Nephrotic Syndrome
Dr. Mansour ALQurashi
Definition
Manifestation of glomerular disease characterized by nephrotic range proteinuria and a triad of clinical findings associated with large urinary losses of protein:
- Hypoalbuminaemia
- Edema
- Hyperlipidemia
Nephrotic range proteinuria:
- Protein excretion of > 40 mg/m²/hr on a 24-hour collection
- First morning protein/creatinine ratio of > 2
Demographic Factors
- Incidence: 2 – 7 cases per 100,000 children per year.
- Most prevalent in children between the ages 1.5-6 years.
- Affects more boys than girls (2:1 ratio).
- MCNS typically presents between 2 and 8 years of age (peak, 3 years).
Etiology
Idiopathic or Primary
- Minimal Change Disease (>80%)
Genetic
- Finnish type Congenital Nephrotic Syndrome
- Alport Syndrome
Secondary
- Infectious: Hepatitis (B, C), HIV-1, Malaria, Syphilis, Toxoplasmosis
- Inflammatory: Glomerulonephritis
- Immunological: Lupus nephritis, Bee sting, Food allergens
- Neoplastic: Lymphoma, Leukemia
- Traumatic (Drug induced): Penicillamine, Gold, NSAIDS, Pamidronate, Mercury, Lithium
Pathophysiology
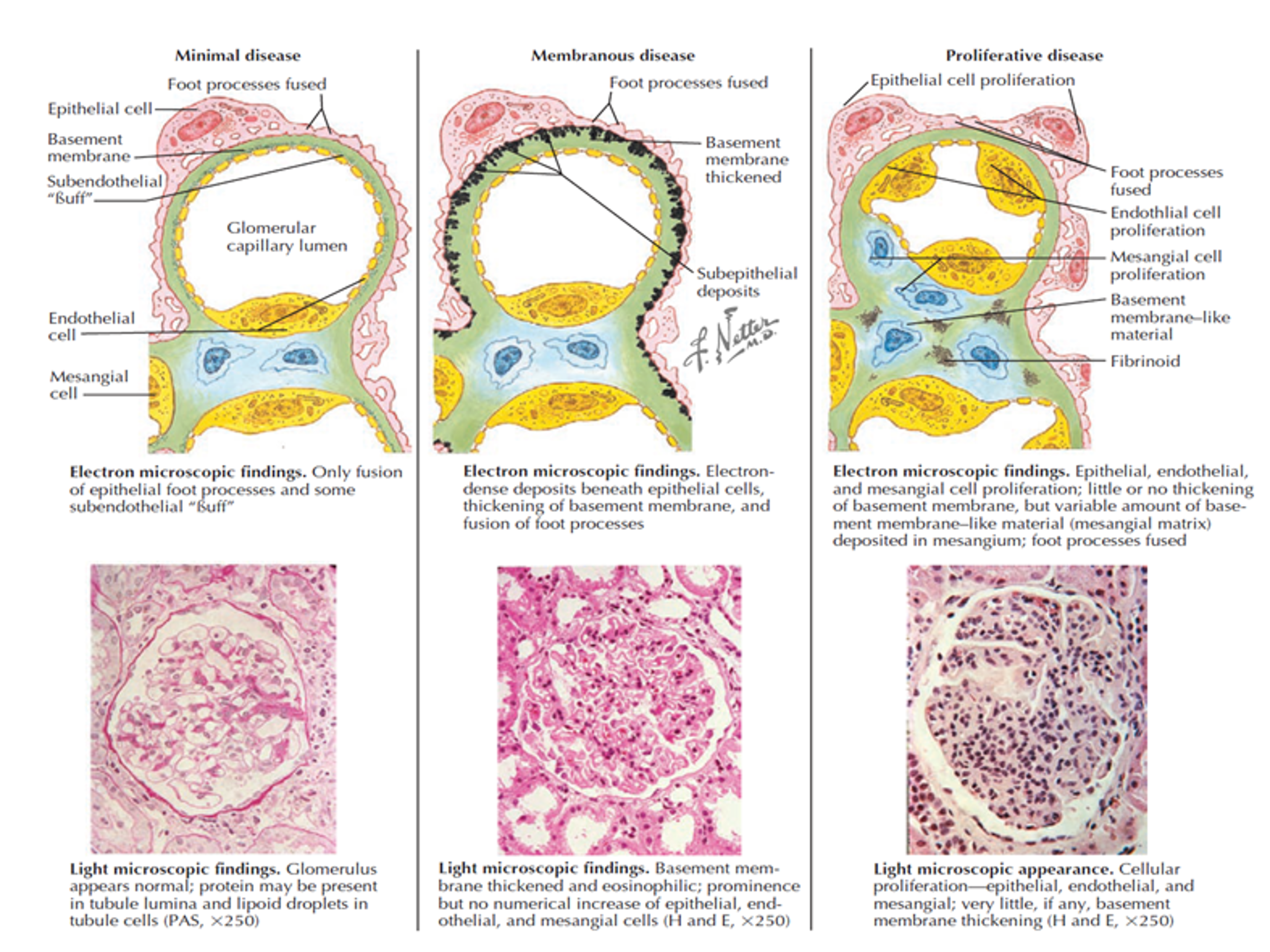
| Cause | Light microscopy | Immunofluorescence | Electron Microscopy |
|---|---|---|---|
| Minimal Change Nephrotic Syndrome | Normal | Negative | Foot process fusion |
| Focal Segmental Glomerulosclerosis | Focal sclerotic lesions | IgM, C3 in lesions | Foot process fusion |
| Membranoproliferative Glomerulonephritis | Type I | ||
| Thickened GBM, proliferation | Granular IgG, C3 | Mesangial and subendothelial deposits | |
