Definition:
failure of the body cells to respond to endogenous or exogenous insulin.
Diagnosis:
By homeostasis model assessment (HOMA Formula): IR index = Fasting insulin (uU/ml) x Fasting glucose (mg/dl)/ 405 Y
- HOMA< 20= insulin sensitivity.
- HOMA > 20 = insulin resistance.
Causes and mechanism:
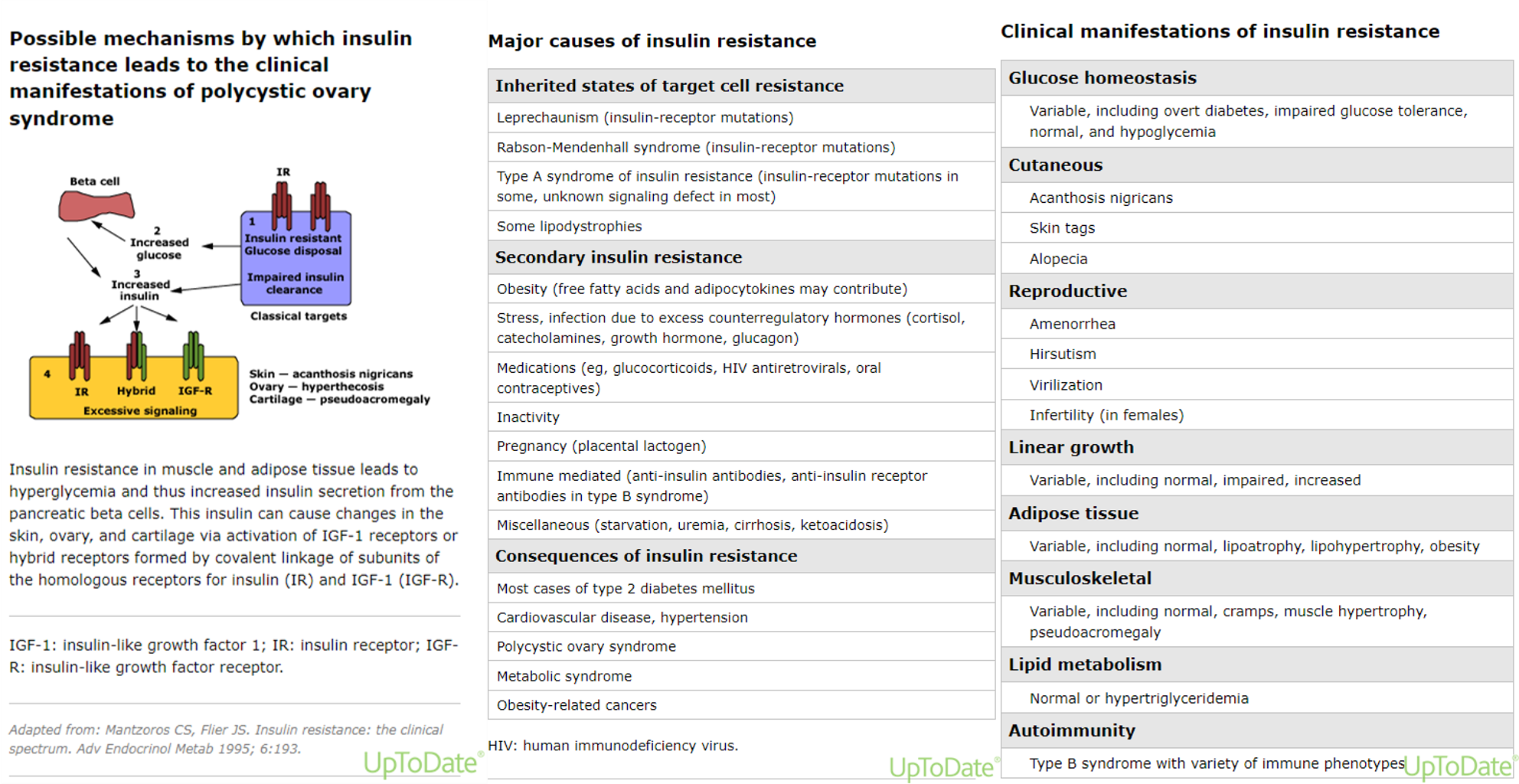
- Immunological (pre-receptors defect): due to formation of IgA or IgG antibodies against insulin.
- Non-Immunological(receptors defect): occurs due to down-regulation of insulin receptors) such as:
- The metabolic syndrome: it means association of central obesity, hypercholesterolemia, hyperinsulinemia, and insulin resistance.
- Obesity.
- Pregnancy.
- Severe infection or stress.
- Corticosteroids.
3- Post-receptor defect (intracellular): abnormal signal transduction due to genetic defect.
4- Local insulin resistance: due to degradation of insulin in s.c. tissue by proteolytic enzymes. It is diagnosed by changing the route of administration to i.v. injection. If there is good response, then the resistance is local.
5- Hepatitis C makes people three to four times more likely to develop type 2 DM and insulin resistance.
THERA Physiology
Definition and Diagnosis of Insulin resistance
Insulin resistance may be defined as a subnormal glucose response to endogenous and/or exogenous insulin.
The diagnosis of insulin resistance in most patients is based upon clinical findings (eg, metabolic syndrome traits):
- Abdominal obesity
- Hyperglycaemia
- Dyslipidaemia
- Hypertension
- Hyperinsulinemia
Insulin resistance syndromes
There are two types of insulin resistance – insulin resistance syndrome type A and type B.
-
Type A syndrome: Insulin can’t bind well because insulin receptors are either absent or malfunctioning due to genetic mutation.
-
Type B syndrome: It is very rare that antibodies are produced against the insulin receptors. When antibodies are directed against the receptors, they block them, and insulin can’t bind as well.