Celiac Disease
Introduction
Celiac disease, also known as gluten-sensitive enteropathy,
is the most common genetically related food intolerance worldwide. It is a multifactorial, autoimmune disorder that occurs in genetically susceptible individuals.
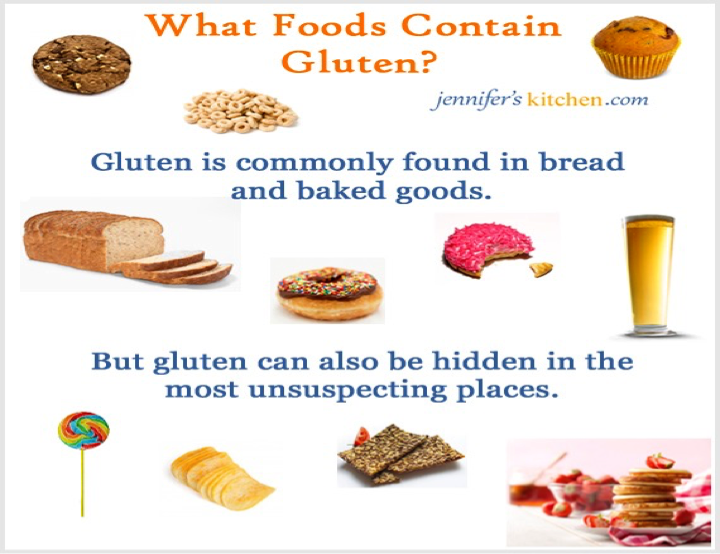
It is triggered by a well-identified environmental factor (gluten and related prolamin present in wheat, rye, and barley). - cross allergy can happen to oats that dont contain gluten
Gluten is a form of protein found in some grains. The damage to the intestine makes it hard for the body to absorb nutrients, especially fat, calcium, iron, and folate.
Pathophysiology
Celiac disease is an autoimmune disease, and the enzyme tissue transglutaminase (tTG) is the autoantigen against which the abnormal immune response is directed.
Gluten is the single major environmental factor that triggers celiac disease, which has a narrow and highly specific association with class II haplotypes of HLA DQ2.
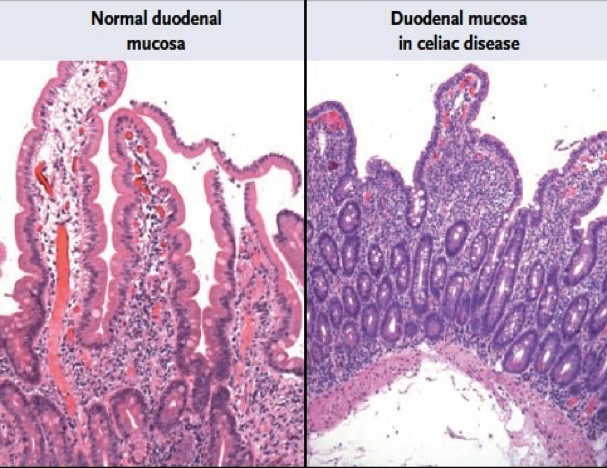
This causes inflammation in the intestines and damages the villi, the hair-like structures on the lining of the small intestine, causing malabsorption.
