Approach to Cyanosis in Neonates
Dr. Mansour ALQurashi
Step 1: Cyanosis Detection
- Is your baby cyanotic? Yes or No
- Is cyanosis due to cardiac or pulmonary disease?
- Steps for diagnosis of cardiac disease in a neonate
Cyanosis & CXR
- CXR may suggest lung disease particularly if the findings are asymmetrical.
- If the changes are diffuse and symmetric, i.e., compatible with pulmonary edema or increased PVM, it is difficult to differentiate between primary lung disease or heart disease causing pulmonary edema, e.g., TAPVD with obstruction.
- PPH can coexist with lung disease and cause severe cyanosis.
Cyanosis and CO2 Retention
- CO2 retention is usually prominent with primary lung disease. Some severely cyanotic infants with cardiac disease can have marked hypercarbia.
- Absence of hypercarbia is suggestive of cardiac disease. Some severely cyanotic infants with pulmonary vascular disease have normal PCO2.
Cyanosis & Hyperoxia Test
- It is the response of the arterial PO2 to administration of 100% O2.
- If PO2 goes above 220 mmHg, the patient has lung disease.
- If PO2 is less than 100 mmHg, the patient is likely to have cardiac disease.
- The test is inconclusive if PO2 is between 100 and 220 mmHg.
- Transcutaneous O2 saturation is NOT an alternative to arterial PO2.
PDA Dependant Cardiac Lesions
- RVOT Obstruction:
- e.g., TA, PA, or Severe TOF +/- PA.
- They manifest with severe cyanosis when the pulmonary flow is compromised by a closing DA.
