History and Examination of Female
- Menstrual cycle (regular, irregular), Previous infections & PID, Hirsutism, Dysmenorrhea, Prolactinoma & Galactorrhea, Contraception history, Family Hx of the same problem, previous marriage and children, previous infertility investigations and management.
- Sexual history (Q for both couple)
A- Anovulation/Oligoovulation (Ovarian)
Causes:
-
Physiological: Post OCPs, Lactation.
-
Pathological:
A. General causes: as amenorrhea and in addition:
- Age, Weight (fertility with age and overweight/obesity)
- Psychological
- Cigarettes smoking and addiction.
- Environmental toxins
B. Hypothalamic and pituitary causes (= all causes of amenorrhea).
C. Ovarian causes:
- Premature ovarian failure
- PCO
- Luteal phase defect
Diagnosis
-
Clinical
- A-Symptoms: absence of normal symptoms of ovulation which are (any one or more):
- Regular cyclic menstruation.
- Ovulation pain = mid-cyclic pain ”= MiettleSchmerz pain”.
- Ovulation spotting.
- Premenstrual mastalgia.
- B-Signs:
- Signs Document ovulation
- increase basal body temperature early in the morning.
- Changes in characters of cervical mucous (become slippery)
- Signs Document ovulation
- A-Symptoms: absence of normal symptoms of ovulation which are (any one or more):
-
Investigations:
-
A- Lab: Hormonal assay
- Day 3 FSH & LH
- Day 21 Progesterone level in blood
- L.H level in plasma and urine.
- E2
- Prolactin
- Testosterone, and its derivatives in hyperandrogenism.
- TFT
- Anti-müllerian hormone (AMH) levels can also be helpful in predicting ovarian reserve
-
B- Radiological:
- U.S For serial measurements of follicular growth and maturation, “the mature Graffian follicle is about 18-25 mm”.
-
C- Histopathological:
- Premenstrual endometrial biopsy show NO secretory changes OR luteal phase defect.
-
Treatment of Ovarian Factor
-
Correction of general condition:
- Treatment of general causes e.g., D.M, T.B, etc.
- Treatment of hypothyroidism
- Treatment of hypothalamic and pituitary causes.
- Treatment of hyper-prolactinemia (Bromocriptine and Cabergolin as anti-prolactin).
- Progesterone for luteal phase defect in the second half of the cycle.
-
Induction of ovulation:
- Clomiphene citrate (Clomid) = antiestrogen: oral 50-100 mg/day from the 3rd day for 5-7 days (first-line medication).
- Mechanism: By blocking the receptors of estrogen so blocking the negative feedback mechanism on the hypothalamus and pituitary with subsequent increase in F.S.H & L.H and thus ++follicular growth and ovulation.
- It increases the sensitivity of the ovary to gonadotrophins.
- Gonadotrophins. (FSH OR HMG)
- H.C.G = human chorionic gonadotrophins. (injection to trigger ovulation)
- Tamoxifen as selective direct estrogen receptor inhibition.
- Metformin as anti-insulin in PCOS.
- Clomiphene citrate (Clomid) = antiestrogen: oral 50-100 mg/day from the 3rd day for 5-7 days (first-line medication).
Ovarian Hyper-stimulation
- It is a common complication of induction of ovulation as the ovaries may enlarge up to 12 cm OR more with a risk of peritoneal irritation and OR ovarian rupture.
- It may be mild, moderate, or severe.
- In mild form; there is abdominal distension, pain, sickness, and diarrhea.
- In moderate form; there may be excess fluid in the abdomen leading to more pain and discomfort.
- In severe form; the case may be life-threatening as there may be free fluid in the abdomen (low albumin), hemoconcentration, and hypercoagulability.
Ascites
B- Tubal Factor of Infertility
Causes:
- Congenital: tubal aplasia, hypoplasia, diverticulum.
- Traumatic: trauma during operation followed by adhesions.
- Inflammatory: following P.I.D ---: “adhesions the commonest cause in the tube”.
- Neoplastic: e.g., small cornal fibroid closing the tubal ostia.
- Endometriosis: causing pelvic adhesions.