Presentations of Celiac Disease
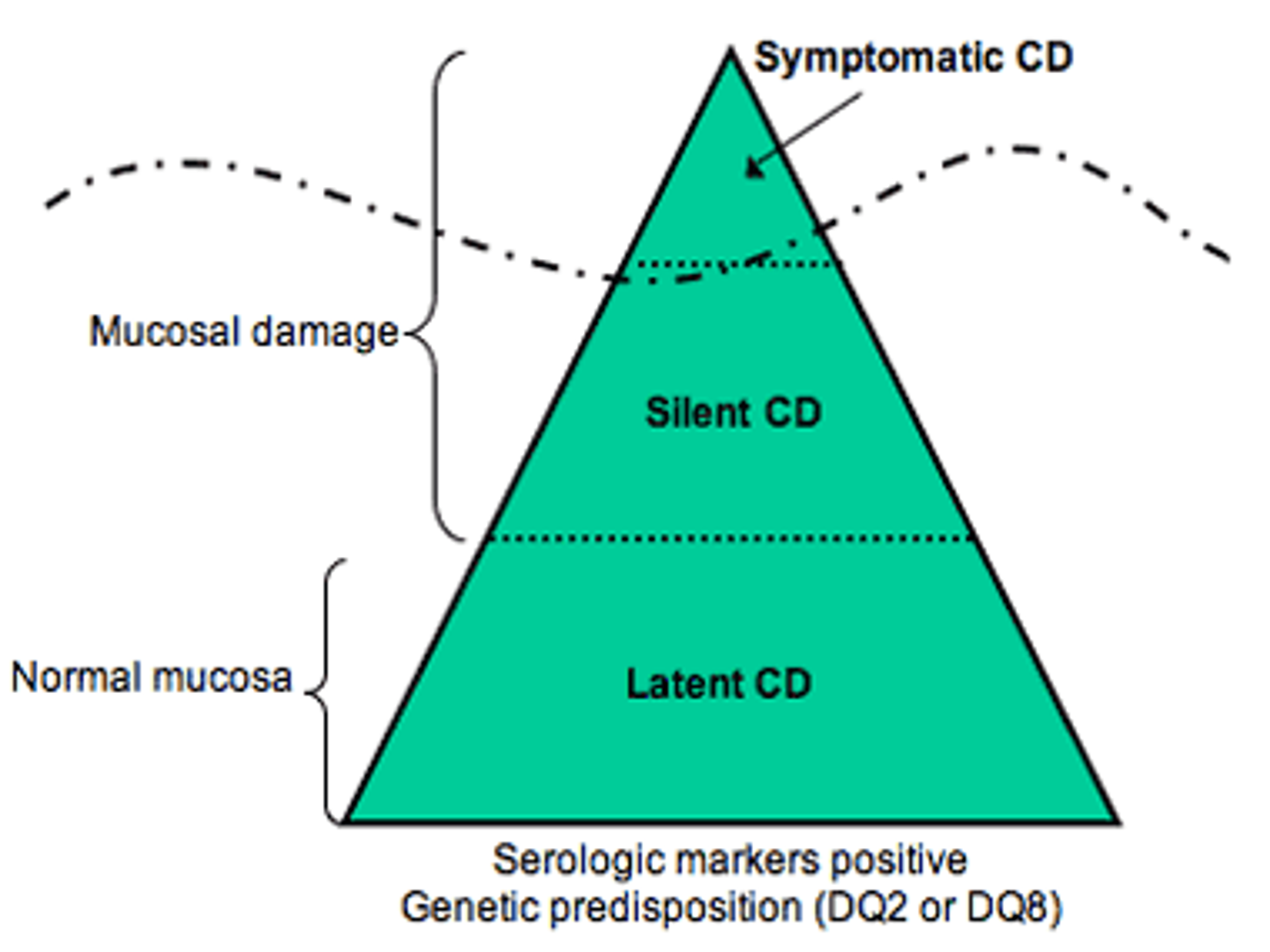
Currently, five possible presentations of celiac disease are recognized:
- Typical: Primarily characterized by GI signs and symptoms.
- Atypical: GI signs and symptoms are minimal or absent, and various extraintestinal manifestations are present.
- Silent: The small intestinal mucosa is damaged, and celiac disease autoimmunity can be detected with serology; however, no symptoms are present.
- Potential: Patients have a positive specific autoimmune serology and may or may not be symptomatic, but the mucosa morphology is normal. These individuals have genetic compatibility with celiac disease and full-blown celiac disease may develop at a later stage in some or all of these individuals.
- Latent: Individuals with normal mucosal morphology who “have had a gluten-dependent enteropathy at some point in their life.” This subset of patients is the rarest of the group.
Symptoms of Celiac Disease
Asymptomatic or minimally symptomatic celiac disease is probably the most common form of the disease, especially in older children and adults.
