CDH - CTEV

Prof. Mamoun Kremli Dr. Tarif Alakhras

Nomenclature
- CDH: Congenital Dislocation of the Hip
- DDH: Developmental Dysplasia of the Hip
- X - other ab CHD: (Congenital Heart Disease)*
Spectrum of Disease
- Different etiologies, pathologies, and natural history
- Affects proximal femur and acetabulum
- Initial pathology is congenital, but progresses if untreated
- Does not always result in dislocation
Classification of CDH
- Teratologic hip: Fixed dislocation at birth, often with other major anomalies
- Dislocated hip: May or may not be reducible
- Unstable hip: Dislocatable and reducible
- Acetabular dysplasia: Shallow acetabulum
Incidence
- Hip instability at birth: 0.5 – 1%
- Classic CDH: 0.1%
- Mild dysplasia: Substantial (up to 50% of hip arthritis in women have underlying hip dysplasia)
Etiology
Multi-factorial condition with several contributing factors:
Ligamentous and Hormonal Factors
- Ligament laxity
- Hormonal influences:
- Estrogen and Relaxin from mothers
- May affect baby girls more due to receptor differences
- Familial (congenital):
- Mild to severe forms including Ehler-Danlos syndrome

Genetic Factors
- Gender predisposition: Females 4-6 times more affected than males
- Twin studies:
- If one twin has DDH, incidence in second twin:
- Monozygotic: 38%
- Dizygotic: 3% (similar to other siblings)
- If one twin has DDH, incidence in second twin:
Mechanical Factors
- Prenatal factors:
- Breech position: Normally 2-4%, in CDH: 16%
- Oligohydramnios, primigravida
- Associated with torticollis and metatarsus adductus
- Postnatal factors:
- Swaddling/strapping hips in adducted and extended position with knees extended


Risk Factors
High-Risk Infants
- Positive family history: 10× increased risk
- Female gender: 4-6× increased risk
- Breech presentation: 5-10× increased risk
- Torticollis: CDH present in 10-20% of cases
- Foot deformities:
- Calcaneo-valgus
- Metatarsus adductus
- Knee deformities:
- Hyperextension and dislocation (Teratologic)
Management of High-Risk Infants
When risk factors are present:
- The infant should be examined repeatedly
- The hips should be imaged (Ultrasound or X-ray)
Clinical Examination
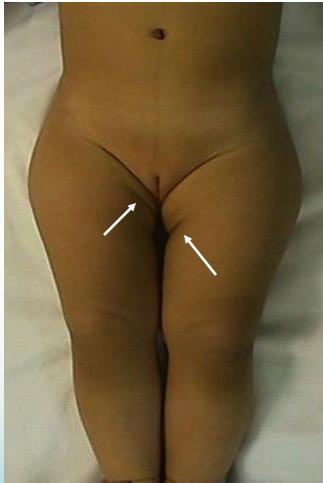
Inspection (Look)
- General appearance:
- Externally rotated hip
- Lateralized contour
- Wide perineum (in bilateral cases)
- Asymmetrical skin folds (anterior and posterior)



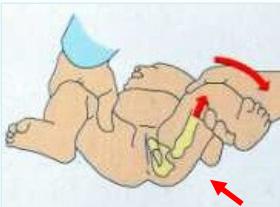
Physical Measurements
- Shortening assessment:
- Supine position
- Galeazzi test (Allis sign)


Range of Motion (Move)
- Abduction limitation in flexion:
- Careful assessment in bilateral cases
- Symmetrical limitation may indicate bilateral involvement
- If abduction < 60° bilaterally: considered abnormal

Special Tests
- Galeazzi test and limited abduction in flexion
- Note: Use of a lollipop can help during examination


Neonatal Special Tests
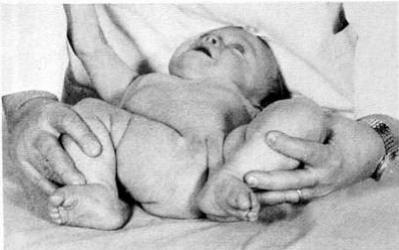
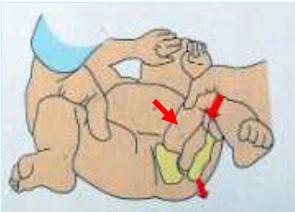
Ortolani Test
- Purpose: Reduces a dislocated hip
- Technique:
- Feel a clunk (positive sign)
- Do not rely on hearing a click (can be misleading)
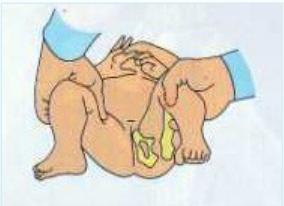