- LVOT Obstruction:
- e.g., HLHS, Critical AS, Hypoplastic AA, or severe Co A.
- They manifest with early CHF as their descending aorta flow is supplied by PDA.
- D-TGA:
- PDA is needed for proper mixing of pulmonary and systemic circulations.
Confirmatory Diagnostic Tools
- ECG
- Echocardiography with Doppler
- Diagnostic Cardiac Catheterization
Persistent Pulmonary Hypertension of the Newborn (PPHN)
- PPHN is defined as a delay in the normal postnatal decline in pulmonary vascular resistance resulting in associated shunting of de-oxygenated blood across to the systemic circulation, leading to arterial hypoxemia.
- PPHN (or persistence of the fetal circulation) occurs in approximately 1 in 1500 live births.
Primary PPHN
- Classical PPHN
- Idiopathic
- Hypoxemia develops in a baby with normal lungs.
- Breath sounds and CXR are usually normal.
Secondary PPHN
- PPHN secondary to lung disease.
- Meconium aspiration syndrome
- Congenital diaphragmatic hernia
- Group B streptococcal pneumonia
- Respiratory distress syndrome
- Sepsis
- Hypoplasia
Treatment of PPHN
Initial Therapies
- Treat metabolic derangements: correct acidosis, hypoglycemia, hypocalcemia
- Optimize lung recruitment: mechanical ventilation, high-frequency oscillatory ventilation, surfactant
- Optimize cardiac output and left ventricular function: vasopressors, inotropic agents
Pulmonary Vasodilators
