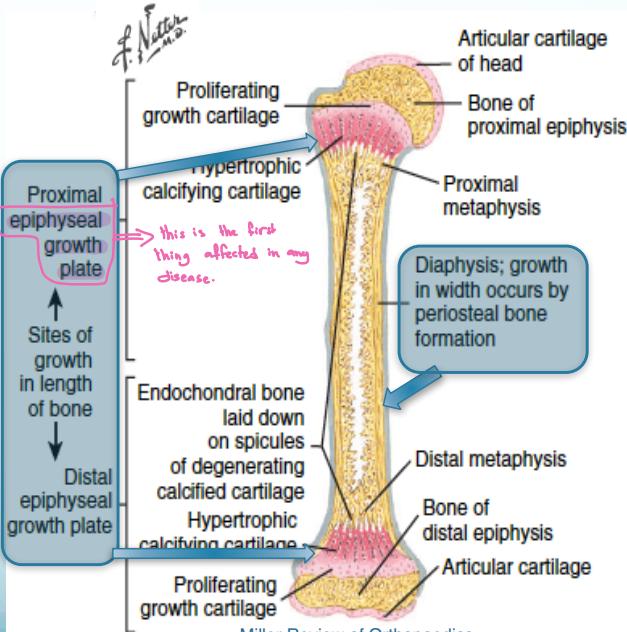
Adult Remodeling
- Continuous remodeling of existing bone (no growth)
- “Old bone” continuously replaced by “new bone”
- Annual turnover rates:
- 4% of cortical bone
- 25% of cancellous bone
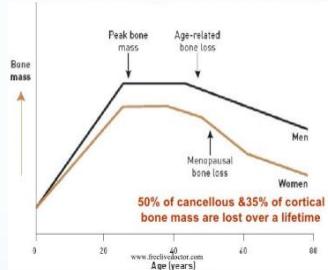
- Age-related changes:
- Initially: formation slightly exceeds resorption
- Later: resorption exceeds formation → Bone mass steadily declines
Age-Related Bone Changes
Childhood – Adolescence
- Growth phase (↑ size & change shape)
Adolescence – 35 years
- Bones get heavier and stronger
- Annual bone mass gain: 3%
35 – 50 years
- Slow loss of bone mass annually:
- Men: 0.3% annually
- Women:
- 0.5% annually to menopause
- Then 3% annually for 10 years (due to ↑ osteoclastic activity from ↓ estrogen hormones)
65 years – onwards
- Loss of mass slows gradually to 0.5% (↓ osteoblastic activity)
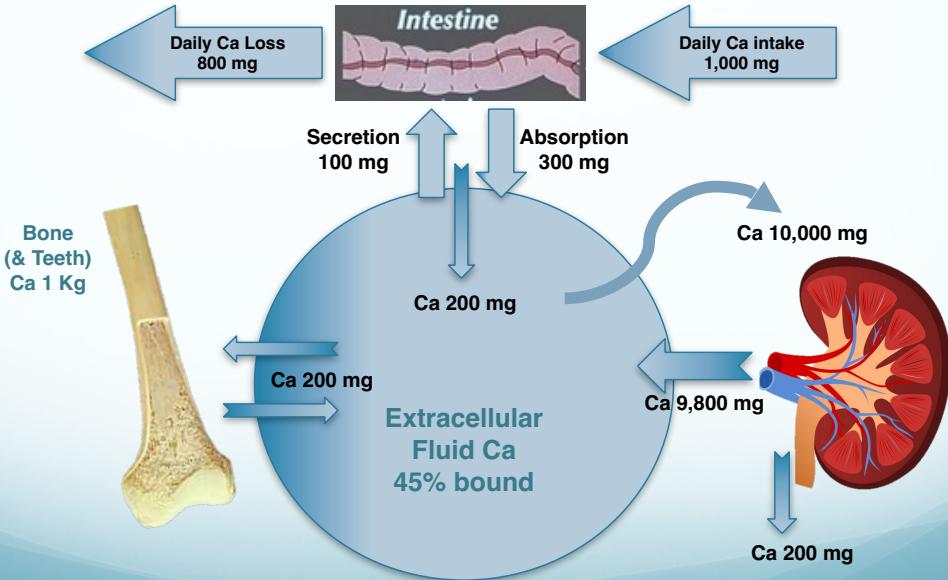
Body Calcium
- Most calcium in the body is present in bone
- Calcium release from bone is a slow process
- Serum calcium is essential for:
- Cell function
- Nerve conduction
- Muscle contraction
- Normal level: 8.8-10.4 mg/dl (2.2-2.6 mmol/L)
- Serum calcium levels must be controlled continuously and promptly through:
- Renal reabsorption
- Bone resorption
- Intestinal absorption
Causes of ↓ Calcium Absorption