| Type II | |||
| Lobulation | C3 only | Dense deposits |
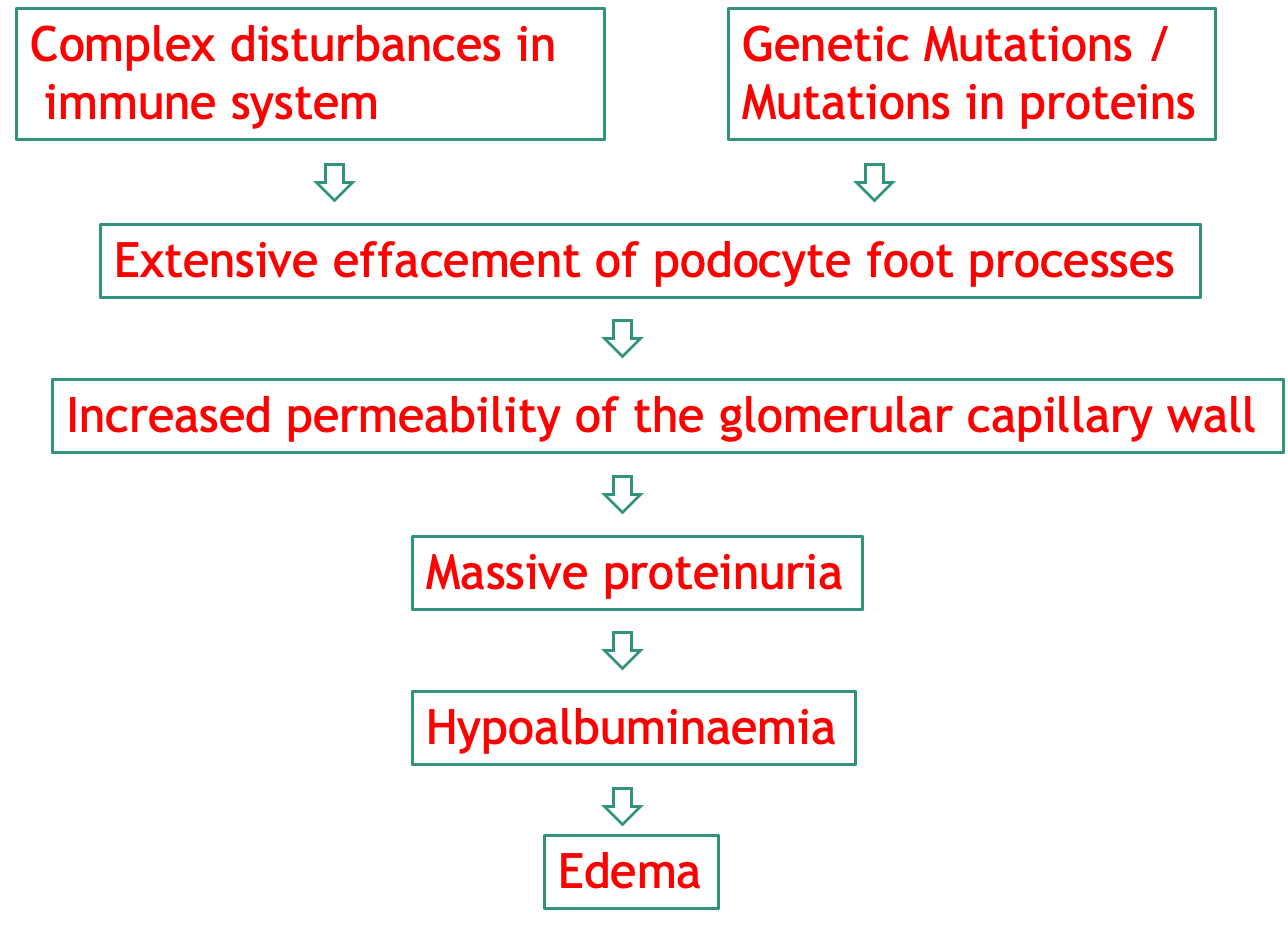
Complex Disturbances
- Immune system
- Genetic Mutations / Mutations in proteins
- Extensive effacement of podocyte foot processes
- Increased permeability of the glomerular capillary wall
- Massive proteinuria
- Hypoalbuminaemia
- Edema
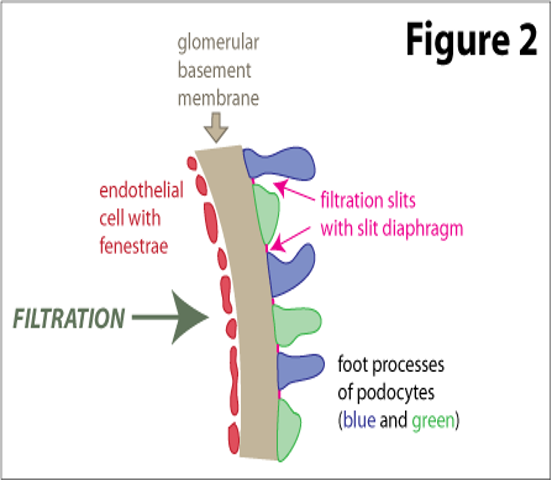
Filtration Barrier at the Glomerulus
3 Layers
- Capillary endothelium of glomerulus
- Basement membrane of glomerulus
- Visceral epithelium of Bowman’s capsule (podocytes with foot processes)
Idiopathic
-
Minimal Change Disease (>80%)
-
IgA Nephropathy (uncommon)
-
About 20% to 30% of nephrotic syndrome in adolescence is MCNS.
-
FSGS occurs at a median of 6 years of age and is more common in adolescents than in younger children.z
-
IgA nephropathy most common in the second and third decades of life.Z
| CLINICAL FEATURES | Minimal Change Nephrotic Syndrome | Focal Segmental Glomerulosclerosis | Membranoproliferative Glomerulonephritis (Low C3-70%) |
|---|---|---|---|
| Age (yr) | 2 - 6 | 2 - 10 | 2 - 18 |
| Sex (M : F) | 2 : 1 | 1.3 : 1 | 1 : 1 |
| Nephrotic Syndrome | 100 % | 90 % | 60 % |
| Asymptomatic proteinuria | 0 | 10 % | 20 % |
| Hematuria | 10 - 20 % | 60 - 80 % | 20 % |
| Hypertension | 10 % | 20 % early | 80% |
| Rate of progression to renal failure | Non progressive | 10 yrs | 50 % in 10 - 20 yrs |
| Associated Conditions | Usually none | None | Thrombotic microangiopathies, SLE, Celiac, Hepatitis B, C, Endocarditis |
