Classification Systems
Anatomical Classification
-
Tetraplegia: Injury to the cervical spinal cord leading to impairment of function in arms, trunk, legs, and pelvic organs
-
Paraplegia: Injury to the thoracic, lumbar, or sacral segments leading to impairment of function in trunk, legs, and pelvic organs (arm function preserved)
ASIA Impairment Scale Y
| Grade | Description | Classification |
|---|---|---|
| A | No motor or sensory function preserved in sacral segments S4-S5 | Complete |
| B | Sensory function preserved, but motor function not preserved below neurological level including S4-S5 | Incomplete |
| C | Motor function preserved below neurological level, and more than half of key muscles below neurological level have muscle grade < 3 | Incomplete |
| D | Motor function preserved below neurological level, and at least half of key muscles below neurological level have muscle grade ≥ 3 | Incomplete |
| E | Motor and sensory functions are normal | Normal |
Types of Shock
| Feature | Spinal Shock | Neurogenic Shock | Hypovolemic Shock |
|---|---|---|---|
| BP | Hypotension | Hypotension | Hypotension |
| Pulse | Bradycardia | Bradycardia | Tachycardia - compensatory mechanism |
| Reflexes | Absent | Variable/Independent | Variable/Independent |
| Motor | Flaccid paralysis | Variable/Independent | Variable/Independent |
| Time | ~48-72 hours after SCI | ~48-72 hours after SCI | Following excessive blood loss |
| Mechanism | Peripheral neurons become temporarily unresponsive to brain stimuli | Disruption of autonomic pathway leads to loss of sympathetic tone and decreased systemic vascular resistance | Decreased preload leads to decreased cardiac output |
Complete injury
an injury with no spared motor or sensory function below the affected level • Classified as ASIA A
Incomplete injury
- an injury with some preserved motor or sensory function below the injury level
- Incomplete spinal cord injuries:
- anterior cord syndrome
- Brown-Sequard syndrome
- central cord syndrome
- posterior cord syndrome
- conus medullaris syndrome
- cauda equina syndrome
Incomplete Cord Syndromes
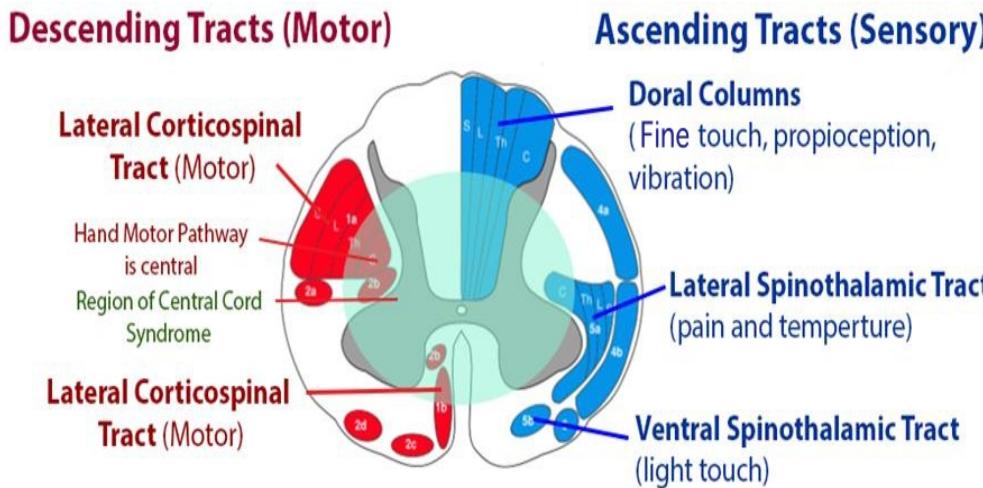
Central Cord Syndrome
- Most common incomplete cord injury
- Often in elderly with minor extension injury mechanisms
- Pathophysiology: Hands and upper extremities located “centrally” in corticospinal tract
Clinical Presentation:
- Weakness with hand dexterity impairment
- Hyperpathia
- Motor deficit worse in UE than LE (some preserved motor function)
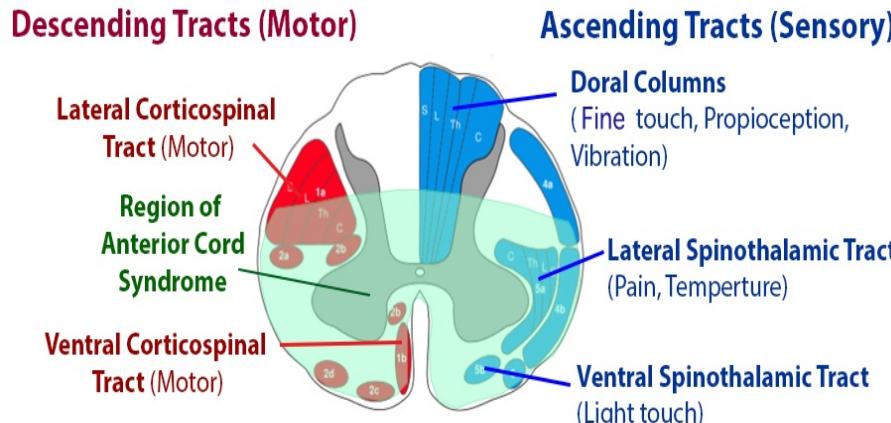
Anterior Cord Syndrome
- Worst prognosis of incomplete SCI
- Causes: Direct compression (osseous) of anterior spinal cord or anterior spinal artery injury
- Key feature: Lower extremities affected more than upper extremities
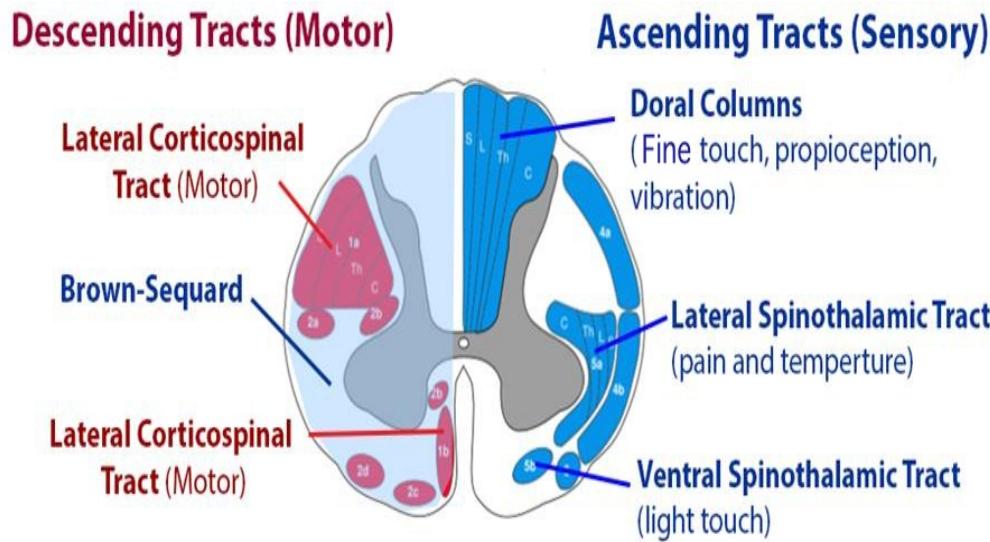
Brown-Sequard Syndrome
- Excellent prognosis
- Cause: Complete cord hemitranssection, usually seen with penetrating trauma
Clinical Features:
- Ipsilateral deficit: LCTL motor function, DC: proprioception, vibratory sense
- Contralateral deficit: LST: pain, temperature
Other Incomplete Syndromes
- Posterior cord syndrome
- Conus medullaris syndrome
- Cauda equina syndrome
Special Conditions
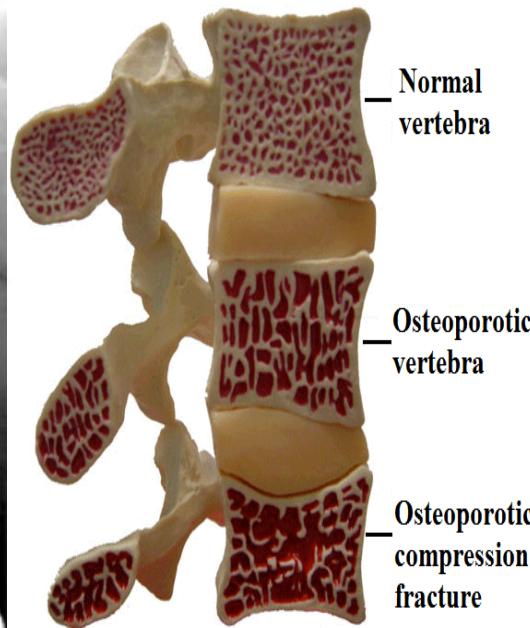
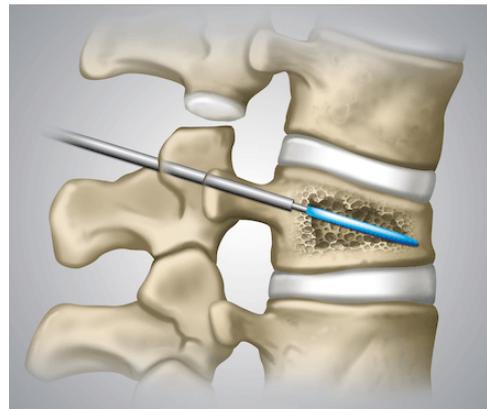
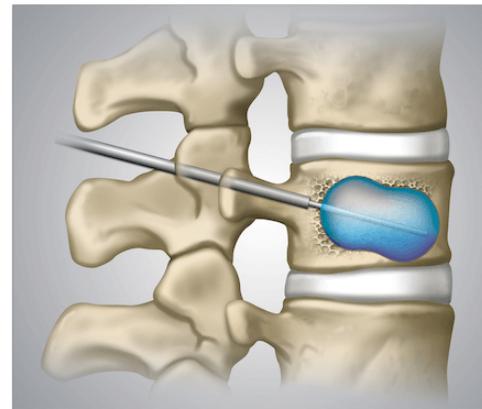
Osteoporotic Vertebral Compression Fracture
- Commonest vertebral injury
- Etiology: Minor trauma in osteoporotic people
- Prevalence: Affects up to 50% of people over 80 years old
- Diagnosis: Lateral radiographs
- Initial treatment: Observation and pain management
- Kyphoplasty: Reserved for patients with recalcitrant symptoms after 4-6 weeks of nonoperative treatment

