IM
Epilepsy
Professor Salih Bin Salih
Epilepsy Syndrome
Epilepsy syndromes may be classified according to:
- Whether the associated seizures are partial or generalized
- Whether the etiology is idiopathic or symptomatic/cryptogenic
- Several important pediatric syndromes can further be grouped according to age of onset and prognosis
-
EEG is helpful in making the diagnosis
-
Children with particular syndromes show signs of slow development and learning difficulties from an early age
Three most common epilepsy syndromes
- Benign childhood epilepsy
- Childhood absence epilepsy
- Juvenile myoclonic epilepsy
Three devastating catastrophic epileptic syndromes
Diagnosis in Epilepsy
Aims:
-
Differentiate between events mimicking epilepsy (syncope, vertigo, migraine, psychogenic non-epileptic seizures) Z
-
Confirm the diagnosis of seizure (or possibly associated syndrome) and the underlying etiology
Differential Diagnosis Z
- Syncope attacks
- Cardiac arrhythmias
- Migraine
- Hypoglycemia
- Narcolepsy (sudden attack of sleep)
- Panic attacks
- PSEUDOSEIZURES
Diagnosis in Epilepsy
Approach:
- History (from patient and witness)
- Physical examination
- Investigations
History
| * Event | |
| ○ Localization | |
| ○ Temporal relationship | |
| ○ Factors | |
| ○ Nature | |
| ○ Associated features | |
| * Past medical history | |
| * Developmental history | |
| * Drug and immunization history | |
| * Family history | |
| * Social history |
Physical Examination
- General ○ esp. syndrome or non-syndromal dysmorphic features, neurocutaneous features
- Neurological
- Other system as indicated ○ E.g. Febrile convulsion, infantile spasm
Investigation Z
-
Routine investigation: Haematology, biochemistry chest X-ray and toxicology
-
Electroencephalography (EEG). Neuroimaging (CT/MRI) should be performed in all persons aged 25 or more presenting with first seizure and in those pts. with focal epilepsy irrespective of age.
-
Specialised neurophysiological investigations: Sleep deprived EEG, video-EEG monitoring.
-
Advanced investigations: Semi Invasive or invasive EEG recordings, MR Spectroscopy, Positron emission tomography (PET) and ictal Single photon emission computed tomography (SPECT)
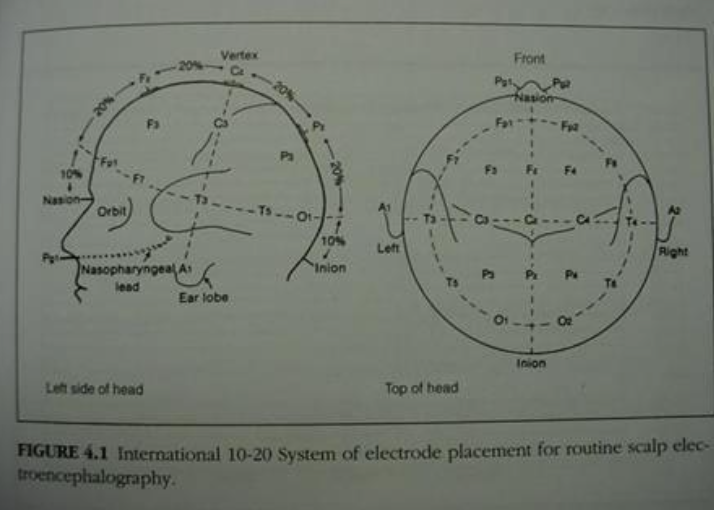
International 10-20 System of Electrode Placement in EEG
Neuroimaging
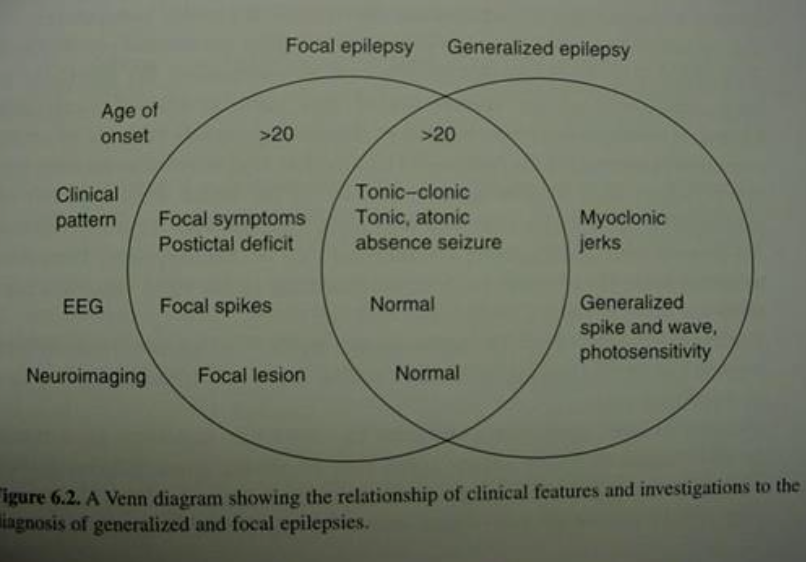
Venn Diagram
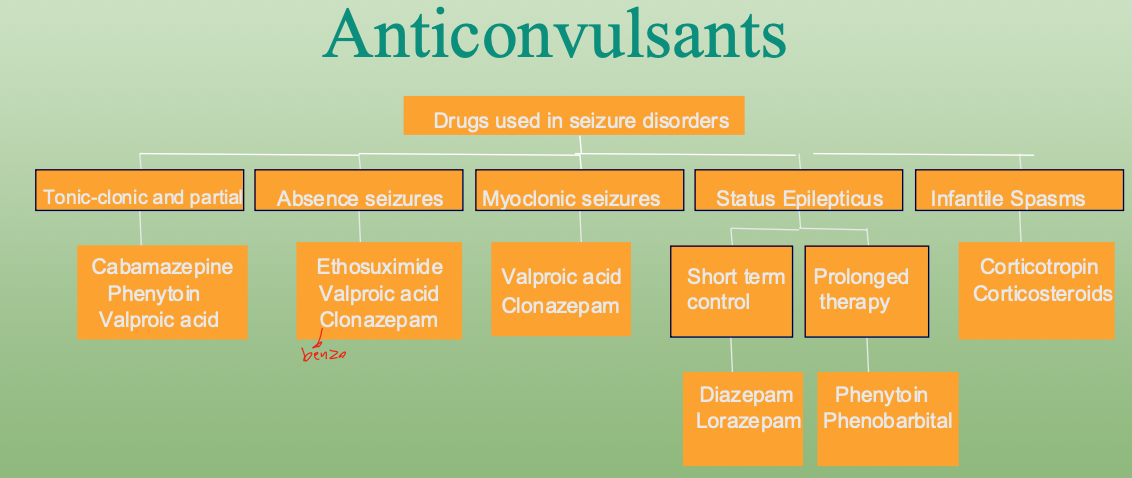
Anticonvulsants
Suppress repetitive action potentials in epileptic foci in the brain