Gastrointestinal Symptoms
- Frequent loose stool; Chronic or recurrent diarrhea
- Abdominal pain, bloating
- Constipation
- Anorexia
- Vomiting
- Failure to thrive or weight loss
Extra-Intestinal Manifestations
-
Dermatitis Herpetiformis and other skin disorders
-
Dental enamel hypoplasia
-
Osteopenia/Osteoporosis (ADULTS)
-
Short stature
-
Delayed puberty
-
Iron-deficient anemia resistant to oral Fe
-
Liver and biliary tract disease (ADULTS)
-
Arthritis (ADULTS)
-
Neurological problems
- Ataxia
- Peripheral neuropathy
- Epilepsy
-
Psychiatric disorders
-
Women sub-infertility (ADULTS)
- Miscarriages
- Low birth weight babies
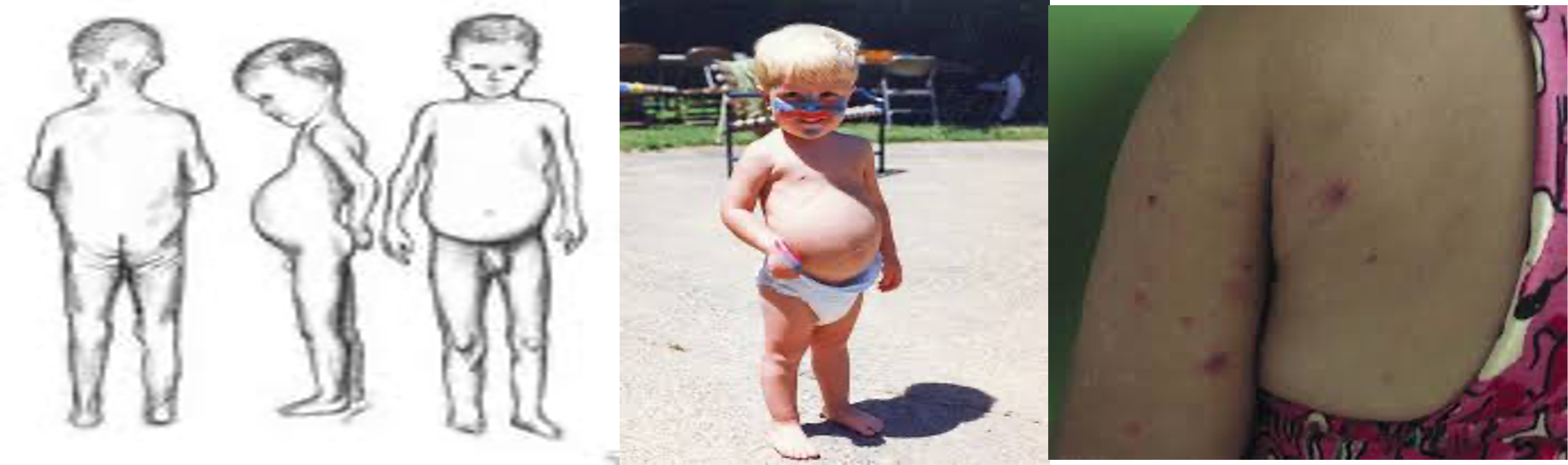
Physical Findings
Examination findings depend on the extent of celiac disease. Dry mucosal membranes with vomiting or diarrhea indicate the degree of dehydration. Oral aphthae (aphthous ulcers) are more frequent than in the normal population. Dental enamel hypoplasia is a highly specific but relatively uncommon finding. Bloating of the abdomen, potbelly, and muscle wasting. Failure to thrive.

Health Problems Accompanying Celiac Disease
-
Osteoporosis, which leads to fractures due to decreased calcium and vitamin D absorption.
-
Miscarriage or infertility in adult females.
-
Birth defects, such as neural tube defects caused by poor absorption of folic acid.
-
Seizures.
-
Intestinal T-cell lymphoma.
-
Other autoimmune diseases:
- Thyroid disease
- Type 1 diabetes
- Lupus
- Rheumatoid arthritis
- Sjögren’s syndrome
Epidemiology
- Prevalence among the general population is 3% in Saudi Arabia. Globally, celiac disease affects 1%.
- The prevalence of CD in Down’s syndrome patients was 10% in Saudi Arabia.
- Most studies indicate a female-to-male prevalence ratio ranging from 1.5:1 to 3:1.
- Classic GI pediatric cases usually appear in children aged 9-18 months usually after weaning, year later mucosal damage may persist in children.
Prognosis
Evidence suggests that the risk of mortality is increased in proportion to the diagnostic delay.
Subjects who do not follow a gluten-free diet have an increased risk of mortality, as high as 6 times that of the general population.
