Seizures and Epilepsy
Professor Salih Bin Salih
-
A chronic neurologic disorder manifesting by repeated seizures (attacks or fits) which caused by paroxysmal uncontrolled discharges of neurons within the central nervous system (gray matter disease).
-
The clinical manifestations range from a major motor convulsion to a brief period of lack of awareness. The stereotyped and uncontrollable nature of the attacks is characteristic of epilepsy.
DEFINITION
-
Seizure (Convulsion) Clinical manifestation of synchronized electrical discharges of neurons
-
Epilepsy Present when 2 or more unprovoked seizures occur at an interval greater than 24 hours apart
-
Provoked seizures Seizures induced by somatic disorders originating outside the brain (E.g. fever, infection, syncope, head trauma, hypoxia, toxins, cardiac arrhythmias)
-
Status epilepticus (SE) Continuous convulsion lasting longer than 30 minutes OR occurrence of serial convulsions between which there is no return of consciousness no regain consciousness
-
Idiopathic seizure: Seizure develops in the absence of an underlying CNS lesion/insult
-
Symptomatic seizure: Seizure occurs as a result of an underlying neurological disorder or a metabolic abnormality
INTRODUCTION
-
Incidence: Approximately 45/100,000 per year
-
Prevalence: 0.5-1% (2.5 million with epilepsy)
- 14 years or younger 13%
- 15 to 64 years most 63% Z
- 65 years and older 24%
-
Cumulative risk of epilepsy: 1.3% - 3.1%
-
Epilepsy refractory to AEDs: 20-30%
Aetiology of Seizures
-
Epilepsy
- Idiopathic (70-80%)
- Cerebral tumour
- Neurodegenerative disorders
- Neurocutaneous syndromes
- Secondary to:
- Cerebral damage: e.g. congenital infections, HIE, intraventricular haemorrhage
- Cerebral dysgenesis/malformation: e.g. hydrocephalus
-
Non-epileptic
- Febrile convulsions
- Metabolic
- Hypoglycaemia, Hypocalcaemia,
- Hypomagnesaemia, Hypernatremia and Hyponatremia
- Head trauma
- Meningitis cns infection
- Encephalitis
- Poisons/toxins
Pathogenesis
-
The 19th century neurologist Hughlings Jackson suggested “a sudden excessive disorderly discharge of cerebral neurons“ as the causation of epileptic seizures.
-
Recent studies in animal models of focal epilepsy suggest a central role for the excitatory neurotransmitter glutamate (increased) and inhibitory gamma aminobutyric acid (GABA) (decreased)
Pathophysiology
-
Abnormal tissues — tumour, AVM, dead area only in CNS These regions of the brain may promote development of novel hyperexcitable synapses that can cause seizures
-
Genetic factors ○ At least 20 % ■ Benign neonatal convulsions. ■ Juvenile myoclonic epilepsy. ■ Progressive myoclonic epilepsy.
Seizure Classification Z
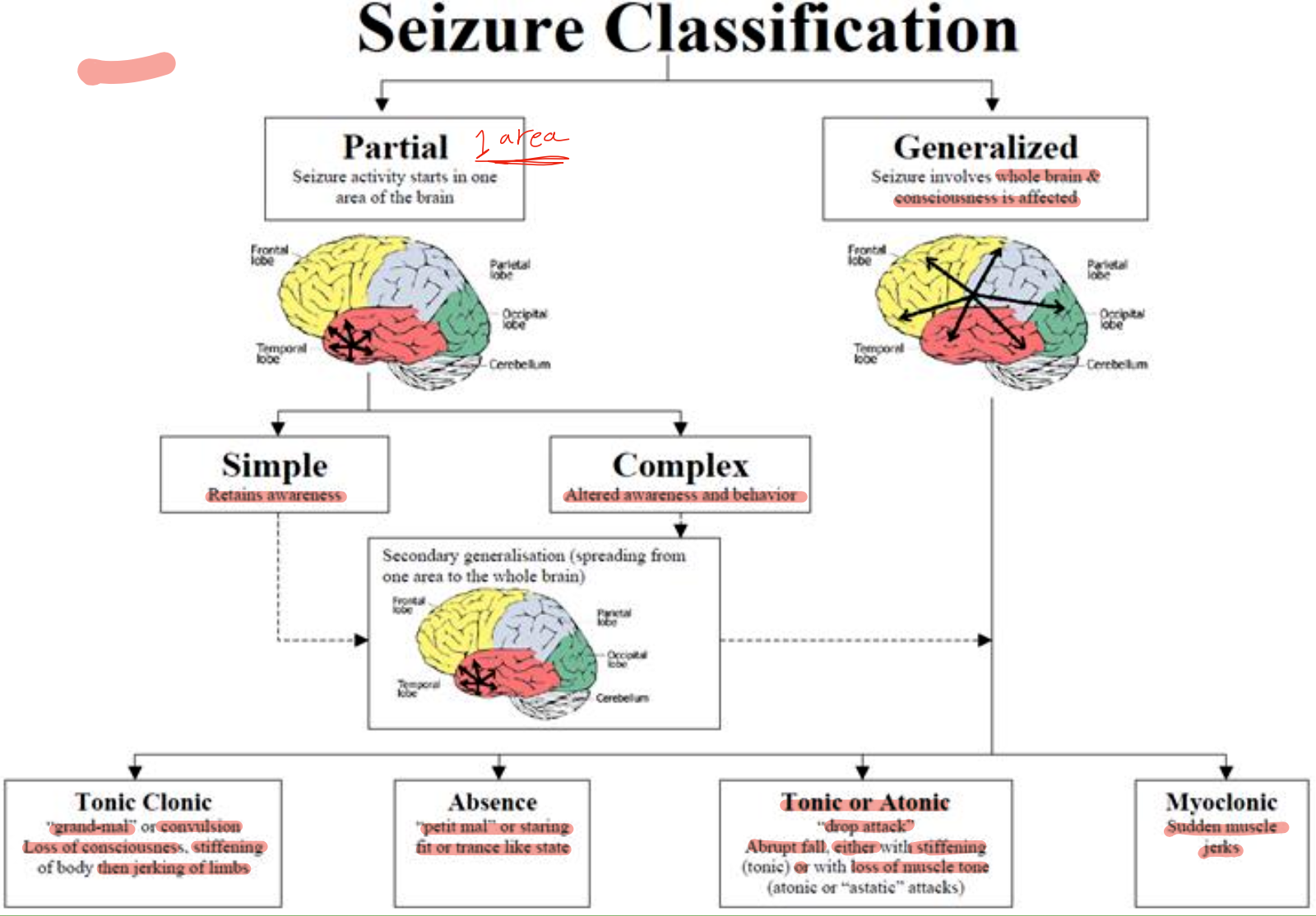
Partial 1 area Seizure activity starts in one area of the brain
Generalized Seizure involves whole brain & consciousness is affected