- Sodium channel blockade
- GABA-related targets
- Calcium channel blockade
- Others: neuronal membrane hyperpolarisation
Anticonvulsants Z
Adverse Effects Z
- Teratogenicity ■ Neural tube defects ■ Fetal hydantoin syndrome
- Over dosage toxicity
- Life-threatening toxicity ■ Hepatotoxicity ■ Stevens-Johnson syndrome
- Abrupt withdrawal ⇒ seziure
Medical Intractability
- No known universal definition
- Risk factors ■ High seizure frequency ■ Early seizure onset ■ Organic brain damage
- Established after adequate drug trials
- Operability
Pediatrics
Epilepsy
- The tendency to have recurrent, unprovoked (reflex) seizures.
- At least two unprovoked (reflex) seizures occurring >24 hours apart.
- One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years.
- Diagnosis of an epilepsy syndrome.
Reflex Epilepsies
Evoked by specific external sensory stimuli (e.g., photosensitive epilepsies), internal cognitive and emotional processes, or activity of the patient (e.g., reading). - (not a medical cause in stress)
An Epilepsy Syndrome
Represents a complex of signs and symptoms that together define a distinctive clinical seizure disorder, e.g., West syndrome or Lennox-Gastaut syndrome.
Incidence/Prevalence
- Incidence rates of epilepsy in childhood range from 0.5 to 8 per 1,000 person-years.
- An estimated 1% of children and adolescents in the United States will experience at least one unprovoked seizure by age 14 years.
- In Saudi Arabia, 6.54 per 1000 population have active epilepsy.
Surgery Z
- Curative (Resection)
- Palliative ■ Vagal nerve stimulation
Aetiology of Status Epilepticus Z
○ Idiopathic status epilepticus ■ Non-compliance to anticonvulsants ■ Sudden withdrawal of anticonvulsants ■ Sleep deprivation ■ Intercurrent infection
○ Symptomatic status epilepticus ■ Anoxic encephalopathy ■ Encephalitis, meningitis ■ Congenital malformations of the brain ■ Electrolyte disturbances, drug/lead intoxication, extreme hyperpyrexia, brain tumour
Status Epilepticus
- A condition when consciousness does not return between seizures for more than 30 min. This state may be life-threatening with the development of pyrexia, deepening coma and circulatory collapse. Death occurs in 5-10%.
- Treatment: AEDs intravenously ASAP, event. general anesthesia with propofol or thiopentone should be commenced immediately.
Medication Used in Status Epilepticus
-
Stop Seizure Benzodiazepine
-
Prevent Recurrence Epanutin, Valproate and Levetiracetam