KAWASAKI DISEASE

INTRODUCTION
- KD is second only to HSP as the most common vasculitis of childhood.
- The underlying etiology is unknown.
- The incidence of KD is greatest in children who live in East Asia or are of Asian ancestry living in other parts of the world, suggesting a genetic predisposition.
- It is typically a self-limited condition, with fever and other acute inflammatory manifestations (12 days).
- KD is a systemic, inflammatory illness that particularly affects medium-sized arteries.
EPIDEMIOLOGY
-
Positive family history in about 1%. Boys are more susceptible than girls.
-
Siblings of children with KD in Japan are at increased risk for developing the disease, which usually occurs within one week of onset of the index case.
-
The risk of occurrence in twins is 13%
-
Occurs in epidemics with geographic wave-like spread
-
80% of children are <5 years old, with most cases in less than 2 years old; relatively uncommon among children younger than six months. Occurrence beyond late childhood is rare.
-
More common during the winter and early spring months.
-
KD is characterized by a febrile exanthem with lymphadenitis and mucositis. These are features similar to those of contagious diseases, such as adenovirus infection, measles, and scarlet fever.
-
There is spatial and temporal clustering of cases.
-
Multisystem inflammatory syndrome in children with COVID-19 is associated with hyperinflammatory syndromes. Children may develop organ failure involving the gastrointestinal tract, heart, central nervous system, kidneys, and other systems. The severe inflammation, cytopenias, coagulopathy, and hyperferritinemia are similar to macrophage activation syndrome or toxic shock in some children. Others develop mucocutaneous symptoms like those in KD. In a percentage of such cases, coronary artery dilatation, and even formation of giant coronary aneurysms, may develop.
DIAGNOSIS
Table 1 Diagnostic criteria for Kawasaki disease. Fever of at least 5 days duration plus four of the following features:
- Bilateral conjunctival injection
- Polymorphous exanthem
- Changes in the lips and oral cavity
- Cervical lymphadenopathy (>1.5cm)
- Changes in the extremities:
- Erythema of the hands and feet
- Swelling of the hands and feet
- Desquamation Other diseases must be excluded
Diagnosis made by
- ≥5 days of fever and ≥4 of the 5 principal clinical features
- Typically, all of the clinical features are not present at a single point in time
- In the presence of 4 of 5 classic criteria, US and Japanese experts agree that only 4 days of fever are necessary before initiating treatment
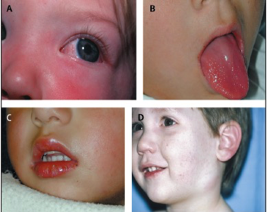
- A: Bilateral, non-exudative conjunctival injection with perilimbal sparing.
- B: Strawberry tongue with loss of filiform papillae and persistence of fungiform papillae (“seeds” of strawberry).
- C: Erythematous, fissured lips.
- D: Unilateral enlarged left jugulodigastric nodes.
 bilateral nonexudative
conjunctivitis ; dry, fissured, erythematous lips and a “strawberry” tongue ; erythematous and edematous
hands and feet ; an erythematous truncal rash and a desquamating perineal rash .
bilateral nonexudative
conjunctivitis ; dry, fissured, erythematous lips and a “strawberry” tongue ; erythematous and edematous
hands and feet ; an erythematous truncal rash and a desquamating perineal rash .
INVESTIGATIONS
- Thrombocytosis appears in the second week of the illness: 500,000 to >1 million/mm3
- Thrombocytopenia is seen rarely
- Elevation of ESR and CRP is universal.