- Inhaled nitric oxide
Other Therapies
- Phosphodiesterase Inhibitors (sildenafil)
- Inhaled prostacyclin analogs (iloprost, prostacyclin)
- Recombinant superoxide dismutase
Congenital Cyanotic Heart Disease
Cyanotic CHD with Decreased Pulmonary Blood Flow
- Pulmonary Atresia
- Tricuspid Atresia
- Critical Pulmonary Stenosis
- Ebstein’s Anomaly
- Tetralogy of Fallot
Cyanotic CHD with Increased Pulmonary Blood Flow
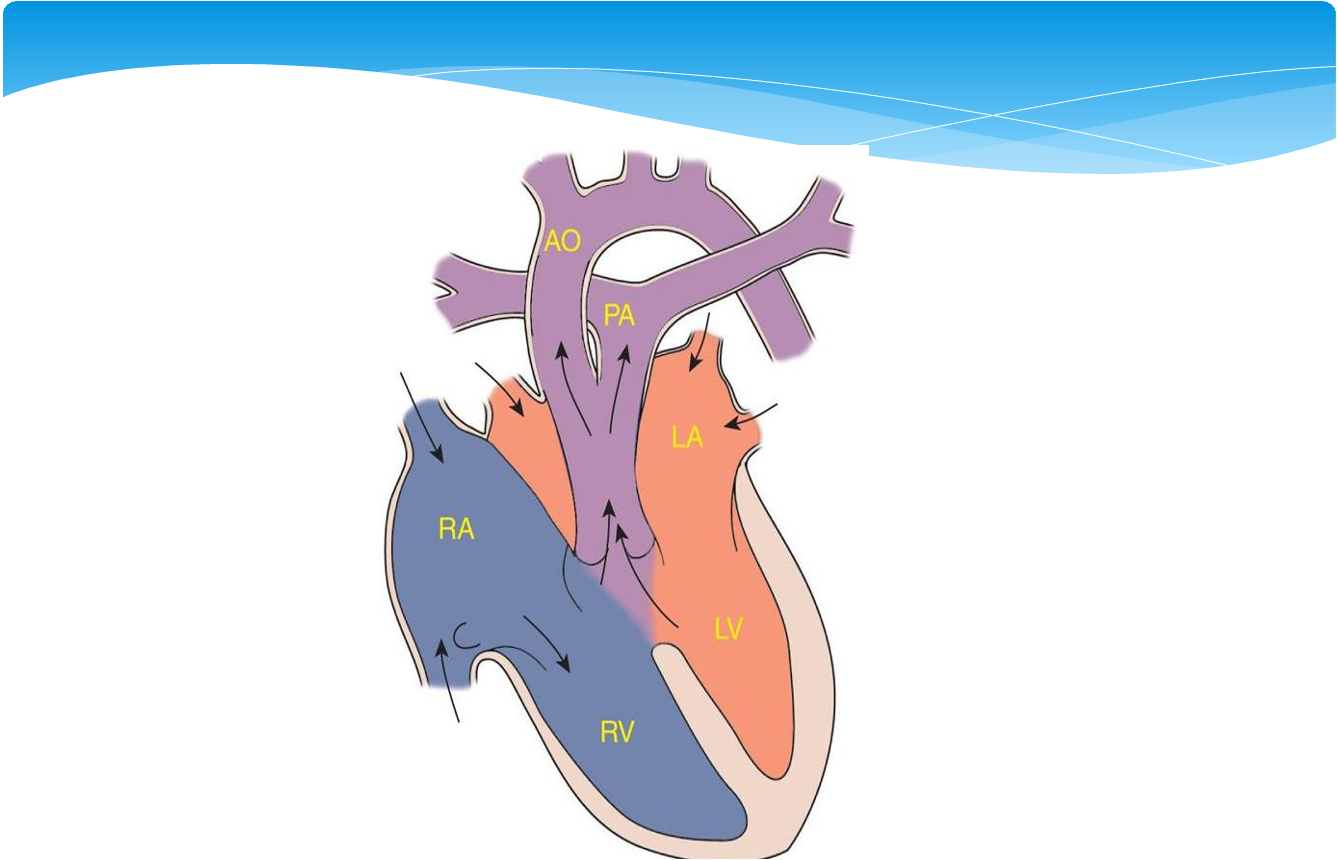
- Transposition of the Great Arteries
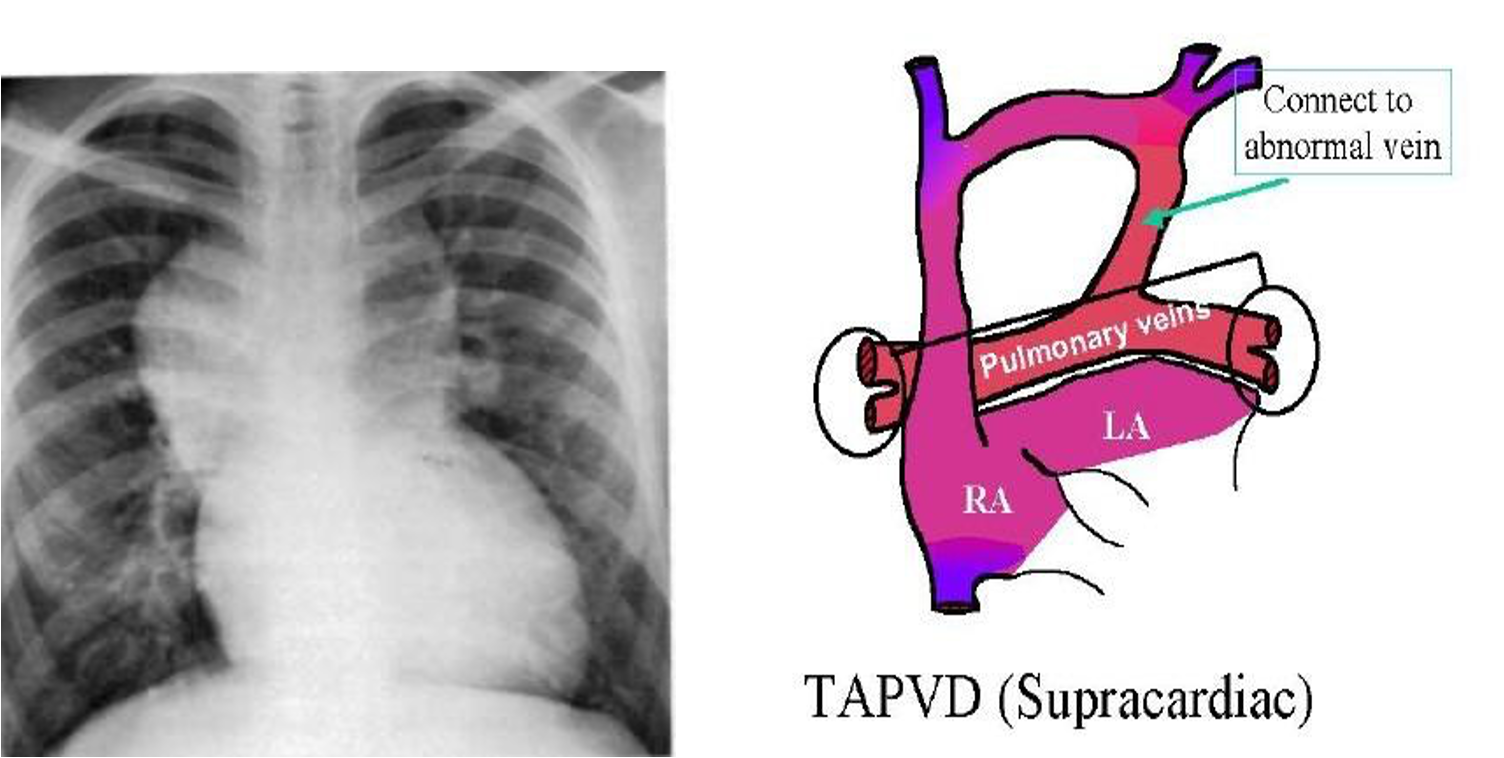
- Total Anomalous Pulmonary Venous Drainage
- Truncus Arteriosus
- Hypoplastic Left Heart Syndrome
Transposition of the Great Arteries
- Although dextroposed transposition of the great arteries represents only about 5% of congenital heart defects, it is the most common cyanotic lesion to present in the newborn period.
- A history of cyanosis is always present, although it depends on the amount of mixing. Tachypnea and a single S2 are typically present. If the ventricular septum is intact, there may be no murmur.
- Children with transposition and a large VSD have improved intracardiac mixing and less cyanosis. They may present with signs of heart failure. The heart is hyperdynamic, with palpable left and right ventricular impulses. A loud VSD murmur is heard. S2 is single.
Case Study
Initial Presentation
