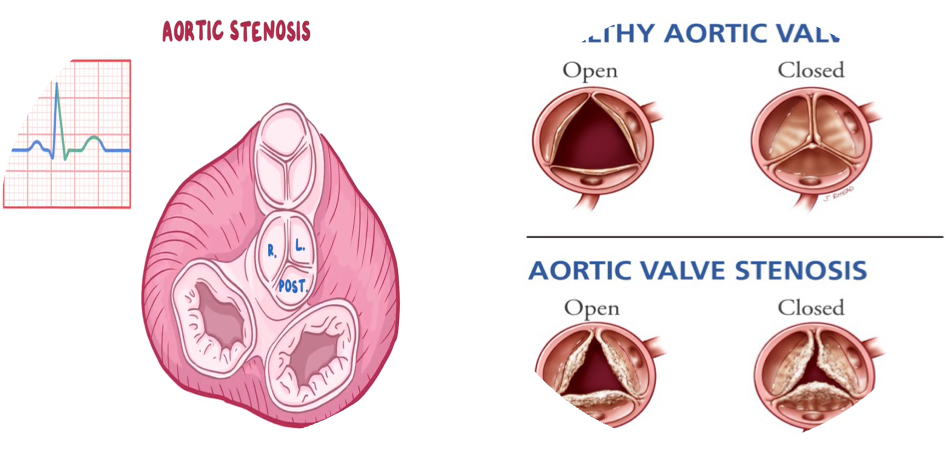
Normal Aortic Valve
Three cusps, crescent-shaped
- 3 commissures
- 3 sinuses
- Supported by fibrous annulus
- 3.0 to 4.0 cm2
Symptoms: valve area: 1/4th of normal
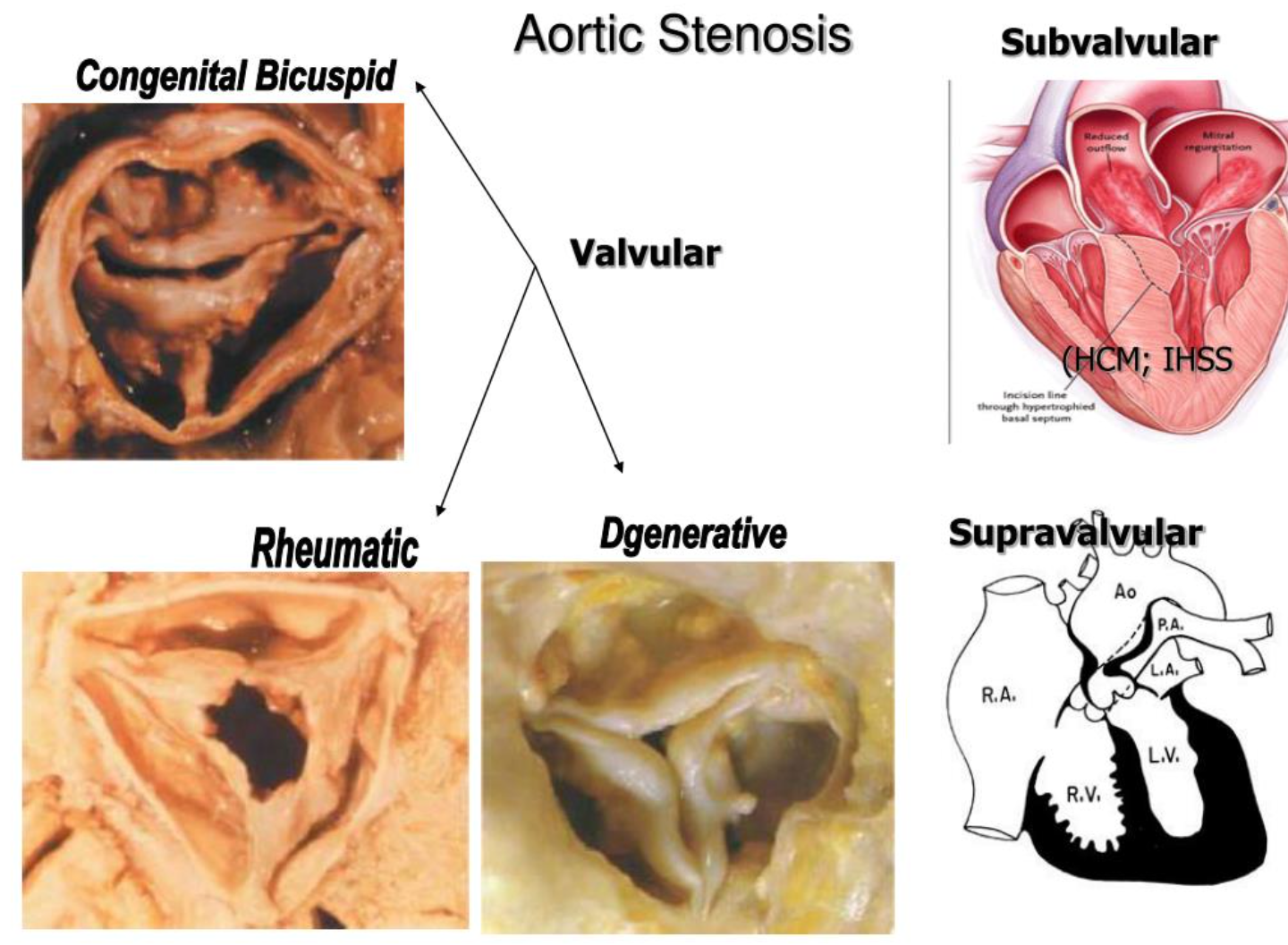
Types:
- Supravalvular: Williams Syndrome AD
- Subvalvular
- Valvular
Epidemiology
- Most common VHD in industrialized countries
- Frequently associated with AR