- ↑ intake of phosphates (as in soft drinks)
- ↑ intake of oxalates (as in tea and coffee)
- Drugs: corticosteroids
- Intestinal mal-absorption syndromes
Players in Calcium Regulation
Primary Regulators
- Vitamin D: The general crude regulator
- Target organs:
- Small intestines (↑ absorption of Ca, Mg, )
- Bones (↑ mineralization)
- Target organs:
- PTH (Parathyroid Hormone): The sensitive fine regulator
- Target organs:
- Kidneys (quick): ↑ reabsorption of Ca, ↓ reabsorption of , converts Vit D2 to D3
- Bones (slow): through Vitamin D
- Small intestine: indirectly through Vitamin D
- Target organs:
- Calcitonin: From C cells of Thyroid
- Opposite to PTH on bone and kidneys
- Protective effect: ↓ osteoclast activity, ↓ kidney reabsorption of Ca, ↓ serum Ca
Secondary Modulators
- Estrogen:
- Protects bone from PTH effects
- In Menopause: osteoclasts become more active
- Corticosteroids (Bad to bone): from supra-renal gland
- ↓ osteoblastic activity, ↑ osteoclastic activity
- ↓ calcium absorption from intestine
- ↑ renal excretion of calcium
- Local factors – BMP (Bone Morphogenic Proteins)
- Mechanical stress:
- Strengthens bone
Normal Calcium & Phosphate Metabolism
Organ Systems Involved
- Intestine
- Kidney
- Bone
Metabolic Pathway
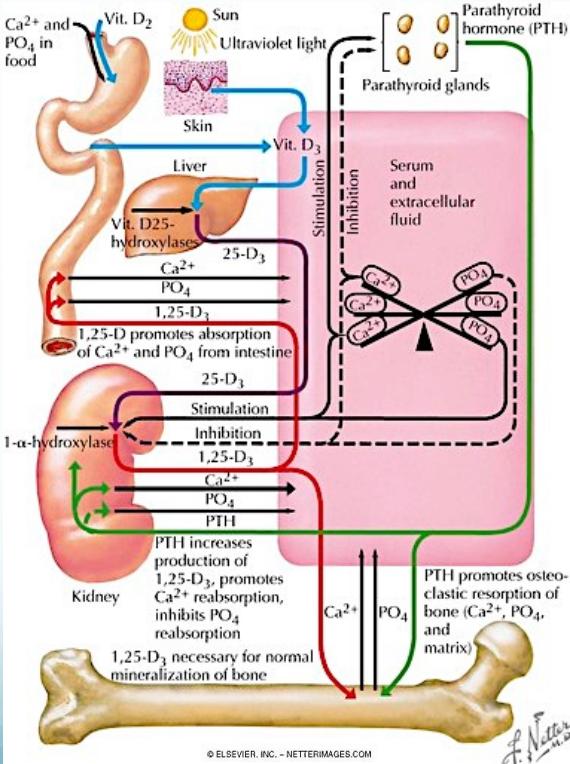
Calcium Metabolism
Calcium Metabolism Diagram