- A 5-hour-old male newborn infant was born at 39 weeks gestation via normal vaginal delivery to a 23-year-old G2 P2 O+ mother with unremarkable prenatal serology studies. Apgar scores were 8 and 9 at 1 and 5 minutes. His initial physical exam was normal. He stayed in the mother’s room and breastfed shortly after delivery. At 5 hours of age, with the second feeding, the baby appears tachypneic and cyanotic, and he is therefore taken to the nursery for further evaluation.
Examination
- VS T 37.0, HR 145, RR 78, BP 67/38, oxygen saturation 82% in room air. Length 53 cm (50%ile), weight 3.7 kg (50%ile), HC 34 cm (50%ile). He is an alert active, nondysmorphic and mildly cyanotic term male. Tachypnea and mild nasal flaring are present. His heart is regular with a grade 2/6 soft systolic murmur at the upper left sternal border. The precordium is quiet. Lungs are clear bilaterally. No hepatosplenomegaly is noted.
Further Evaluation
- He is placed in an oxygen hood with a fraction of inspired oxygen (FiO2) of 0.7 (70%) with no appreciable rise in his oxygen saturation. A radial arterial blood gas shows pH 7.44, pCO2 35, paO2 39, bicarb 22 in FiO2 0.7 (70%) by hood.
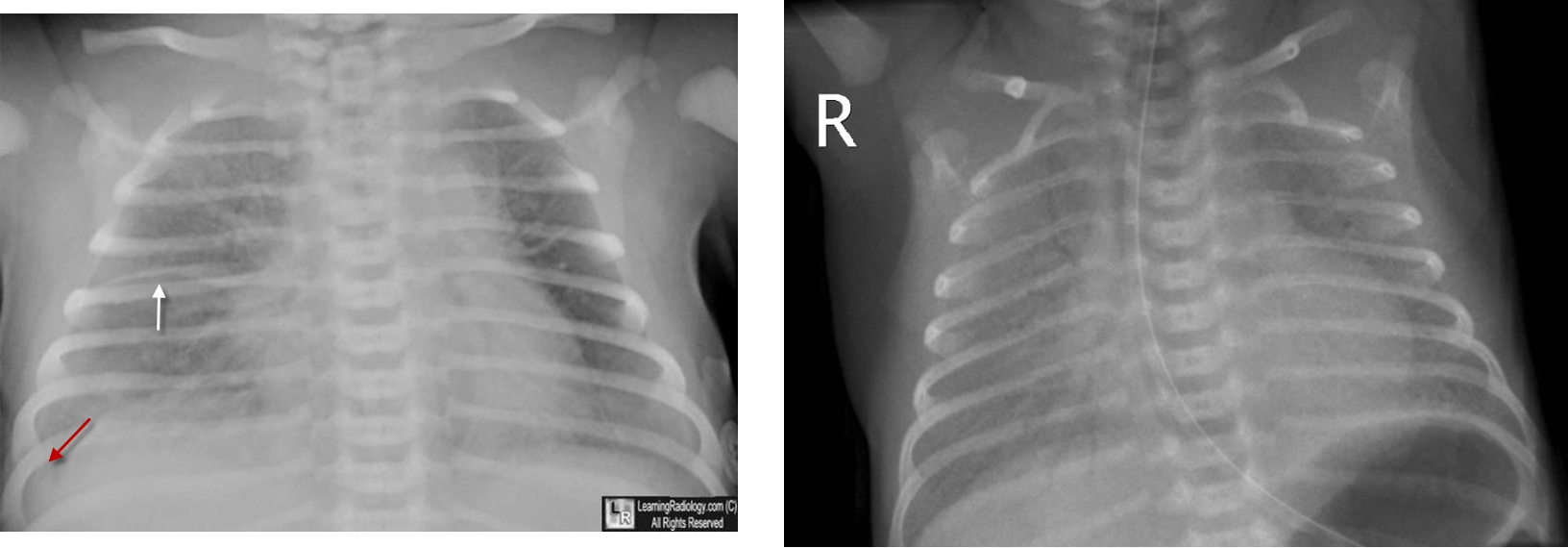
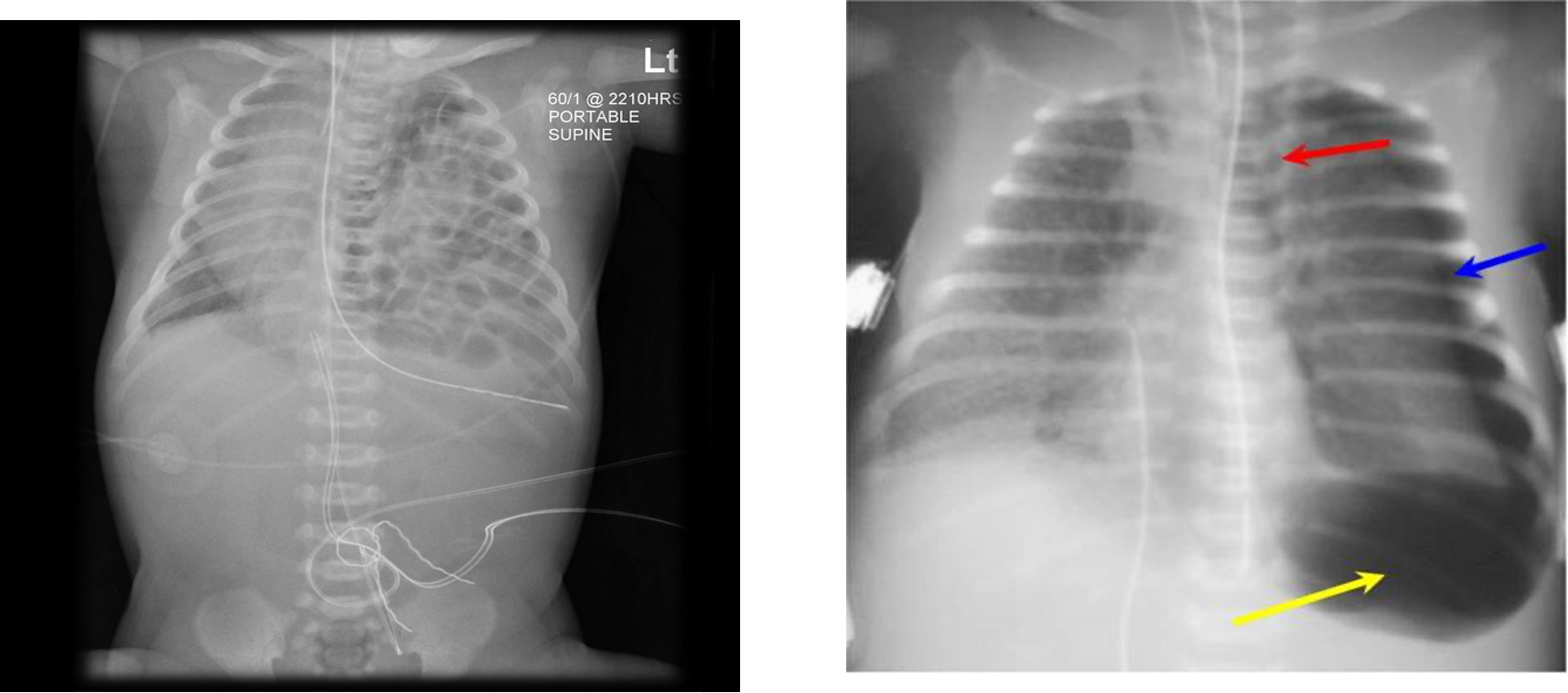
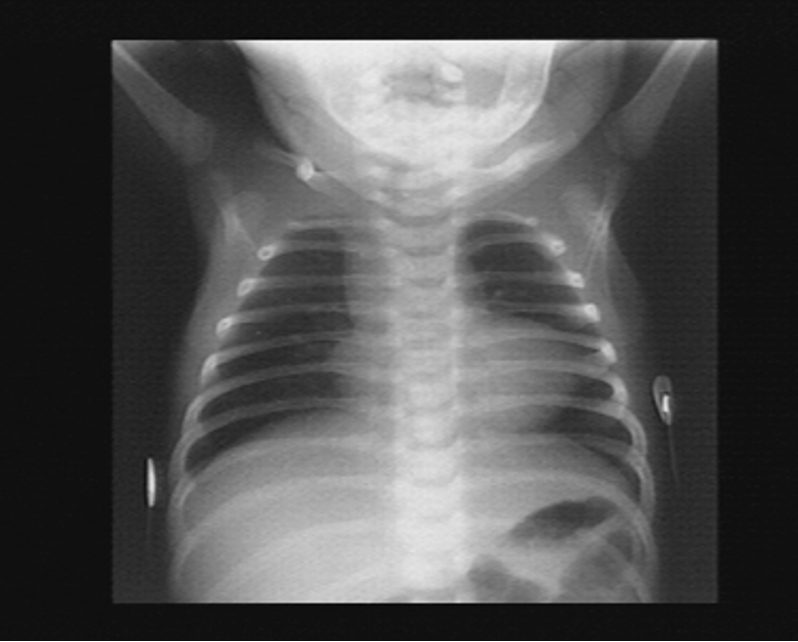
- A chest radiograph: cardiomegaly, narrow mediastinum, and increased pulmonary vasculature. ECG: RAD and RVH

Diagnosis and Treatment