- Prevalence: ↑ with age
Prognosis
- Asymptomatic with normal LVEF: progression to symptoms or LV dysfunction at a rate of < 6% /yr
- Asymptomatic patients with ↓ EF: progression to symptoms at a rate of > 25% per year
- Untreated: die 2-3 years if no surgical intervention.
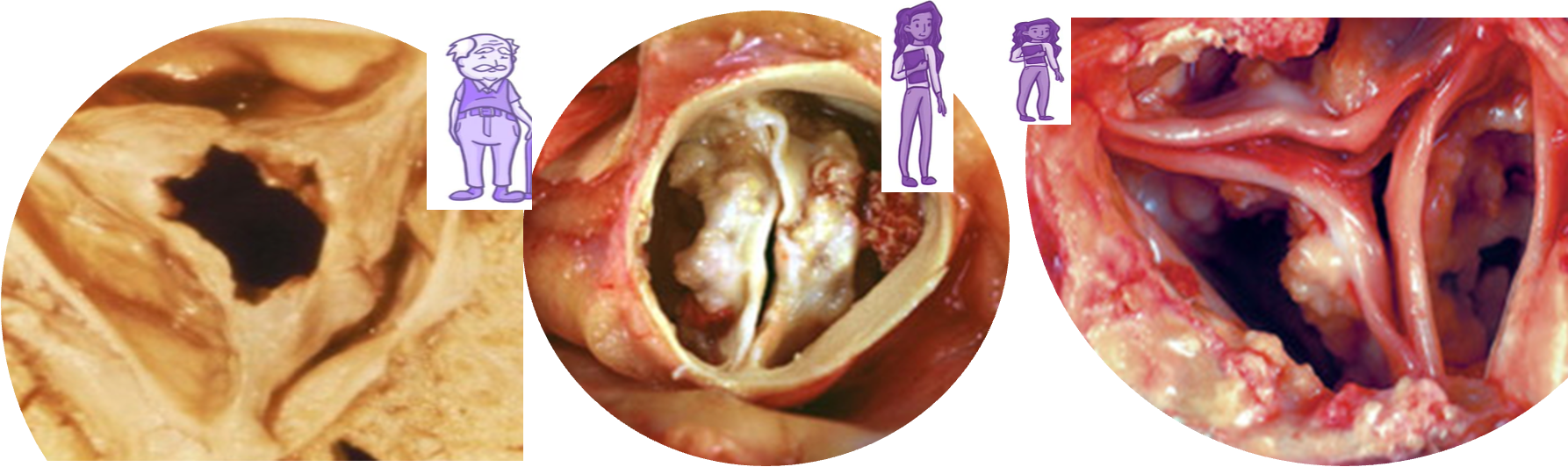
Etiology
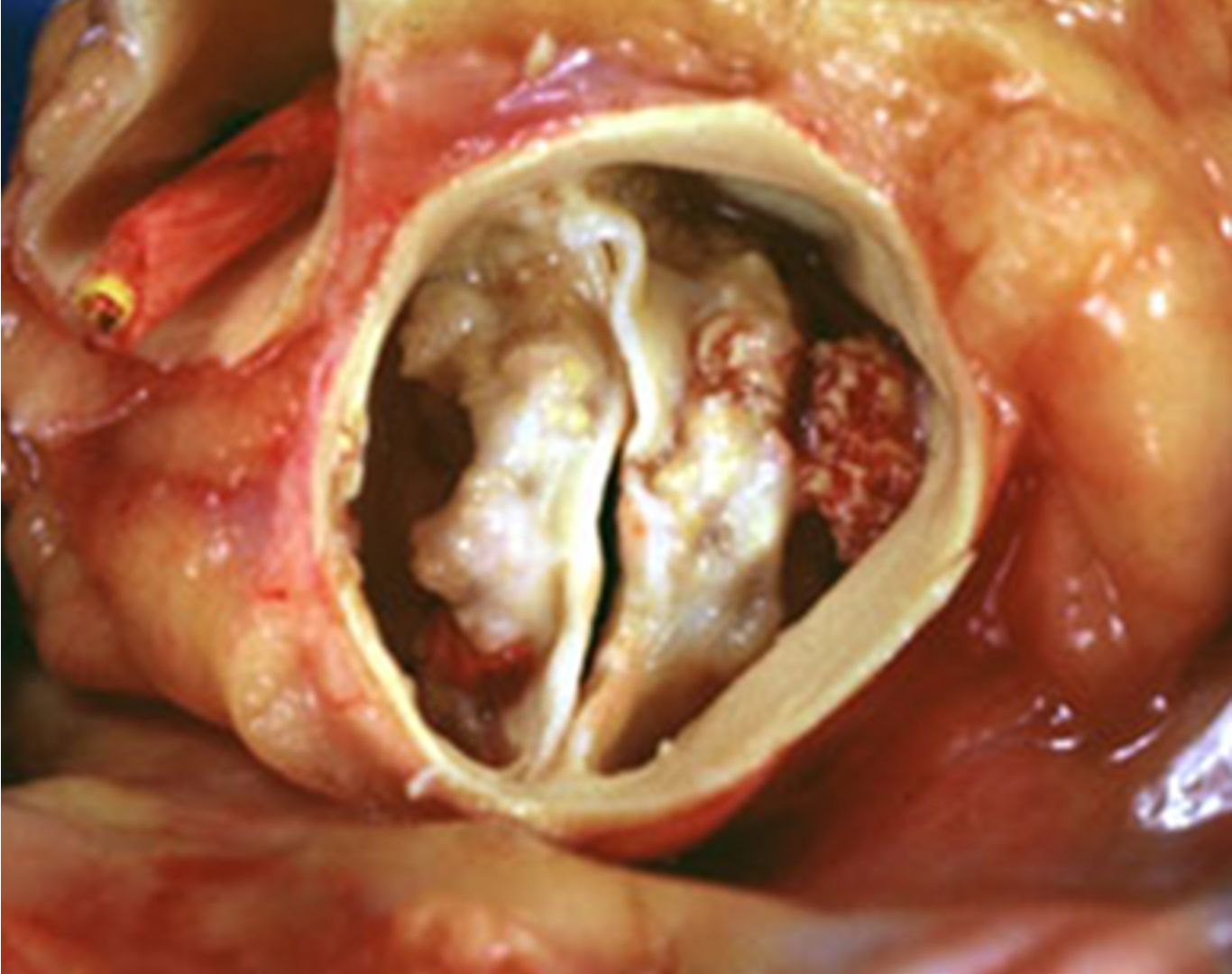
- Aortic valve sclerosis: C st. Normal tips. ↑ with age ~ atherosclerosis
- Bicuspid aortic valve (BAV): Fusion leaflets in utero. C: males (3:1). Dystrophic calcification and degeneration. Associated with A coarctation, root dilation & A dissection. Symptoms of AS: earlier than in regular aortic valve calcification.
- Rheumatic fever: C in lower-income countries. Stenosis is caused by commissural fusion. 2nd turbulent flow, calcification of tips.