The increased death rates are most commonly due to intestinal malignancies that occur within 3 years of diagnosis.
Differential Diagnoses
- Autoimmune enteropathy
- Cystic Fibrosis
- Inflammatory Bowel Disease
- Irritable Bowel Syndrome
- Protein Intolerance
Diagnosis
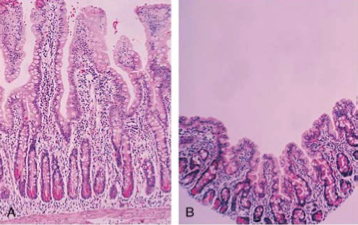
Duodenal mucosa histology changes in celiac disease (CD) are documented while on a gluten-containing diet and are characterized by a progressive deterioration of the villous architecture associated with a progressive increase in crypt length and density. Biopsy samples are now almost universally obtained by endoscopy.
Multiple biopsy samples (at least 4): are recommended because celiac disease may be patchy and areas of villous atrophy may be adjacent to normal areas.
In addition, biopsy from the duodenal bulb is also recommended, as about 2-3% of celiac children may have changes only in that part of the duodenumZ.
Intestinal Biopsy of Patient with Chronic Diarrhea, Abdominal Distention
In Clinical Practice
It is recommended to obtain first serologic tests for celiac disease (namely the anti-TTG-Ig A) and then to proceed with the intestinal biopsy to diagnose the condition in positive cases.
Serology, especially TTG, also has a major role in monitoring response to treatment.
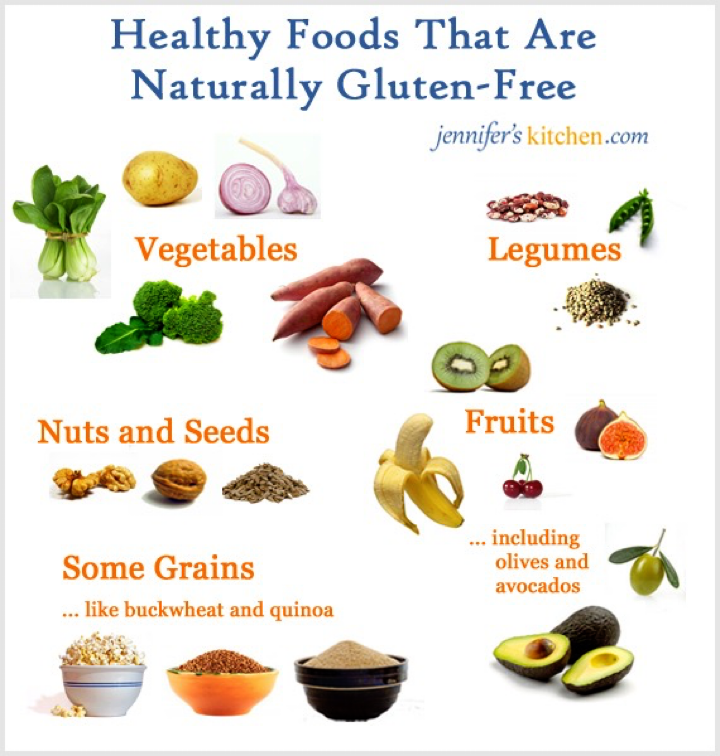
Treatment
-
Medical Care
-
Total lifelong avoidance of gluten ingestion is the cornerstone treatment for patients with celiac disease (CD).
-
Wheat, rye, and barley are the grains that contain toxic peptides. They should be eliminated as completely as possible, although daily intake doses larger than 10 mg are likely needed to cause a mucosal reaction.
-
Lactose is often eliminated in the initial phases of dietary treatment as well. This is because lactase deficiency is thought to accompany the flat mucosa.
- Lactose is often eliminated in the initial phases of dietary treatment as well. This is because lactase deficiency is thought to accompany the flat mucosa.
GI symptoms in patients with symptomatic celiac disease who adhere to a gluten-free diet typically resolve within a few weeks; these patients experience the normalization of nutritional measures, improved growth in height and weight (with resultant normal stature), and normalization of hematological and biochemical parameters.
Furthermore, treatment with a gluten-free diet reverses the decrease in bone mineralization and the risk for fractures. Symptomatic children treated with a gluten-free diet also improve their sense of physical and psychological well-being.