- Echocardiography reveals D-transposition of the great vessels with a 5mm ventricular septal defect and patent ductus arteriosus. A prostaglandin E1 infusion is started. The infant is mechanically ventilated and subsequently transported to a pediatric cardiac surgical specialty center. An arterial switch procedure is performed successfully. He is discharged home 3 weeks later.
Initial Stabilization
- ABC’s: Volume resuscitation, inotropic support, correction of metabolic acidosis, r/o sepsis
- Intubate if needed, titrate FiO2 to keep SpO2 80%-85% to prevent pulmonary overcirculation
- Placement of umbilical lines
- Infants who present in shock within the first 3 weeks of life, consider ductal dependent lesions
- Use of PGE1 (0.025 to 0.1 mcg/kg/min)
Stabilization for Transport
- Reliable vascular access
- Intubation if on PGE1, OG placement
- Oxygen delivery, SpO2
- Monitor HR, tissue perfusion, blood pressure, temp, and acid-base status
- Calcium and glucose status
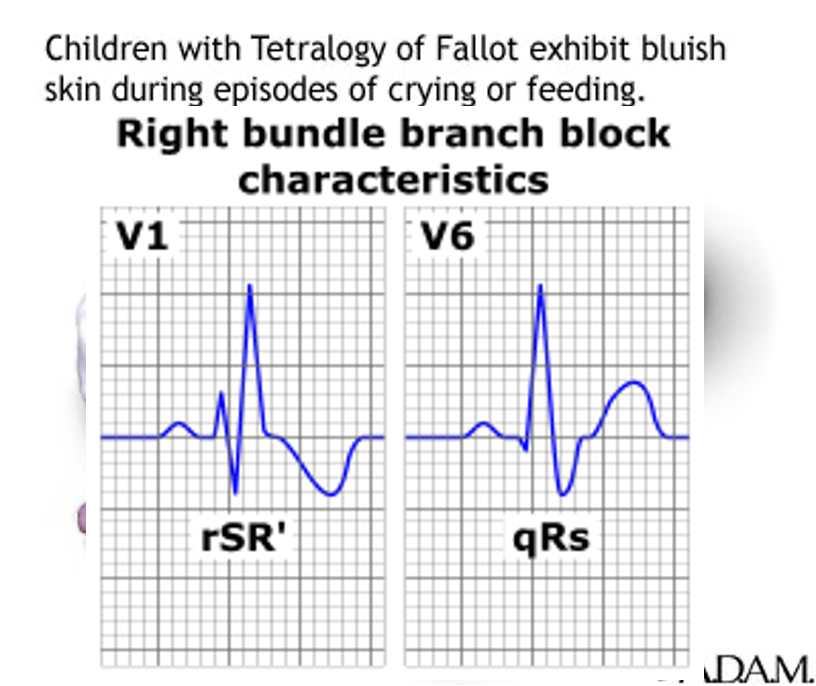
Tetralogy of Fallot
Neonates and infants with central cyanosis or cardiac failure are an emergency – irrespective of their clinical state.
-
TOF is the most common cyanotic congenital heart defect. ~10%.
-
Cyanosis pulmonary stenosis.
-
A pulmonary stenosis murmur.
-
A single S2 and right ventricular impulse at LSB.
-
Hypoxic (Tet) spells: - Hyperpnea occurs with gradually increasing cyanosis and loss of the murmur. - Prolonged unconsciousness and convulsions, - hemiparesis, or death may occur.