Cauda Equina Syndrome Z
- Etiology: Severe compression of nerve roots in the thecal sac of lumbar spine, most commonly due to acute lumbar disc herniation
- Critical: Early diagnosis is essential
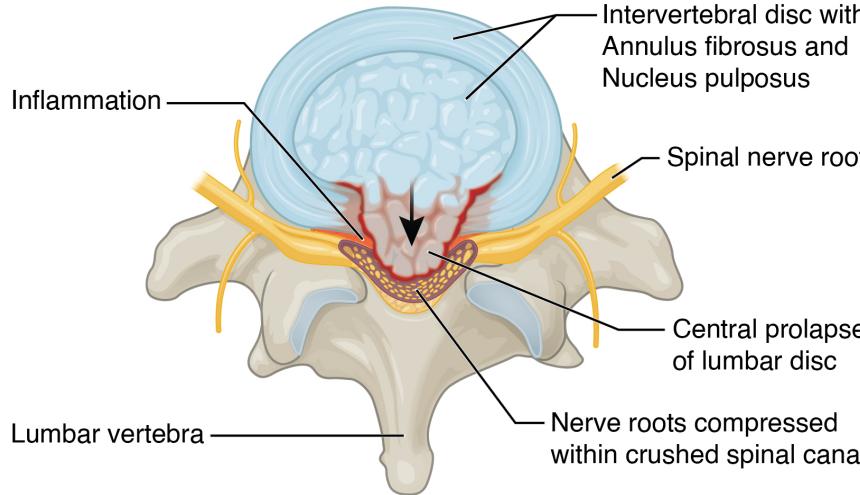
Clinical Features:
- Back pain (most common)
- Unilateral or bilateral leg pain (2nd most common)
- Saddle anesthesia (highly specific)
- Bladder dysfunction: Urinary retention → overflow incontinence
- Unilateral or bilateral sensory changes in legs
- Unilateral or bilateral motor weakness in legs
Diagnosis:
- Urgent MRI to confirm cause

