Ophthalmology
Hypertensive retinopathy Y
-
Damage to the retina from high blood pressure
-
Duration increases risk
-
Worse with
- Diabetes
- high cholesterol
- smoking
- Malignant hypertension
-
A systolic blood pressure (SBP) mmHg and/or
-
A diastolic (DBP) .
-
Based on the average of two or more properly measured, seated BP readings.
-
On each of two or more office visits.
The Eyes Y
-
Retinopathy, retinal hemorrhages and impaired vision.
-
Vitreous hemorrhage, retinal detachment
-
Neuropathy of the nerves leading to extraoccular muscle paralysis and dysfunction
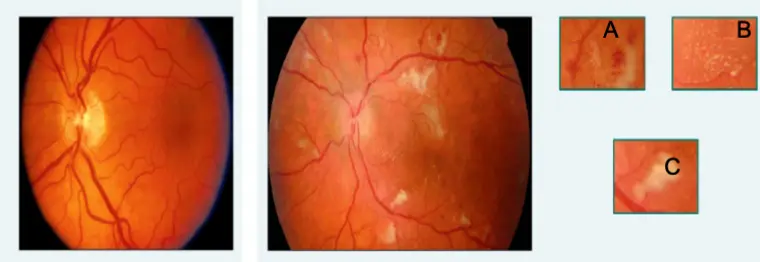
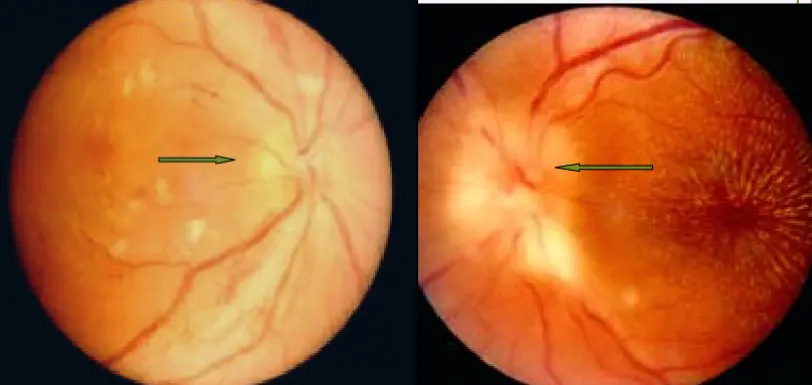
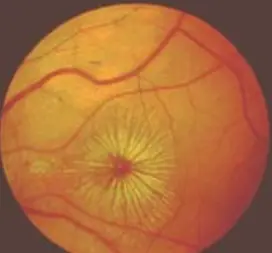
Normal Retina
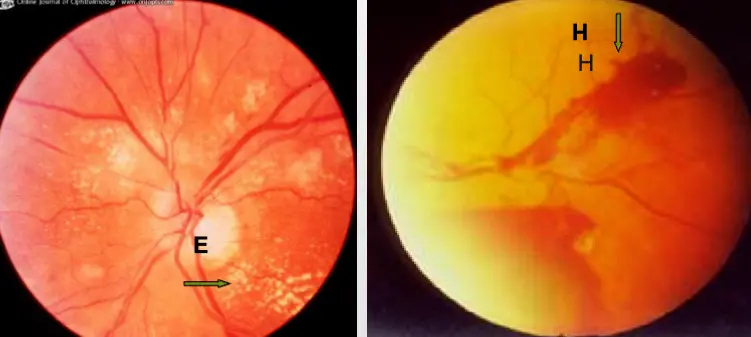
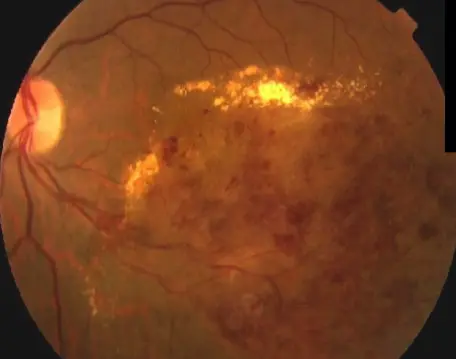
Hypertensive Retinopathy A: Hemorrhages B: Exudates (Fatty Deposits) C: Cotton Wool Spots (Micro Strokes)
Symptoms of Hypertensive retinopathy Z
-
Grade 1- no symptoms
-
Grade 2/3- blurring of vision/headache/diplopia
-
Grade 4- Optic nerve swelling gives blurred vision and field loss.
-
Patients often have poor renal function and are at risk of stroke and encephalopathy
Signs of Hypertensive Retinopathy
- CWS (Diast BP often )
- Flame shaped Haem.