-
Increased risk for cerebral thromboembolism and cerebral abscesses.
Case Study
-
You have responded for a 3-month-old male infant because the parents state he is having episodes of excessive crying followed by limpness, cyanosis, and passing out. He was born at 41 weeks of gestation by C-section because of failure to progress. Apgar scores of 7 and 8 at 1 and 5 minutes, respectively. His cyanosis increases with crying.
-
On Exam you note that he is alert and active in respiratory distress, with visible cyanosis. His lungs are clear. He has normal peripheral pulses with cyanotic nail beds and mucous membranes. VS: T 37 (98.6), P164, RR 64, oxygen saturation 83% on blow-by oxygen.
Tetralogy of Fallot
- “Tet spell”
- Hyperpnea
- Worsening cyanosis
- Disappearance of murmur
- RBBB pattern on ECG
Imaging
- Small to N cardiac silhouette
- Decrease pulmonary vasculature
Treatment of Tet Spell
-
Quiet, calm environment
-
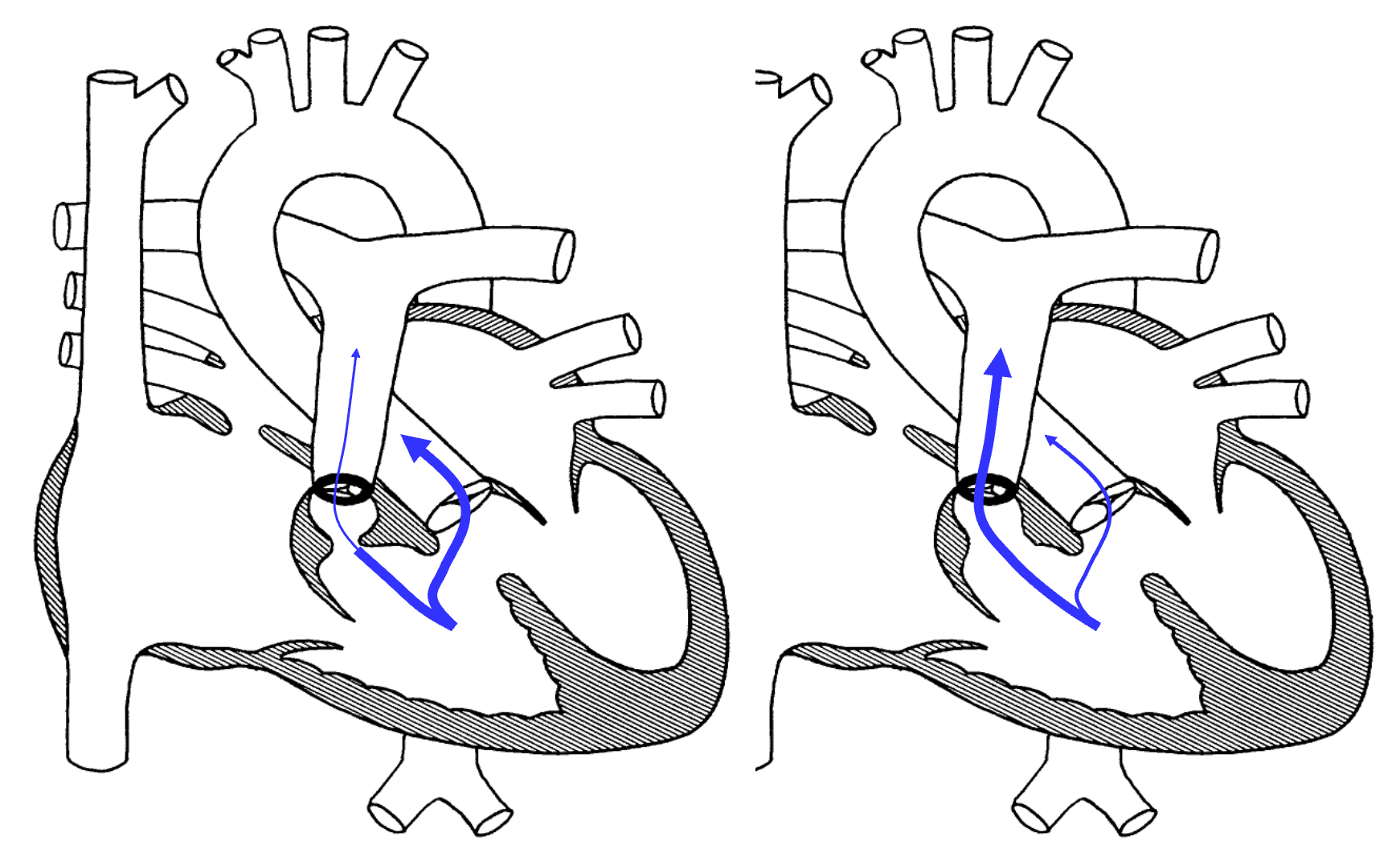
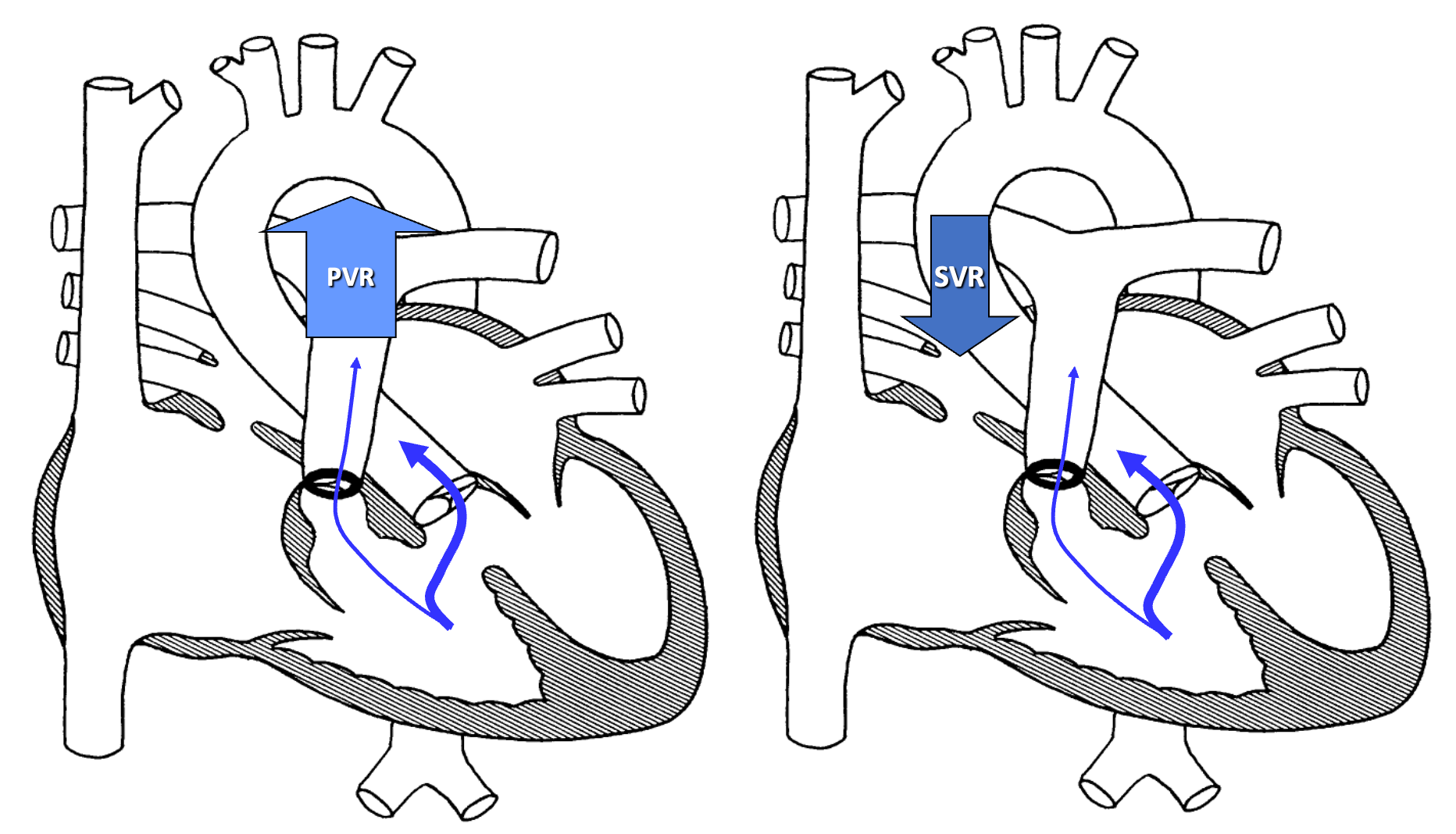
Knee-chest or squatting position increases afterload thus increasing systemic resistance
-
Oxygen
-
Morphine to reduce spasm and/or sympathetic stimulation
