History Taking in MSK Trauma
Overview
Prof. Mamoun Kremli
Dr. Tarif Al Akhras
History Taking
Key Components
- Patient’s story / or companion’s
- Doctor/student reconstructs the history
- Open-ended questions
- How did it happen?
- Leading questions
- Were you able to stand/walk after the injury?
- What increases the pain?
- Did you vomit?
- Open-ended questions
History Structure
Following the History Theme
- Patient Demographic
- Chief Complaint
- History of Presenting Complaint
- Past medical/surgical history
- Medication/allergy history
- Family history
- Social history
- Diet
- Activity
- Systemic review Relate to function
Trauma History
Detailed History of Injury
-
Details of injury:
- Mechanism of injury. High Vs. Low velocity Open Vs. Closed
- Date, time, type, force, method of impact, direction,
- Consciousness level.
- Other injuries. Life/ Limb threatening
- Other medical problems
-
Details of fracture:
- Pain. Swelling, Deformity, movement of injured part
- Wounds/ bleeding.
- Anti-Tetanus status (if skin breached)
- Other major injuries
-
Relate to function
-
Details of initial management
Additional Considerations
-
For all cases, ask about
- Progression
- Previous investigations
- Previous treatment
-
Careful:
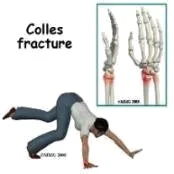
- Fractures are not always at the site of impact
- Some fractures do not need severe force
-
From Trauma history, you should be able to differentiate
- Low energy from High energy trauma
Low Energy Trauma
Key Questions
- When, Where, How?
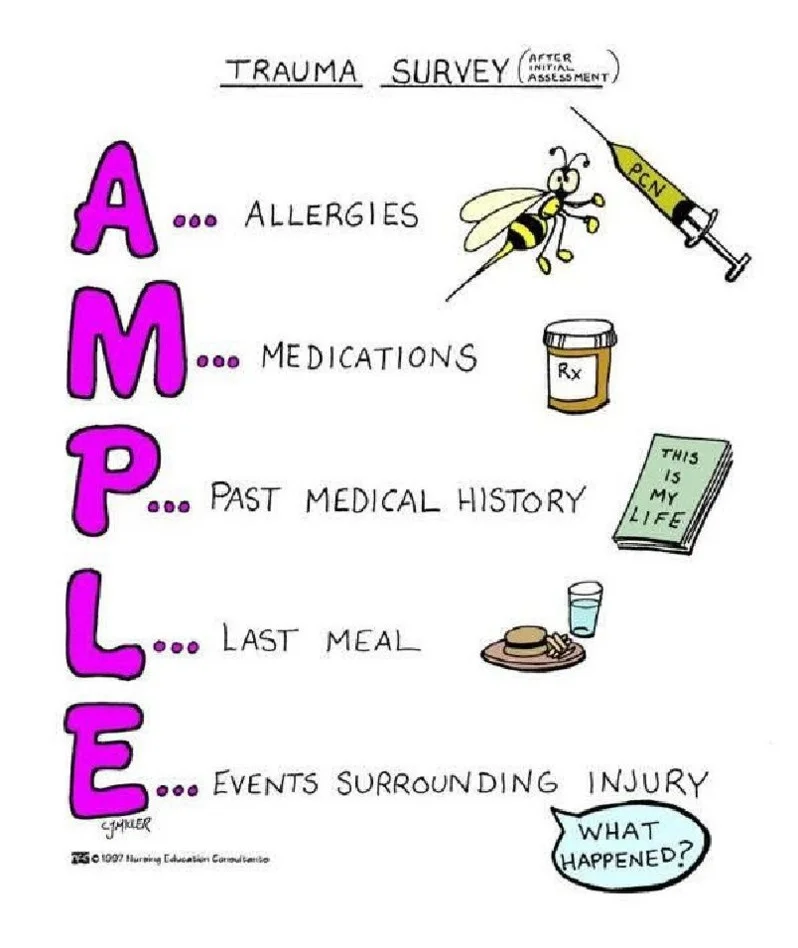
- AMPLE History (acute):
- Allergy,
- Medication,
- Past Medical & Surgical History,
- Last Meal,
- Event (How? Or Mechanism of injury)
All covered by our history, except: Last meal

High Energy Trauma
Road Traffic Accident (RTA)
- Low energy Qs,
- Driver / Passenger / Pedestrian
- Seat belted / non-belted
- Speed and location of impact
- Position of the patient and the limb at impact
- Severity of crash
- Need to use the “Jaws of Life”
- Type:
- Head-on collision. Side impact. Car turn-over




Fall from Height
- Low injury Qs
- How many levels
- Position of the patient and the limb at impact
- Missed injuries
- Combination injuries




Pathological Fractures
Considerations
- Minor trauma (e.g., slipped at home) indicates a pathological fracture
- In elderly:
- Osteoporosis: Diet, sun exposure, risk factors of osteoporosis
- Secondary metastasis: history of known malignancy, systematic review carefully looking for unknown primary
- In younger: look for cause of weak bone
- Osteomalacia, hyperparathyroid, bone disease
- In very young: local pathology: cyst, infection
- In elderly:
Trauma Case Histories
Case 1: Knee Injury
- A 25-year-old injured his knee while playing football
- Mechanism of injury
- Swelling:
- Immediate: hemarthrosis: Cruciate / fracture
- Later: effusion: meniscal injury
- History of locking / giving way
Case 2: Motor Vehicle Accident
- A 32-year-old female was brought to the emergency room after a motor vehicle accident
Case 3: Fall from Scaffold
- A 45-year-old man was seen in the emergency room after falling from a scaffold in a building site
Case 4: Hip Pain After Fall
- A 65-year-old lady presented to the emergency room with pain in right hip after falling at home