Barlow Test
- Purpose: Dislocates a reduced hip
- Technique:
- Feel a clunk (positive sign)
- Do not rely on hearing a click (can be misleading)



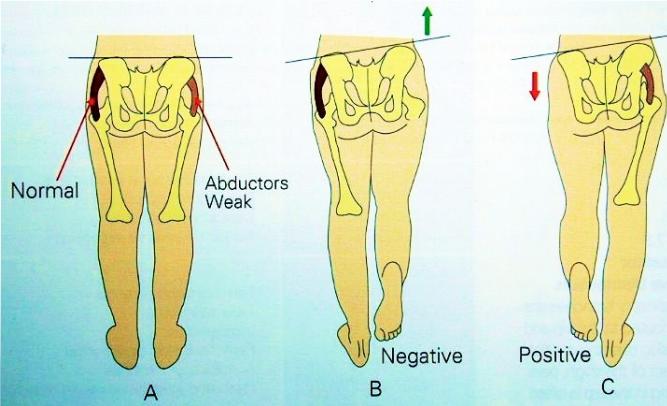
Trendelenburg Test
- Unilateral cases: Trendelenburg gait
- Bilateral cases: Waddling gait
Age-Specific Examination Findings
- Neonatal: Limited abduction, positive Ortolani/Barlow tests
- Toddler: Shortening, limited abduction
- Walking age: Shortening, limited abduction, positive Trendelenburg sign
Imaging
Ultrasound
- Early infancy: More reliable than X-ray
- Expert interpretation required for accurate results
- Timing considerations:
- Incidence of hip stability declines rapidly to 50% within first week of neonatal life
- Better to delay ultrasound until after 2 weeks of age
Radiology (X-ray)
Early Infancy
- Not reliable in early infancy - ultrasound is preferred

After 3 Months
- More reliable for assessment
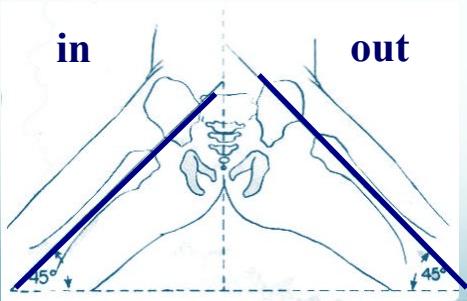
- AP abduction view:
- Long axis of femur normally passes through acetabulum
After 6 Months
- Clearly shows dislocation
- Femoral head ossific center size and position assessment