-
Phenylephrine increases afterload by promoting systemic vasoconstriction
-
Crystalloids: consider small volume challenge (5-10 cc/kg) to increase preload and SVR
-
NaHCO3 to treat acidosis
Oxygenate to target saturation levels
Squatting
- Common with unrepaired TOF
- Increases oxygen saturations
- Angulation and kinking of femoral arteries with increased SVR, decreasing the R→L shunt

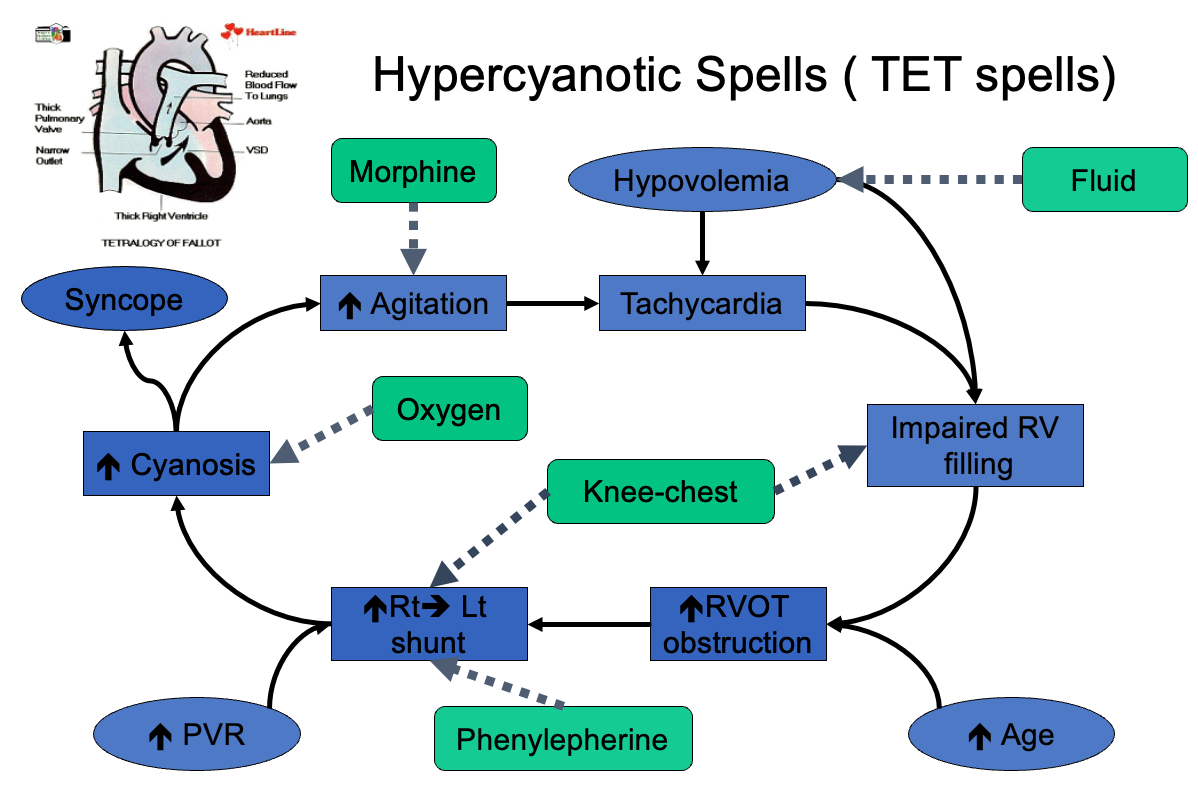
Tachycardia
- Impaired RV filling
- Increased RVOT obstruction
- Increased Rt→Lt shunt
- Increased Agitation
- Hypovolemia
- Increased Age
- Increased PVR
- Hypercyanotic Spells (TET spells)
- Increased Cyanosis
- Syncope
- Fluid
- Morphine
- Oxygen
- Phenylephrine
- Knee-chest
Cyanotic Spells
-
Increase systemic vascular resistance
- Squat/Knee chest position
- Ketamine 1-2mg/kg IV
- Neosynephrine 0.02mg/kg IV
-
Tachycardia & Release of infundibular spasm
- Propranolol 0.1mg/kg IV
-
Irritability: Morphine 0.2mg/kg S.C or IM
-
Hypoxia: Oxygen
-
Dehydration: Volume
-
Acidosis: NaHCO3 1mEq/kg IV
Pulmonary Atresia
- Early cyanosis
- Ductus dependant lesion
- Wide PFO or ASD is needed for right to left shunt (Atrial level)
