SHOCK
DR. AHMED KHAN
Definition
Shock: A state of inadequate tissue perfusion of oxygen and nutrients to maintain normal tissue and cellular function.
A disparity between blood volume and vascular capacity, which can be caused by:
- Reduction in blood volume
- Increase in the vascular bed
- By both the above mechanisms.
Inadequate peripheral perfusion:
- → to failure of tissue oxygenation
- → Lead to anaerobic metabolism
- → tissue acidosis & cellular dysfunction
- → multi organ dysfunction(MOF) & death.
Systemic inflammatory response syndrome SIRS
A clinical response to a nonspecific insult of either infectious or non infectious origin. SIRS is defined as 2 or more of the following variables:
- Fever of more than 38°C (100.4°F) or less than 36°C (96.8°F)
- Heart rate of more than 90 beats per minute
- Respiratory rate of more than 20 breaths per minute or arterial carbon dioxide tension (PaCO2) of less than 32 mm Hg (N= 38-42)
- Abnormal white blood cell count (>12,000/µL or < 4,000/µL or >10% immature [band] forms)
Multiple Organ Dysfunction Syndrome (MODS)
Progressive distant organ failure (initially uninvolved) following severe infectious or noninfectious insults (severe burn, multiple trauma, shock, acute pancreatitis)
Types of Shock & Prognosis
- Hypovolemic Shock (readily treatable - well response medical therapy)
- Septic Shock (mortality rate up to 75%)
- Cardiogenic Shock extensive myocardial infraction : (mortality up to 75%)
- Anaphylactic Shock (readily treatable - well response medical therapy)
- Neurogenic Shock (readily treatable - well response medical therapy)
Pathogenesis:
Series of pathophysiological changes aimed at protecting the organism and preserving its vital functions as follows:
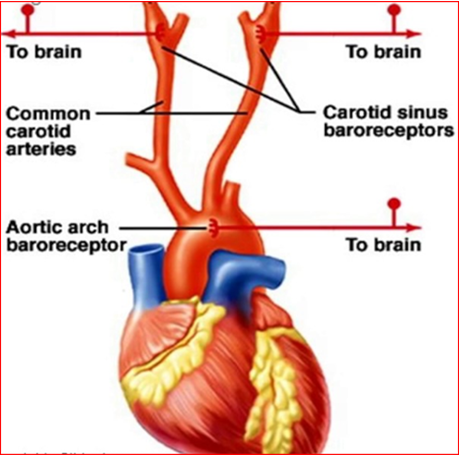
I. Sympatho-adrenal response: A) The fall in blood pressure due to inadequate cardiac output is sensed by the stretch receptors located in the aortic arch and carotid sinus (Baroreceptors) with the consequent sympathoadrenal stimulation.
B) The Vasomotor Center activity is increased resulting in: an enhanced peripheral resistance to maintain the blood pressure .
C) The heart rate increases to restore the cardiac output.
D)The increased “sympathetic cardiac activity” :
-
increases the heart rate and
-
also increases the strength of myocardial contraction.
-
The arteriolar constriction is selective.
The blood flow to skin, skeletal muscle, salivary glands, intestines, liver, and kidneys is reduced. The skin becomes cold.
Salivary secretion stops and mouth becomes dry, intestines manifest impaired digestion and water absorption.
How ever, blood flow to essential organs like brain, heart, diaphragm and intercostal muscles is maintained.
II. Neuroendocrine response: In case of apparent hypovolemia, there will be increased secretion of ACTH, growth hormone, glucagon, ADH, catecholamines and cortisol. ---- ADH helps in the reabsorption of H2O from the distal renal tubules.
Activation of the renin angiotensin system Due to decreased renal blood flow there is secretion of renin from the juxtaglomerular apparatus which leads to the formation of angiotensin, a potent vasoconstrictor which stimulates aldosterone secretion resulting in Na and H2O retention and increase of blood volume.
Glucagon stimulates gluconeogenesis and glycogenolysis thereby causing hyperglycaemia and increased osmolarity which helps in the fluid shift from the interstitium to the intravascular compartment.
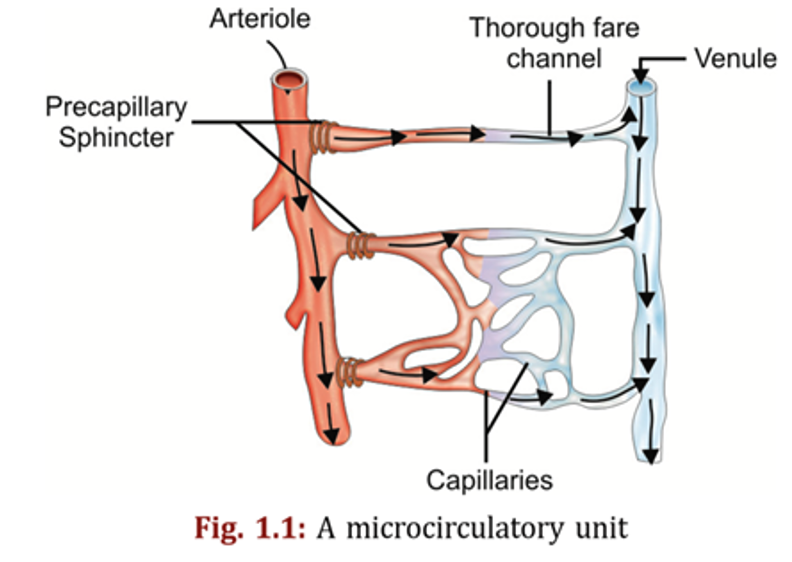
III. Microcirculatory Changes Due to intense sympathoadrenal and neuroendocrine response following hypovolemia there will be selective diversion of blood flow through meta-arteriolar shunt or thorough channels as closure of pre-and post- capillary sphincters occur.
In the irreversible phase of shock, there is relaxation of the precapillary sphincters while postcapillary sphincters remain constricted and blood gets sequestrated in the microcirculatory unit.
IV. Cellular Changes: 1- The cellular changes are due to ischemia:
-
Lack of oxygen and accumulation of waste products cause cell membrane dysfunction and metabolic acidosis
(Hypoxia of kidney, renal function is impaired → blood levels of acids rise, like lactate, pyruvate, phosphate & sulfate → causing metabolic acidosis)
2- Na and H2O enter the cell and K leaves it: which results in cellular swelling.
3- Mitochondrial dysfunction occurs in prolonged shock which will cause diminished ATP production.
4- There is also lysosomal disruption with resultant release of lysosomal enzymes and intracellular autodigestion occurs.
5- Widespread cellular damage may lead to multiorgan dysfunction syndrome (MODS).
Learning objectives (ILOs)
At the end of this presentation students will be able to describe:
- Definition & Types of shock
- Pathophysiology of different types of shock
- Clinical features & management of different shock.
BOOK REFERENCE
PRINCIPLES AND PRACTICE OF SURGERY 6th edition: PAGE NO: 17-26