Pathophysiology
Progressive narrowing: ↓ flow across the valve. ↑ LV pressure, LV hypertrophy (Stroke volume), and ↑ end-diastolic pressures and non-compliant LV.
Symptoms
- Syncope: ↓ cerebral perfusion; triggered by cardiac arrhythmias or complete heart block.
- Angina: High end-diastolic pressures reduce coronary artery perfusion.
- Dyspnea: On exertion due to heart failure (systolic and diastolic).
forth sputum, alveoli, effusion
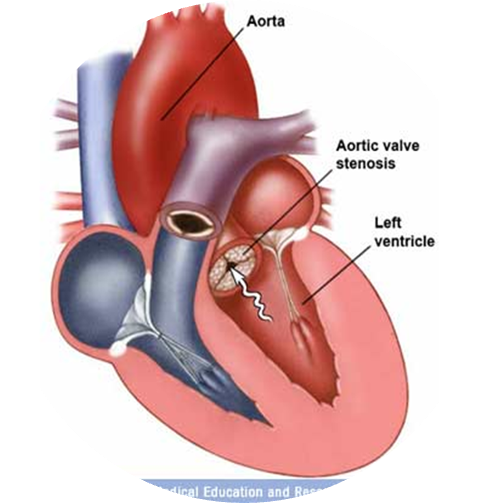
Narrowed opening area of the aortic valve during systole → obstruction of blood flow from the left ventricle (LV) → increased LV pressure → left ventricular concentric hypertrophy, which leads to: Increased LV oxygen demand. Impaired ventricular filling during diastole → left heart failure. Reduced coronary flow reserve. Initially, cardiac output (CO) can be maintained. Later, the decreased distensibility of the left ventricle reduces cardiac output and may then cause backflow into the pulmonary veins and capillaries → higher afterload (pulmonic pressure) on the right heart → right heart failure.
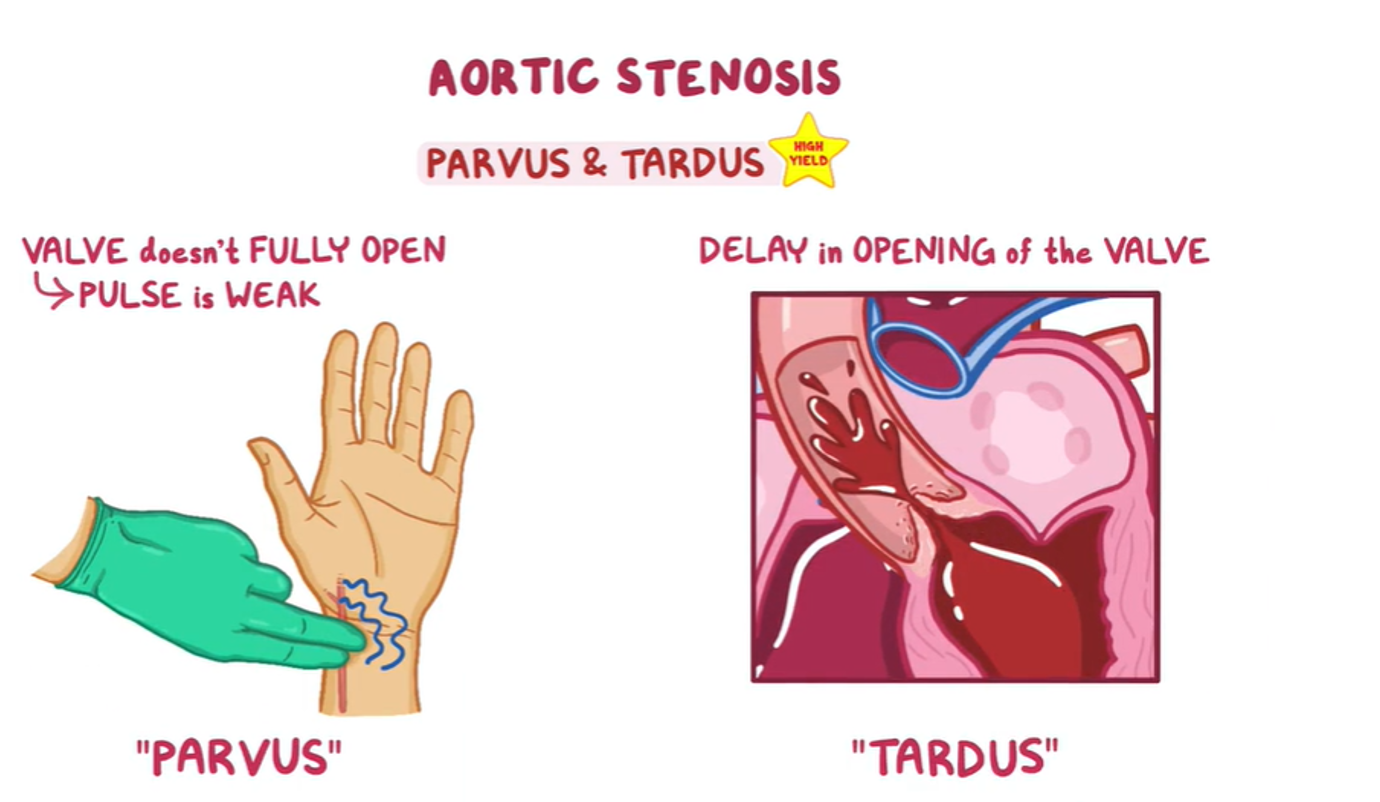
Examination Findings Z
- Weak & delayed distal pulse & decreased pulse amplitude.