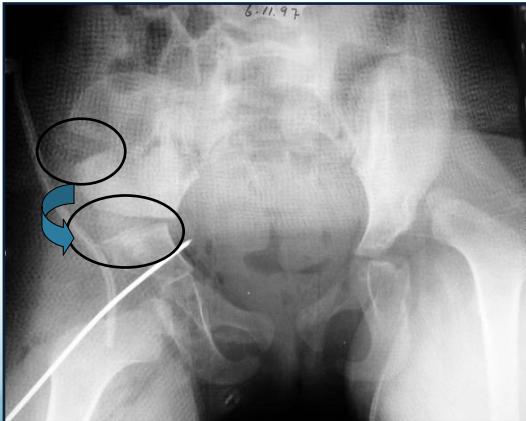
Radiological Assessment Methods
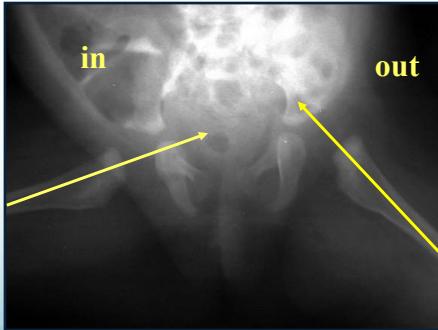
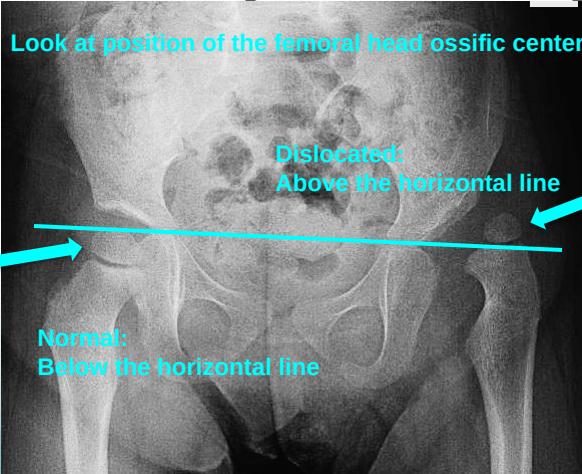
1. Horizontal Line Through Tri-radiate Cartilage
- Normal: Femoral head ossific center below the horizontal line
- Dislocated: Femoral head ossific center above the horizontal line
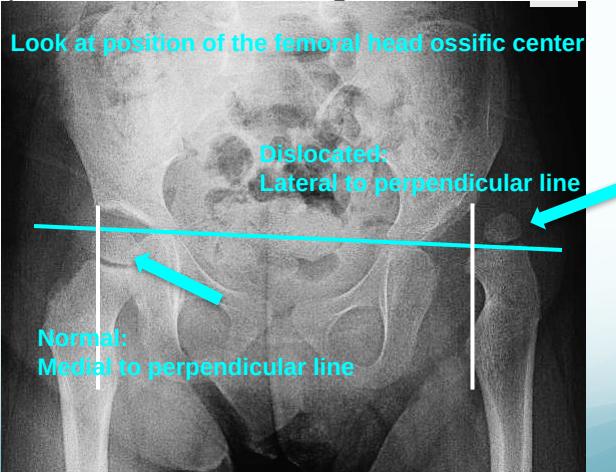
2. Perpendicular Line from Acetabular Edge
- Normal: Femoral head ossific center medial to perpendicular line
- Dislocated: Femoral head ossific center lateral to perpendicular line
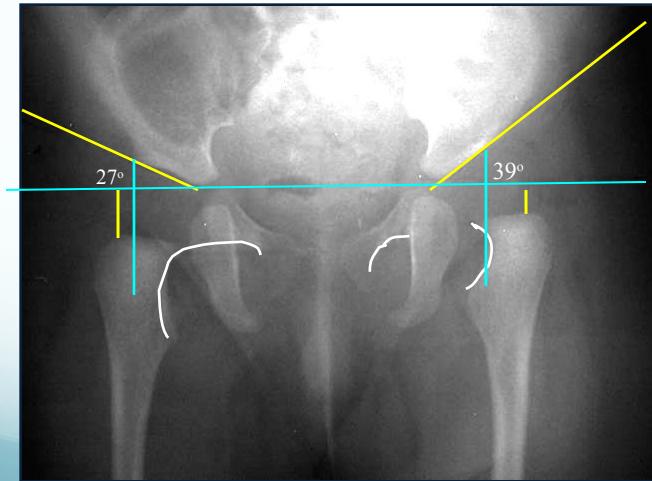
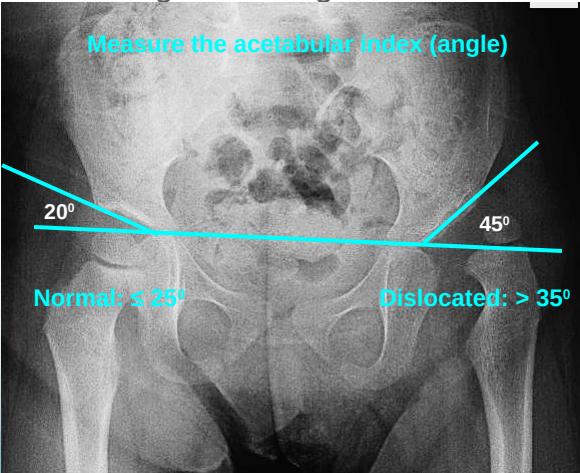
3. Acetabular Index (Acetabular Angle)
- Measurement: Angle from acetabular edge to base at horizontal line
- Normal: ≤ 25°
- Dislocated: > 35°
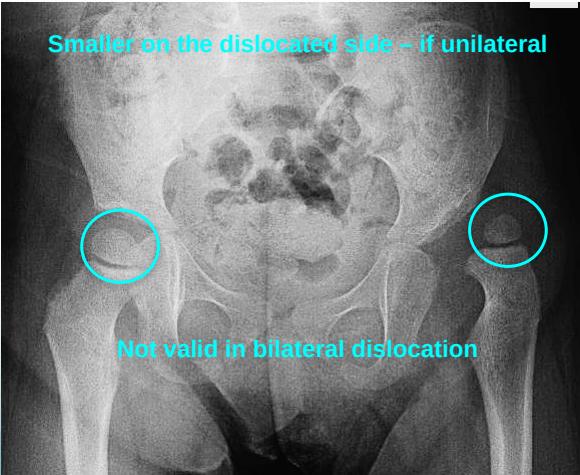
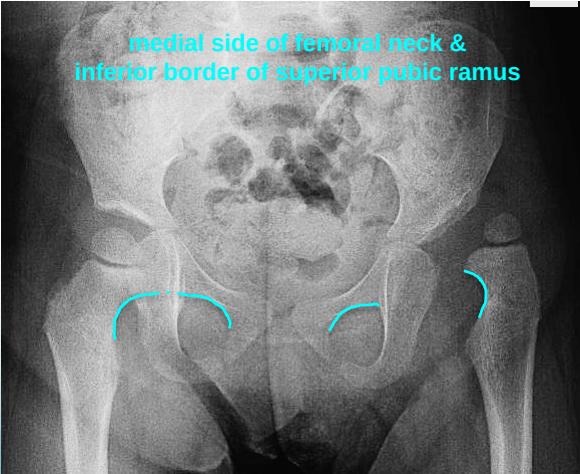
4. Shenton’s Line
- Important assessment tool for hip joint integrity
Treatment
Treatment Goals
- Obtain concentric reduction of the hip
- Non-traumatic approach to preserve blood supply to femoral head
- Early detection and intervention for optimal outcomes
Key Principles
- Method depends on age at presentation
- Earlier treatment = easier management and better results
- Early detection is critical for successful outcomes
Age-Specific Treatment Protocols
Neonatal Hip Instancy (Birth to 6 months)
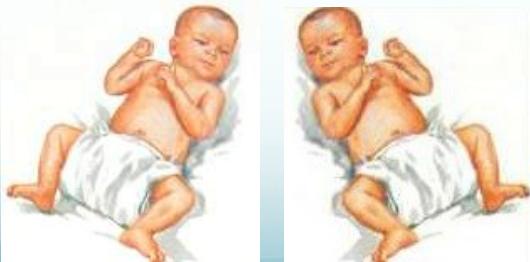
- Initial observation (most resolve spontaneously):
- Avoid adduction swaddling
- Apply double diapers
- Re-evaluate at 2 weeks of age
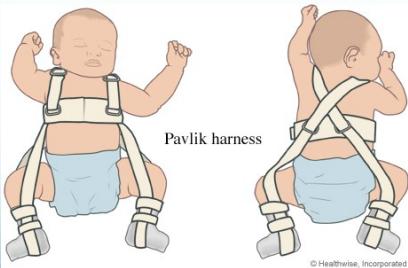
- If unstable at 2 weeks: Pavlik Harness
- Dynamic, effective, and safe treatment option