Simple Retains awareness
Complex Altered awareness and behavior
Secondary generalisation (spreading from one area to the whole brain)
Tonic Clonic “grand-mal or convulsion Loss of consciousness, stiffening of body then jerking of limbs
Absence “petit mal” or staring fit or trance like state
Tonic or Atonic “drop attack” Abrupt fall, either witt stiffening (tonic) or with loss of muscle tone (atonic or “astatic” attacks)
Myoclonic Sudden muscle jerks
Classification
-
The modern classification of the epilepsies is based upon the nature of the seizures rather than the presence or absence of an underlying cause.
-
Seizures which begin focally from a single location within one hemisphere are thus distinguished from those of a generalised nature which probably commence in a deeper structures (brainstem) and project to both hemispheres simultaneously.
Seizures Z
| Partial | Generalized |
|---|---|
| * Electrical discharges in a relatively small group of dysfunctional neurons in one cerebral hemisphere | * Diffuse abnormal electrical discharges from both hemispheres |
| * Aura may reflect site of origin hear - smell - visual warning | * No warning |
| * +/- LOC | * Always LOC |
-
Partial Seizure
-
Generalized Seizure
-
Absence Seizure
-
Myoclonic Seizure
-
Tonic-Clonic Seizure
-
Atonic Seizure
Seizure Therapy Z
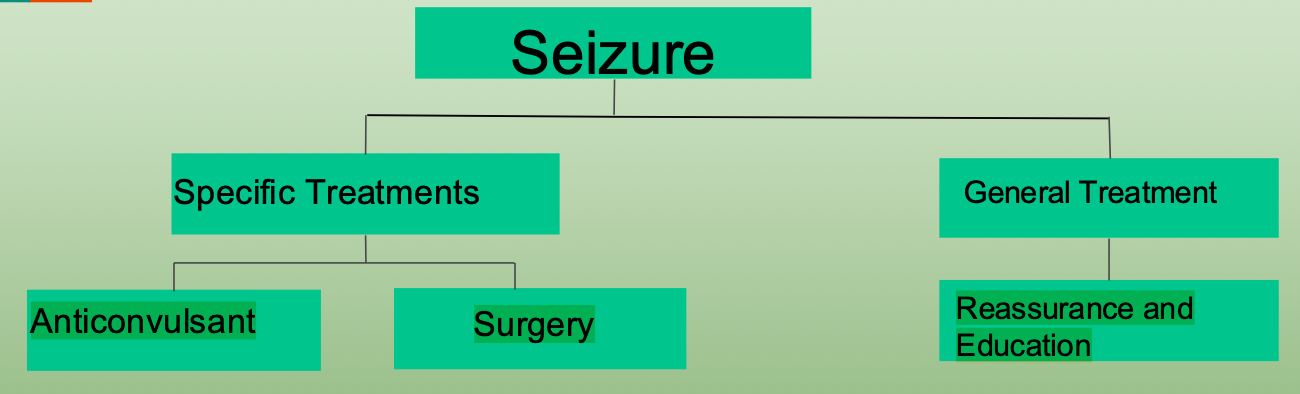
Seizure
Specific Treatments
- Anticonvulsant
- Surgery
General Treatment
- Reassurance and Education
Education & Support
- Information leaflets and information about support group
- Avoidance of hazardous physical activities
- Management of prolonged fits ○ Recovery position ○ Rectal diazepam relieve attack
- Side effects of anticonvulsants
Treatment Z
-
The majority of pts respond to drug therapy (The treatment target is seizure-freedom and improvement in quality of life)
-
The commonest drugs used in clinical practice are: Carbamazepine, Sodium valproate, Lamotrigine (first line drugs) Levetiracetam, Topiramate, Pregabaline (second line drugs) Z
-
Basic rules for drug treatment: Drug treatment should be simple, preferably using one anticonvulsant (monotherapy). “Start low, increase slow“. Add-on therapy is necessary in some patient Z
-
If patient is seizure-free for three years, withdrawal_of_pharmacotherapy should be considered. Withdrawal should be carried out only if patient is satisfied that a further attack would not ruin employment etc. (e.g. driving license). It should be performed very carefully and slowly! 20% of pts will suffer a further sz within 2 yrs.
-
The risk of teratogenicity is well known (~5%), especially with valproates, but withdrawing drug therapy in pregnancy is more risky than continuation. Epileptic females must be aware of this problem and thorough family planning should be recommended. Over 90% of pregnant women with epilepsy will deliver a normal child.\