Treatment:
- Prompt surgical decompression
- Should be performed within 24 hours, absolutely within 48 hours
Common Spinal Disorders
Degenerative Conditions
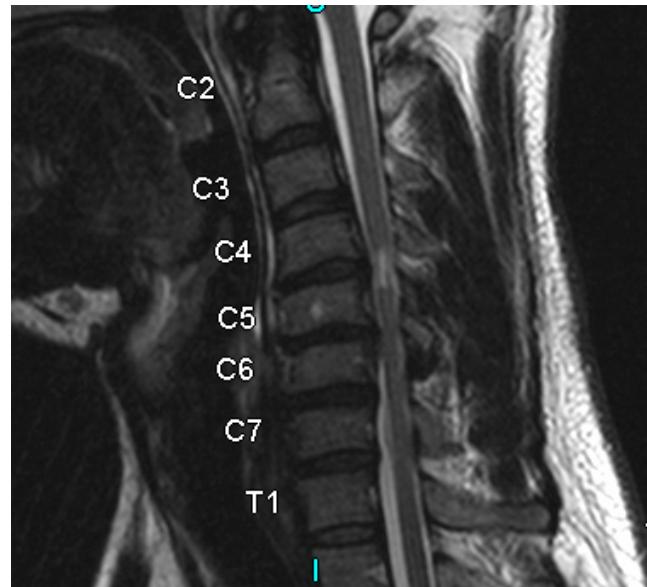
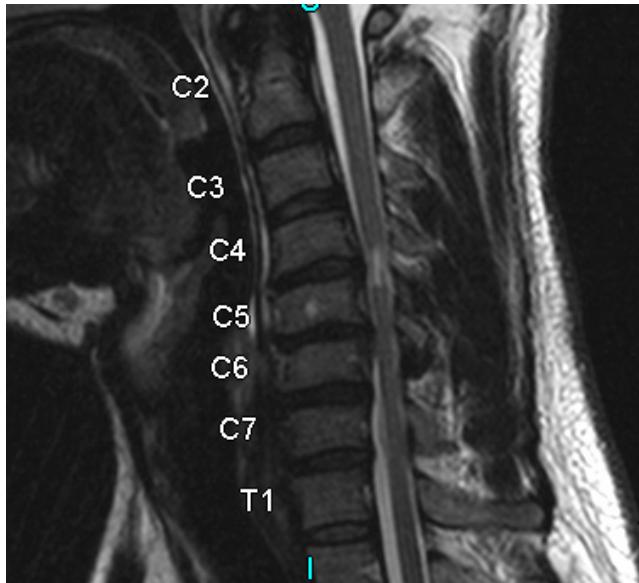
Cervical Spondylosis
- Pathophysiology: Natural aging and degenerative process of cervical motion segment
- Age of onset: Typically begins at age 40-50; 85% of patients >65 years
- Presentation: Can lead to cervical radiculopathy, cervical myelopathy, or axial neck pain
- Diagnosis: Plain radiographs of cervical spine
- Treatment: Observation, medical management, or surgical management depending on severity and chronicity of pain, presence of instability, or neurological deficits