- If VSD is absent, usually hypoplastic RV is found
Truncus Arteriosus
- Less than 1% of CHD
Total Anomalous Pulmonary Venous Drainage
- Blood flow from lungs is drained to RA instead of LA.
Management of Neonates with Cyanotic Heart Disease
Treatment of Shock
- A, B, C, …..
- Fluid Therapy and Acidosis Correction.
- IV Vasoactive Drugs:
- Dopamine, Dobutamine,
- Epinephrine,
- Isoproterenol,
- Amrinone,
- Phenylephrine.
-
Prostaglandin E1 infusion:
- Should be started as soon as ductus dependent lesion is suspected even before echocardiography confirming the diagnosis.
- Dose: 0.02 – 0.1 micrograms/kg/min.
- Side effects as apnea, hypotension, and fever should be anticipated.
-
Treatment of CHF:
- Digoxin,
- Furosemide, Chlorothiazide, Spironolactone,
- Captopril.
-
Therapeutic Catheterization:
- Balloon atrial septostomy,
- Pulmonary and aortic valvuloplasty,
- Pulmonary artery angioplasty,
- Aortic coarctation angioplasty,
- Closure of systemic-to-pulmonary arterial collateral vessels.
-
Surgical Procedures:
- Palliative surgeries, e.g., pulmonary artery banding.
- Corrective surgeries.
- Neonatal heart transplantation.