- Narrow pulse pressure.
- Systolic thrill over the Aortic A.
- Apex: heaving.
On auscultation:
- S2: soft and reversed-split.
- S4 gallop due to atrial contraction.
- Crescendo–decrescendo ejection systolic murmur radiating to both carotids (best heard over the aortic area).
Clinical Features
- Loudness is not related to the severity.
- Triad of ‘SAD’ symptoms on exertion: Syncope, Angina, Dyspnea.
- Sudden death.
Investigations
First-line: non-invasive gold standard:
-
Echocardiography and Doppler: A narrow AV is diagnostic; mean pressure gradient and jet velocity across the valve.
-
ECG:
- Left ventricular hypertrophy with strain pattern, left axis deviation.
- CXR:
- Cardiomegaly, calcified aorta and aortic valve, and post-stenotic aortic dilatation.
Second-line:
- Cardiac MRI: Assess thoracic aorta: aneurysm, dissection, or coarctation.
- Cardiac catheterization: Accurate, before surgery.
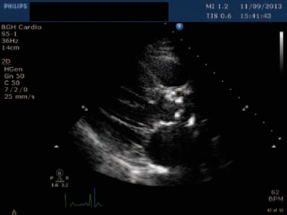 Calcification and narrowing of the AV. Increased mean aortic pressure gradient and transvalvular velocity. Signs of cardiac remodeling, e.g., concentric hypertrophy.