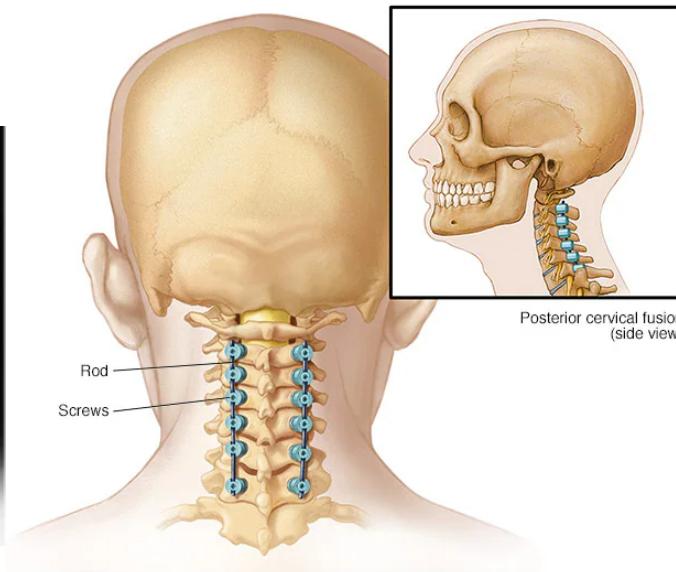
Cervical Myelopathy Z
- Definition: Common form of neurologic impairment caused by compression of cervical spinal cord, most commonly due to degenerative cervical spondylosis
- Typical presentation: Older patients with symmetric numbness and tingling in extremities, hand clumsiness, and gait imbalance
- Treatment: Usually surgical decompression and stabilization as condition is associated with step-wise progression
Clinical Presentation:
- Neck pain and stiffness
- Extremity paresthesias: diffuse, bilateral, nondermatomal numbness and tingling
- Weakness and clumsiness: bilateral weakness and decreased manual dexterity (dropping objects, difficulty manipulating fine objects)
- Gait instability: Most important clinical predictor
- Urinary retention
Physical Examination:
- Upper motor neuron signs (spasticity):
- Hyperreflexia
- Hoffmann’s sign: Snapping patient’s distal phalanx of middle finger leads to spontaneous flexion of other fingers (most common physical exam finding)
- Sustained clonus: > three beats defined as sustained clonus
- Babinski test: Positive with extension of great toe
Imaging:
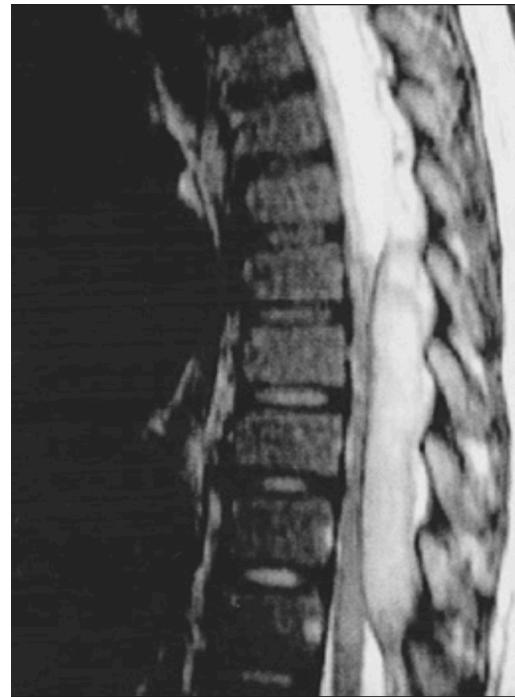
- MRI: Study of choice to evaluate degree of spinal cord and nerve root compression
Management:
- Observation
- Symptomatic treatment
- Surgery (decompression and fusion)