From focal closure of retinal microvasculature/microinfarcts
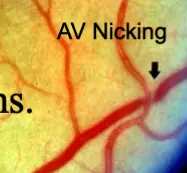
CWS + AV Nicking

Ophthalmoscopy findings
Hypertensive Retinopathy
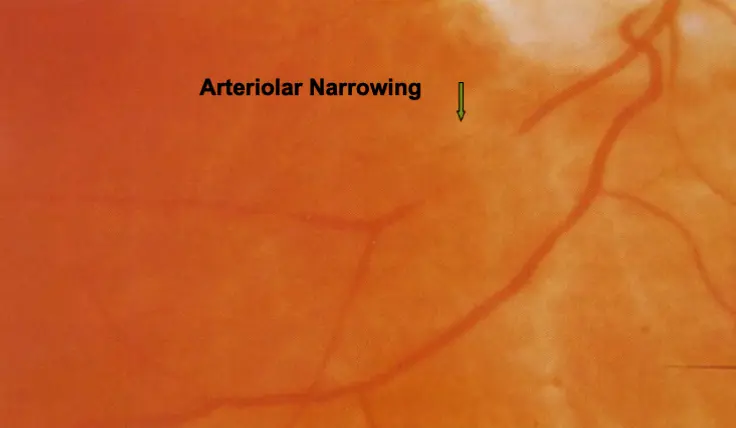
Stage I- Arteriolar Narrowing Z
Stage II- AV Nicking Z
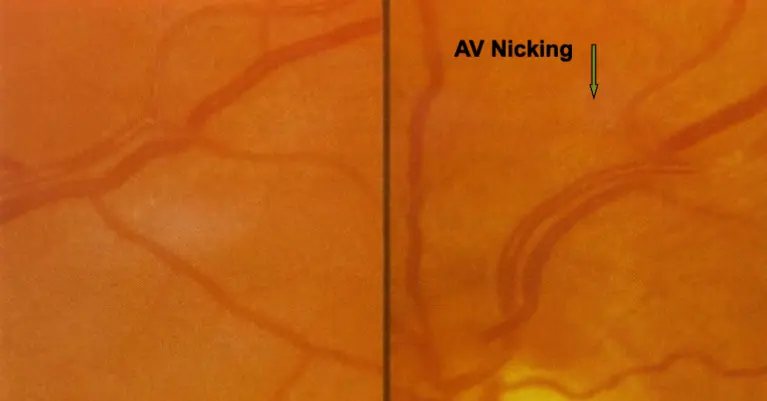
 Venous congestion, vneouartery
Venous congestion, vneouartery
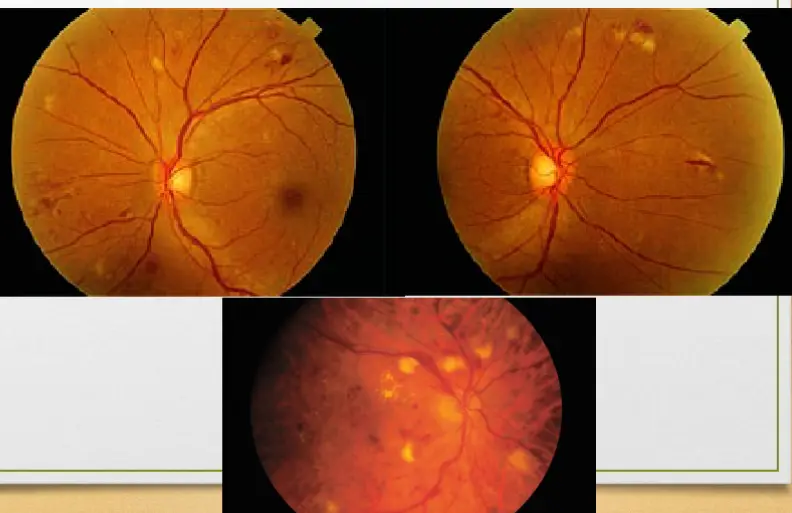
Stage III- Hemorrhages (H), Cotton Wool Spots and Exudats
Stage IV- Stage III+Papilledema
All previous stages has already happened - last stage
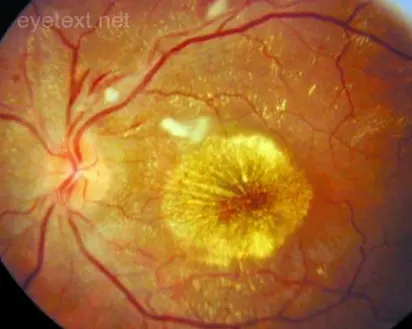
Hypertensive Retinopathy, Severe - REVERSIBLE Z
-
Rarely retinal/macular oedema
-
Disc oedema + severe macular oedema with macular star in extreme cases (malignant HTN, with BP on the range of )
-
Macular star may develop in weeks & resolve in months
-
Disc oedema may develop in days and resolve in weeks or months
-
 eclampsia - preeclampsia referral - retinal examination shows papilledema - it is in stage 4, treat hypertensions control
eclampsia - preeclampsia referral - retinal examination shows papilledema - it is in stage 4, treat hypertensions control
Arteriolosclerosis often coexist:
-Arteriolar narrowing, focal or diffuse -Arteriolar colour changes -AV crossing changes, e.g. nicking flame Haems. -Vessel sclerosis, threading
Treatment
- Lower blood pressure to below
Malignant hypertension
- Collagen vascular diseases
- Renal problems
- Eclampsia of Pregnancy
- Pheochromocytoma
Retinal Vein Occlusion
- Second most common vascular disease causing loss of vision
Pathophysiology
- thrombus formation
- disease of the vein wall
- external compression of the vein
- Retinal arteries and arterioles and their corresponding veins share a common adventitial sheath.