Calcification and narrowing of the AV. Increased mean aortic pressure gradient and transvalvular velocity. Signs of cardiac remodeling, e.g., concentric hypertrophy.
Severity:
- Mild disease is a gradient < 30 mm Hg.
- Moderate disease: 30–70 mm Hg.
- Severe disease > 70 mm Hg.
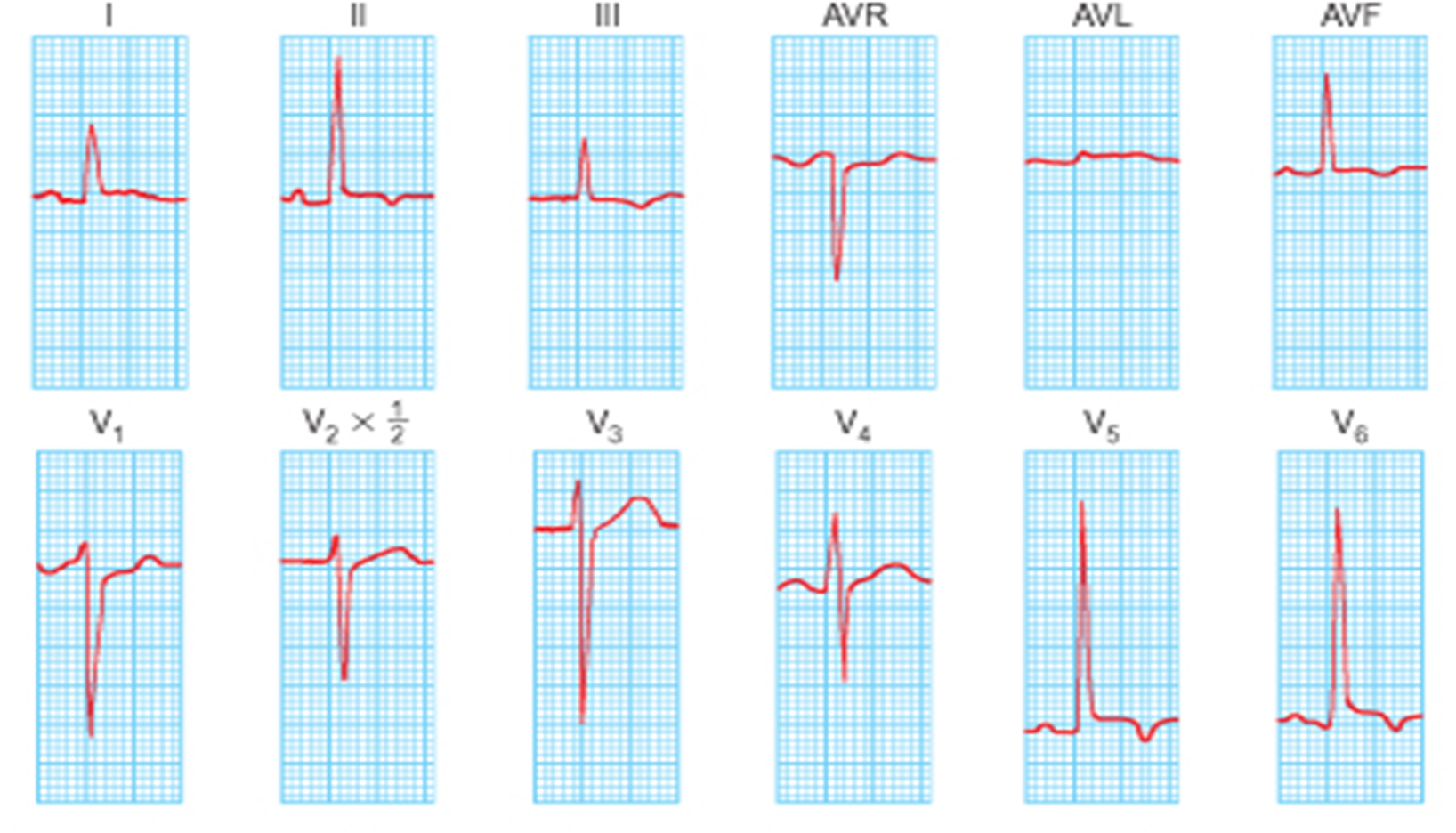 V2 + V6 Ventricular hypertrophy squares cc
V2 + V6 Ventricular hypertrophy squares cc
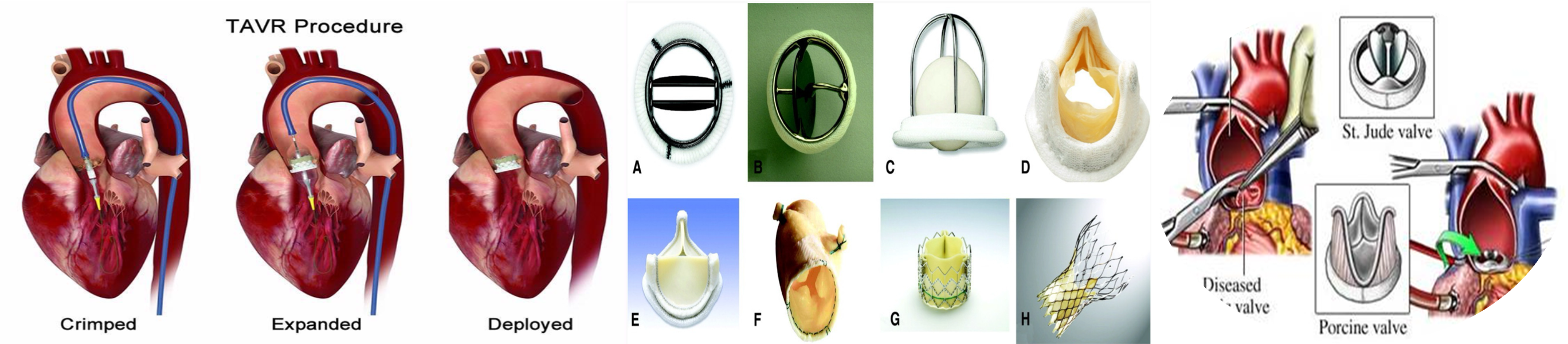 thrombus potentiating metalic valve, anticouagulant for life exception of prosthetics in beginning
thrombus potentiating metalic valve, anticouagulant for life exception of prosthetics in beginning
Symptoms are a good index of severity
Symptomatic: Surgical therapy Aortic valve replacement (AVR): effective either with Bioprosthetic or Mechanical AVR Two approaches: 1. Surgical AVR: low surgical risk. 2. Transcatheter AVR: high surgical risk or contraindication
Medical therapy (Treat symptoms)
- Anticoagulants: AF or mechanical prosthesis
- Vasodilators are relatively contraindicated in severe AS
Balloon valvuloplasty: children with no aortic valve calcification
Asymptomatic: Regular assessment:
- symptoms and echocardiography every 6–12 months to monitor
Surgical intervention:
- Severe AS symptoms with LVEF of <50%.