Clinical Features
Edema
- Main presenting feature (95%) with rapid or insidious onset.
- Mild pitting edema starts with peri-orbital puffiness (more pronounced in the morning) and lower extremities.
- Progression to generalized edema, ascites, pleural effusion, genital edema, and sacral edema.
- Pleural effusions are generally asymptomatic but may cause respiratory compromise if large.
- Ascites may lead to umbilical or inguinal hernias and serious complications like spontaneous bacterial peritonitis (SBP).
- Bowel wall edema may produce diminished appetite, abdominal colic, and diarrhea, leading to protein-losing enteropathy if chronic.
Blood Pressure
- Hypertension (12%): Resulting from fluid overload or primary kidney disease (unusual in minimal change disease), suggestive of another underlying pathology, such as FSGS or glomerulonephritis.
- Careful assessment of volume status is critical. The child with anasarca may be profoundly intravascularly volume depleted.
- Children with nephrotic syndrome are at increased risk of cardiovascular collapse in the setting of ongoing volume loss, particularly if compounded by adrenal insufficiency caused by long-term steroid administration.
- Hypotension and signs of shock: Can be present in children presenting with sepsis.
Urine
- Nephrotic patients are often oliguric, and the urine appears concentrated and foamy.
- Nephrotic-range proteinuria
- Specific gravity may be artificially high secondary to the proteinuria.