- Atherosclerosis and thickening of the arteriole compresses the vein, eventually causing occlusion.
Venous occlusion
Branch Retinal Vein Occl.
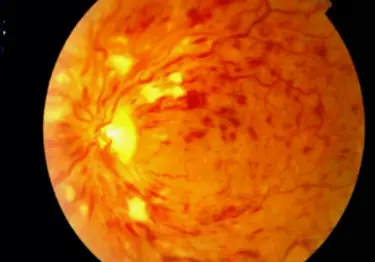
Central Retinal Vein Occl.
Etiology
- Advancing age - over over 65 yo
- under the age of 45
- Hypertension( of patients)
- Hyperlipidaemia, diabetes, smoking and obesity.
- Inflammatory diseases - sarcoidosis, Behçet’s syndrome.
- Hyperviscosity states- myeloma.
- Thrombophilic disorders (considered in yo
Therapeutics

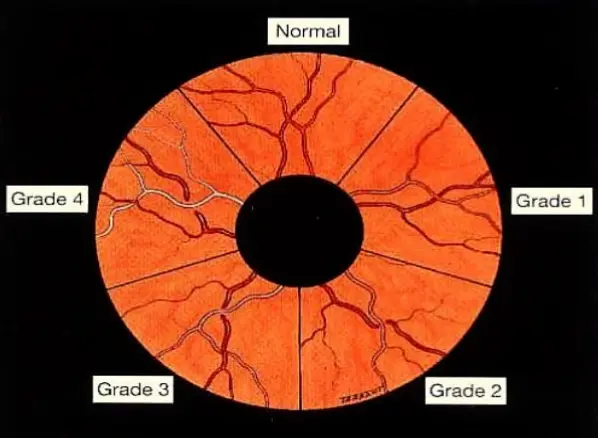
Classification system according to Keith-Wagener-Barker
| Grade | Findings | Symptoms |
|---|---|---|
| Grade I | Vessel diameter variation: arteriolar constriction and tortuosity | Usually asymptomatic |
| Grade II | Gunn sign and marked constriction of vessels and sclerosis of arterioles | Usually asymptomatic |
| Grade III | Cotton wool exudates, hard exudates, retinal hemorrhage, retinal edema, macular star formation | Decreased and/or blurred vision, headaches |
| Grade IV | Papilledema, optic atrophy | Decreased and/or blurred vision, headaches |
| X Gunn sign (Arteriovenous nicking) | ||
| A tapering of a retinal venule at the point where a retinal arteriole crosses the retinal venule; creates an hourglass shape. Associated with advanced hypertensive retinopathy. | ||
| Hard exudate | ||
| Accumulation of exudate from capillary leakage within the outer plexiform layer (Henle layer) and the inner nuclear layers of the retina. | ||
| Local treatment of retinopathy is not possible, therefore, systemic reduction of blood pressure is critical |
Bilateral papilledema- hypertensive emergency
 #X Bilateral papilledema
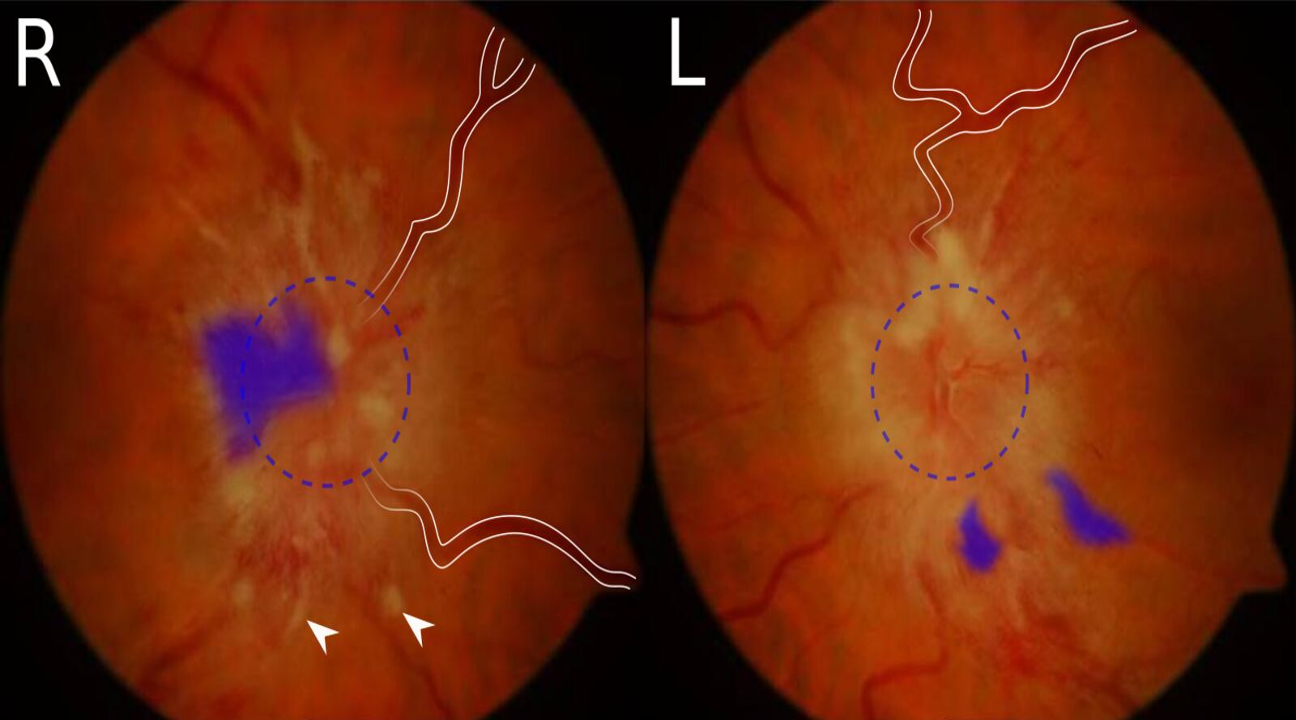
Fundus photography of right (R) and left (L) optic disc of the same patient:
The optic discs show severely blurred margins (dashed circle indicates supposed margin). The retinal veins are dilated and tortuous (examples marked by white lines). There are multiple peripapillary hemorrhages, which appear as flame-shaped hemorrhages (examples marked by blue overlay). Cotton wool spots are also present and appear as bright spots (examples marked by arrowheads).
These features are characteristic of papilledema. If present bilaterally, possible causes include cranial hypertension or hypertensive emergency.
Source: “Figure 1. in: A 43-year-old woman on triptorelin presenting with pseudotumor cerebri: a case report” by Uday Kumar Bhatt, Imran Haq, Venkata S. Avadhanam und Kim Bibby, Journal of Medical Case Reports, licensed under CC BY 2.0. The supplementary image with overlays of relevant areas was adapted from the image mentioned above (© AMBOSS).
#X Bilateral papilledema
Fundus photography of right (R) and left (L) optic disc of the same patient:
The optic discs show severely blurred margins (dashed circle indicates supposed margin). The retinal veins are dilated and tortuous (examples marked by white lines). There are multiple peripapillary hemorrhages, which appear as flame-shaped hemorrhages (examples marked by blue overlay). Cotton wool spots are also present and appear as bright spots (examples marked by arrowheads).
These features are characteristic of papilledema. If present bilaterally, possible causes include cranial hypertension or hypertensive emergency.
Source: “Figure 1. in: A 43-year-old woman on triptorelin presenting with pseudotumor cerebri: a case report” by Uday Kumar Bhatt, Imran Haq, Venkata S. Avadhanam und Kim Bibby, Journal of Medical Case Reports, licensed under CC BY 2.0. The supplementary image with overlays of relevant areas was adapted from the image mentioned above (© AMBOSS).