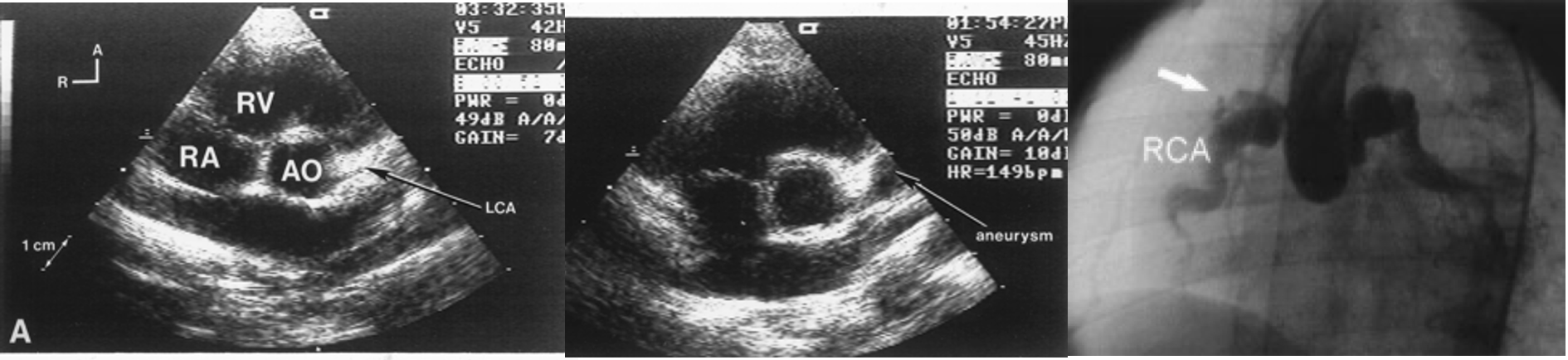
- Echocardiography: 20% of untreated patients develop coronary aneurysm, which regresses in most patients within 1-2 years.
- US of abdomen: Hydrops of the gallbladder
- Urine: sterile pyuria
Complications
KD can cause coronary artery aneurysms. Increased risk:
- Late diagnosis and delayed treatment with IVIG.
- Age younger than one year or older than nine years.
- Male sex
- Fever ≥14 days
- Serum sodium concentration less than 135 meq/L.
- Hematocrit less than 35%. WBC >12,000/mm3.
- Cardiomyopathy, myocardial infarction, arrhythmias.
- Visceral vascular involvement (GIT, renal, CNS) and peripheral arterial occlusion.
- KD shock syndrome (sustained systolic hypotension).
- Macrophage activation syndrome (DIC, cytopenias, and thrombosis).
- Thrombocytosis
TREATMENT
- IVIG decreases the incidence of coronary aneurysms from 20% to 5% (if used before day 10)
- Give in the first 10 days and preferably within 7 days of illness.
- Aspirin:
- Additive anti-inflammatory effects to IVIG.
- Does not appear to lower the frequency of the development of coronary abnormalities.
- During the acute phase of illness, aspirin dose 80-100 mg/kg per day.
- Reduce the aspirin dose after the child has been afebrile for 48 to 72 hours.
- Low-dose aspirin (3-5 mg/kg per day) is maintained until the patient shows no evidence of coronary changes by 6 to 8 weeks after the onset of the illness.
- For children who develop coronary abnormalities, aspirin may be continued indefinitely.
Additional therapy for patients at high risk for IVIG resistance
- REFRACTORY KD: Fever persists or returns in 10 to 15 percent of patients
- Glucocorticoids: 2 mg/kg/day of intravenous prednisolone for five days, then switch to oral dosing starting with 2 mg/kg/day for five days, then 1 mg/kg/day for five days, and then finally 0.5 mg/kg/day for five days or until afebrile
- Cyclosporine.
- Tumor necrosis factor inhibition: etanercept or infliximab.
- Antithrombotic therapy
Prognosis
- Mild dilatation (3-4 mm) regresses within 2 years.
- 80% of those with moderate dilatation (4-8 mm) regress within 5 years.
- Giant aneurysms (>8 mm) are unlikely to resolve, and many progress to stenosis or complete obstruction within years of the initial diagnosis.
Differential Diagnosis
- Measles, echovirus, adenovirus, and EBV infections.
- Infantile polyarteritis nodosa, juvenile idiopathic arthritis, leptospirosis, Lyme disease, mercury toxicity, rocky mountain spotted fever, toxic epidermal necrolysis, staphylococcal scalded skin syndrome, SLE.
- Stevens-Johnson syndrome/drug-induced rash.
- Meningococcemia, rickettsial disease
- Pharyngoconjunctival fever, herpangina, and primary herpetic gingivostomatitis.