- Microscopic hematuria may be noted.
- Gross or macroscopic hematuria is rare and may indicate a complication such as infection or renal vein thrombosis.
Other Signs and Symptoms
- Viral respiratory tract infection: A history of a respiratory tract infection immediately // soar throat - preceding the onset of nephrotic syndrome is frequent on initial presentation and on subsequent relapses.
- Allergy: Approximately 30% of children with nephrotic syndrome have a history of allergy.
- Symptoms of infection: May include fever, lethargy, irritability, or abdominal pain due to sepsis or peritonitis.
- Respiratory distress: Due to either massive ascites and thoracic compression or frank pulmonary edema and effusions, or both.
- Seizure: Caused by cerebral thrombosis (urinary losses of antithrombotic proteins, increased synthesis of prothrombotic factors).
- Anorexia, pallor, Muehrcke’s lines (double white lines that run across the fingernails horizontally).
Differential Diagnosis
Any cause for edema
- Protein losing enteropathy.
- Hepatic failure.
- Heart failure.
- Acute/Chronic Glomerulonephritis.
- Protein Malnutrition.
DiagnosisZ
-
Urinalysis: 3+ to 4+ proteinuria
- Spot UPC ratio > 2.0
- UPE > 40 mg/m²/hr
- Renal Function: Azotemia (↑ BUN), Creatinine – normal or elevated
-
LFT:
- ALT, AST. Serum albumin - < 2.5 gm/dl
- Serum Cholesterol/TGA levels: Elevated
- Serum Complement levels (C3, C4): C3 Normal or low.
-
CBC & Blood picture:
- Hemoconcentration (↑ hemoglobin). Thrombocytosis
-
Platelet hyperaggregability, ↑ V, VIII, and fibrinogen with blood hyperviscosity.
-
↑↑ ESR
-
Electrolytes:
- Hyponatremia (Na: 120 -130 mEq/L)
- ↓ Serum calcium (pseudohypocalcemia, true hypocalcemia)
-
Antistreptolysin O titre
-
Chest X-ray, Kidney ultrasonography, and tuberculin test.
-
ANA, Anti–double-stranded DNA.
-
Hepatitis B surface antigen/Hepatitis C antibodies.
Indications for Renal Biopsy:
- Age below 12 months or older than 13 years.
- Gross or persistent microscopic hematuria or RBC casts
- Low blood C3
- Significant hypertension or pulmonary edema.
- Impaired renal function
- Failure of steroid therapy (steroid resistance).
- Extrarenal or constitutional symptoms, such as weight loss, recurrent fever, rash, or arthritis
Management
Supportive Therapy
- High protein diet.
- Salt moderation
- Treatment of infections
- If significant edema – diuretics: Furosemide, spironolactone, and metolazone, with or without 25% IV albumin
Corticosteroid Therapy
- Prednisolone or prednisone (2mg/kg per day for 6 weeks followed by 1.5 mg/kg single morning dose on alternate days for 6 weeks), after which the dose is gradually tapered, with a minimum total duration of treatment of 12 weeks.
- The first morning urine sample should be monitored daily by urine dip.
- Remission is defined as at least 3 consecutive days of negative to trace urine protein.
- Approximately 95% of children with MCNS compared with 20% to 25% of those with FSGS go into remission after 8 weeks of prednisone.Z
Management of Relapse
Relapse
- Defined by 3 consecutive days of 2+ or greater urine protein.
- Infrequent Relapsers: 3 or less relapses per year
- Frequent Relapsers: 4 or more relapses per year
Steroid Therapy
-
Steroid Dependent: Relapse following dose reduction or discontinuation (within 2 weeks).
-
Steroid Resistant: Partial or no response to initial treatment (lack of remission by 8 weeks of standard steroid therapy).
Parent Education
-
Symptomatic therapy for infections in case of low-grade proteinuria
-
Persistent proteinuria (3 - 4+):
- Prednisolone (2mg/kg/day until protein is negative for 3 days)
- 1.5 mg/kg on alternate days for 4 weeks, after which the dose is gradually tapered.
Frequent Relapses
- Alternate Day Prednisolone
- Steroid Sparing Agents:
- Levamisole (2 – 2.5 mg/kg)
- Cyclophosphamide (2 – 2.5 mg/kg/day)
- Mycophenolate Mofetil (20 – 25 mg/kg/day)
- Cyclosporin (4 – 5 mg/kg/day)
- Tacrolimus (0.1 – 0.2 mg/kg/day)
- Rituximab (375mg/m² IV once a week)