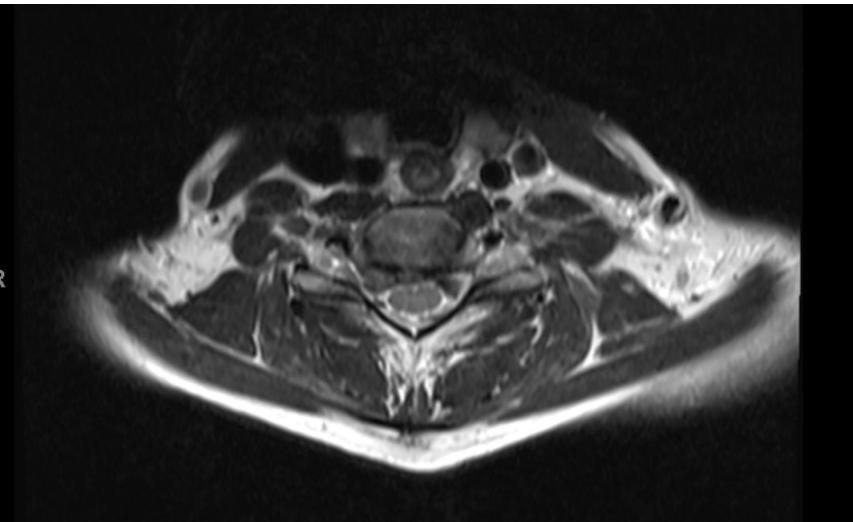
Cervical Radiculopathy
- Definition: Clinical condition characterized by unilateral arm pain, numbness and tingling in dermatomal distribution in hand, and weakness in specific muscle groups
- Evaluation: Thorough neurologic examination, cervical spine radiographs including flexion-extension views, and MRI of cervical spine
- Treatment: Nonoperative treatment successful in 75%-90% of patients; surgical decompression reserved for refractory cases or patients with progressive neurologic deficits
Imaging Examples:

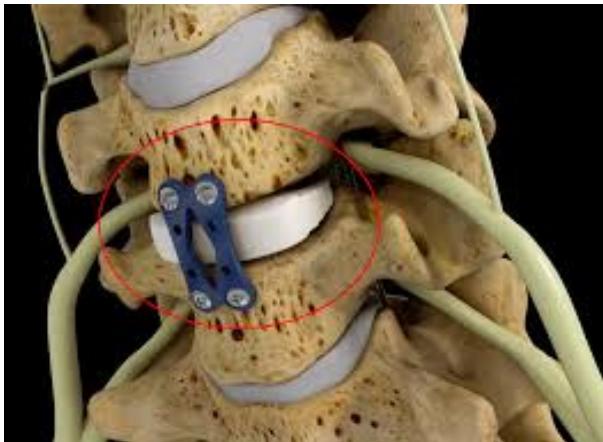
Surgical Treatment - Anterior Cervical Discectomy and Fusion:

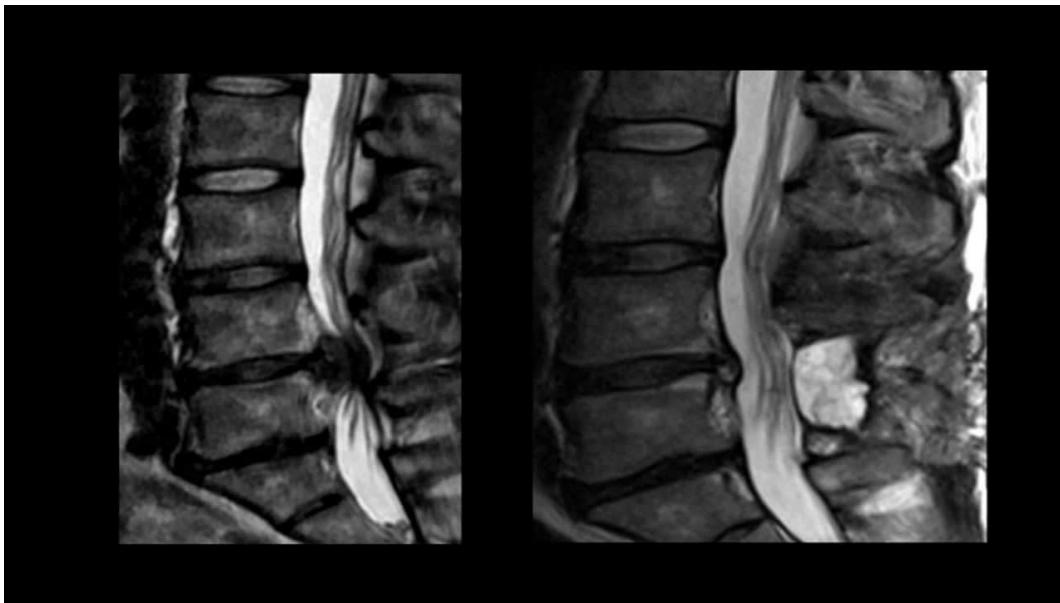
Lumbar Disc Herniation
- Significance: Very common cause of low back pain and unilateral leg pain (radiculopathy)
- Diagnosis: Made clinically and confirmed with MRI studies of lumbar spine
- Initial treatment: Nonoperative with oral medications and physical therapy for radicular leg pain
- Surgical indication: Microdiscectomy for severe pain and/or motor deficit that have failed to respond to nonoperative management
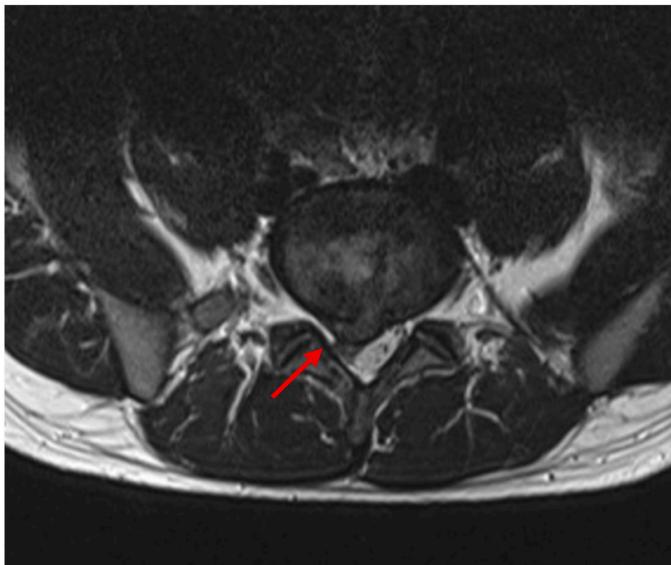
L5/S1 Disc Herniation Example:

Degenerative Spondylolisthesis
- Definition: Common degenerative condition characterized by subluxation of one vertebral body anterior to the adjacent inferior vertebral body with intact pars
- Demographics: Most common in females over 40 years of age, at the L4-5 level
- Diagnosis: Lateral radiographs; flexion and extension lateral lumbar radiographs can identify degree of instability
- MRI: Helpful for central or foraminal stenosis





Treatment:
- Nonoperative: Trial with NSAIDs and physical therapy
- Surgical: Indicated for progressive disabling pain that has failed nonoperative management, and/or progressive neurological deficits
Scoliosis
Deformities
Scoliosis Classification
- Adolescent Idiopathic Scoliosis
- Infantile Idiopathic Scoliosis
- Congenital Scoliosis
- Neuromuscular Scoliosis: Irregular spinal curvature caused by disorders of brain, spinal cord, and muscular system
Adolescent Idiopathic Scoliosis
- Definition: Coronal plane spinal deformity most commonly presenting in adolescent girls from ages 10 to 18
History Assessment:
- Who noticed it? Family history?
- When was it noticed?
- Pre-natal, post-natal history?
- Pubertal status?
- Pain presence?
- Previous treatment?
Physical Examination:
- Leg length inequality
- Midline skin defects (hairy patches, dimples, nevi)
- Signs of spinal dysraphism
- Shoulder height differences
- Truncal shift
- Rib rotational deformity (rib prominence)
- Waist asymmetry and pelvic tilt
- Café-au-lait spots (neurofibromatosis)
- Foot deformities (cavovarus)
Adams Forward Bending Test:
 - Normal spine
- Normal spine
 - Scoliosis deformity
- Scoliosis deformity
- Adams test
Imaging:

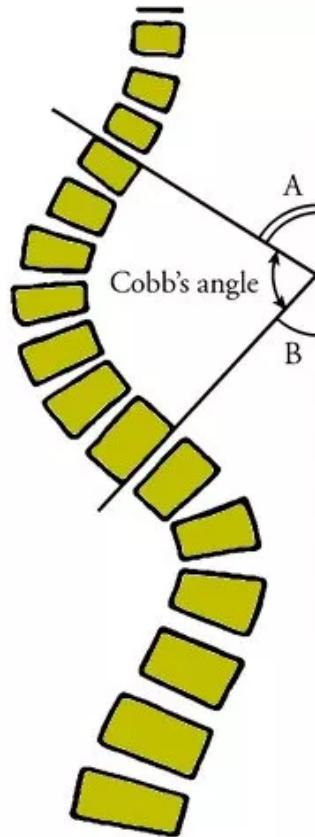
Severity Grades:
- Mild: 10-25°
- Moderate: 25-45°
- Severe: >45°
Treatment Based on Severity:
- Observation: Mild curves, depending on age and skeletal maturity
- Bracing: Moderate curves (25-45°) in growing patients

- Surgery: Severe curves (>45°) or progressive curves


Infantile Idiopathic Scoliosis
- Definition: Coronal plane spinal deformity presenting in children ages 3 years or less
- Characteristics: Usually normal kids with no other pathologies

Congenital Scoliosis
- Definition: Congenital spinal deformity occurring due to failure of normal vertebral development during 4th to 6th week of gestation
- Association: Usually patients have other congenital pathologies

Infections
Spinal Epidural Abscess
- Definition: Spinal infection caused by collection of pus or inflammatory granulation tissue between dura mater and surrounding adipose tissue
- Presentation: Pain (87% of cases), often severe and insidious in onset; Neurologic deficits present in ~33%
- Diagnosis: MRI studies with contrast
- Treatment: Prompt surgical decompression and long-term IV antibiotics
Risk Factors:
- IV drug abuse
- Immunodeficiency
- Malignancy
- HIV infection
Microbiology:
- Staphylococcus aureus is most common organism