6-12 Months of Age
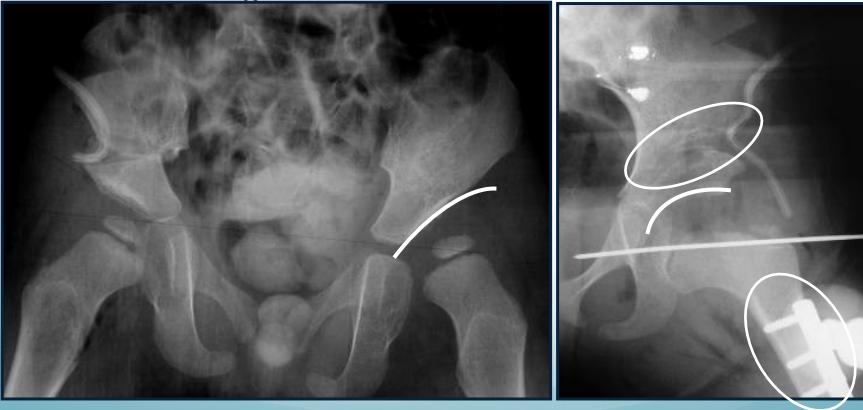
- Closed reduction with hip spica cast
- Open reduction (surgery) with hip spica cast
- Arthrography-guided procedures


18-24 Months of Age
- Surgical intervention: Open reduction with possible acetabuloplasty
Above 2 Years of Age
- Comprehensive surgical approach:
- Open reduction
- Acetabuloplasty
- Femoral shortening
Complete Treatment Algorithm
| Age Range | Primary Treatment |
|---|---|
| Birth - 6 months | Pavlik harness or hip spica |
| 6-12 months | Closed reduction under GA and hip spica (Note: some approaches avoid this) |
| 12-18 months | Open reduction |
| 18-24 months | Open reduction and acetabuloplasty |
| 2-8 years | Open reduction, acetabuloplasty, and femoral shortening |
| Above 8 years | Open reduction, acetabuloplasty (all three pelvic bones), and femoral shortening |
CDH Summary
- Complex multi-factorial, endemic disease
- Identify at-risk groups for early screening
- Learn proper examination methods for accurate diagnosis
- Early treatment is easier and yields better results