- undergoing cardiac surgery
Balloon valvuloplasty: children with no aortic valve calcification
Aortic valve stenosis is a progressive condition, and definitive management requires valve replacement.
- Urgency of valve repair/replacement depends on staging.
- Symptomatic and/or severe AS: aortic valve replacement usually indicated.
Afterload reduction (e.g., with vasodilators or diuretics) in severe AS may reduce cardiac output enough to compromise systemic and myocardial perfusion. Careful titration is recommended with specialist guidance.
- Peak velocity through the aortic valve >5.5 m/s.
- Systolic pulmonary artery pressure >60 mmHg.
- Rapid increase in velocity through the valve at >0.3 m/s/year.
Hypertension:
- Follow standard hypertension guidelines; medication should be carefully titrated to avoid hypotension.
- ACE-inhibitors may be beneficial in the prevention of cardiac remodeling.
Case Study 1
A 75-year-old hypertensive man presented 20 minutes after he suddenly lost consciousness. He has had episodes of mild chest pain and abdominal discomfort for the past 2 months. Vital signs: pulse 89/min BP 110/88 mm Hg. Examination shows a grade 3/6 late systolic murmur at the right sternal border that radiates to the carotids. There is no swelling or erythema of the lower extremities. Neurologic examination shows no focal findings. Which of the following is the most likely cause of this patient’s symptoms?
- Rupture of the chordae tendineae
- Fibrosis of the sinus node
- Asymmetric septal hypertrophy
- Calcification of the aortic valve
- Embolus in the pulmonary artery
Case Study 2
A 75-year-old man presented with an episode of syncope two days ago. The patient was working in his garden when he suddenly felt light-headed and lost consciousness for one minute. The patient endorses worsening shortness of breath and occasional chest pain during his usual morning walk for the past month. His temperature is 36.0°C (96.8°F), pulse is 75/min, and blood pressure is 138/87 mmHg. On physical examination, the lungs are clear to auscultation. Neurologic examination is normal. ECG: LVH. Cardiac auscultation will most likely reveal a murmur in which of the areas marked on the diagram below?
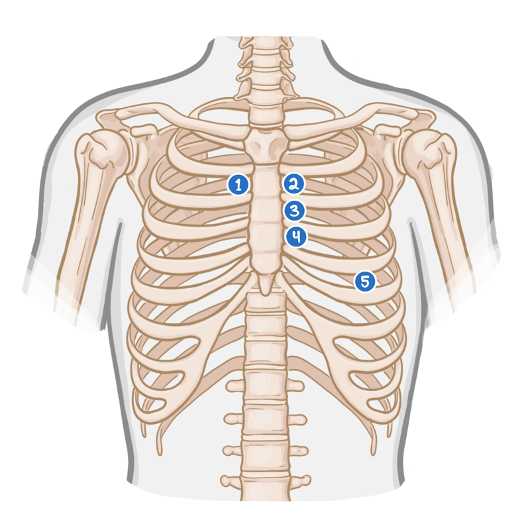
- Area 1: Crescendo-decrescendo systolic murmur.
- Area 4: Holosystolic murmur.
- Area 3: Systolic ejection murmur.
- Area 5: Opening snap followed by diastolic murmur.
- Area 2: Ejection murmur accompanied by a fixed split-second heart sound (S2).