- Disturbed physiology: e.g., Poor ciliary movement.
Diagnosis/Investigations:
- A-Hysterosalpingography = H.S.G: the main line used for diagnosis by “tubal patency tests”.
-
The idea: Inject radio-opaque dye in the uterus to pass through the tubes to the peritoneal cavity.
-
Then the lower abdomen and pelvis are photographed.
-
Timing of the test: it should be done post-menstrual to minimize chances of interrupting a pregnancy.
-
Complications:
- Neurogenic shock, hemorrhage due to trauma,
- Infection, perforation of uterus, endometriosis, oil embolism, dye allergy.
-
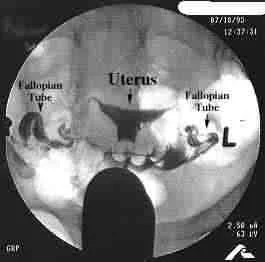
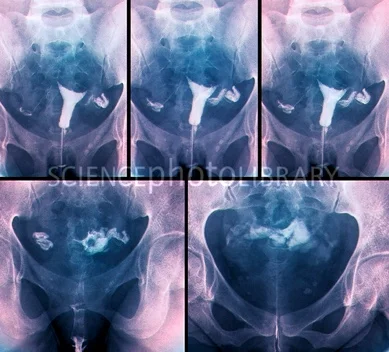
Values of HSG:
- Diagnostic for: intrauterine and tubal disorder
- Therapeutic for:
- Removal of mucous plug that may close the tube.
- Removal or absorption of thin adhesions.
- Straightening of kinked tube or relief of uterotubal spasm.
B-Laparoscopy with Dye Injection:
- By injection of methylene blue dye through the cx if passed from the fimbrial end = patent tubes.
Treatment:
- IVF
C- Cervical Factor of Infertility
Causes:
- Congenital:
- Traumatic
- Inflammatory: endocervicitis, “common organisms are chlamydia and gonorrhea”.
- Neoplastic: cervical fibroid and masses blocking or distorting the cx.
- Immunological i.e., presence of anti-sperm antibodies.
- Hormonal: especially decreased estrogen causing decreased mucous and rendering it thick.
Diagnosis:
- Cervical culture
- Postcoital tests: for patients with history or physical exam findings suggestive of cervical factor.
- The validity of the test is controversial.
Treatment:
- Treat underlying cause
D- Uterine Factor of Infertility
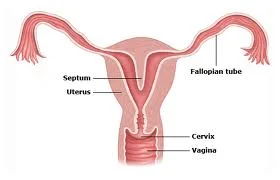
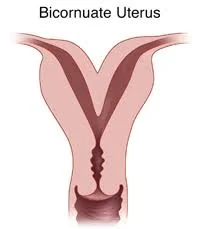
- Uterine factors include leiomyomata, intrauterine synechiae (Asherman syndrome), septae, and other müllerian anomalies.
- Fibroid - Adhesions
Investigation:
- Pelvic US
- Saline infusion ultrasonography (sonohysterography [SHG])
- HSG
- Hysteroscopy: Reserved for those patients with HSG or SHG results that need further evaluation.
- Laparoscopy: Septate and bicornuate uterus are similar in HSG and differentiate between them by Laparoscopy.
Treatment:
- According to Cause.
- Surgery, adhesiolysis in Asherman’s.
- Polypectomy OR myomectomy in fibroid.
- Removal of septum if septate uterus.
F- Pelvic and Peritoneal Factor
- Any gross pathology in the pelvis may disturb the function/movement of tubes/ovaries like endometriosis, adhesions, or PID.
Diagnosis:
- Laparoscopy.
- Ultrasound can diagnose endometrioma / hydrosalpinx
Treatment:
- Treatment of the cause.
- Endometriosis: remove endometrioma > 3 cm if present, lysis and excision of endometriosis if indicated.
-
mild endometriosis >> ovulation induction +/- IUI.
-
if failed or moderate/severe endometriosis >> IVF.
-
- Endometriosis: remove endometrioma > 3 cm if present, lysis and excision of endometriosis if indicated.