Investigations
-
Spirometry:
- Is the primary method for confirming variable airflow limitation. Can confirm airflow obstruction and demonstrates significant reversibility.
- The degree of significant reversibility is defined as an improvement in forced expiratory volume in 1 s (FEV1) ≥12% and ≥200 ml from the pre-bronchodilator value.
-
Bronchodilator response:
- to assess bronchodilator reversibility in almost all adult and adolescent patients with airflow limitation on their baseline spirometry.
Broncho Provocation Testing
- Is a useful tool for diagnosing asthma in patients with normal baseline airflow.
Peak Expiratory Flow (PEF)
- Measured during a brief, forceful exhalation.
- We typically use PEF measurements to monitor patients with a known diagnosis of asthma or to assess the role of a particular occupational exposure or trigger, rather than as a tool for the primary diagnosis of asthma.
Peripheral Eosinophilia and Elevated IgE Levels
- Are supportive of the diagnosis but are not routinely recommended unless dealing with moderate to severe asthma.
Investigation
- Blood tests: For screening of eosinophilia & anemia.
- Tests for allergy: Allergy tests are not useful for the diagnosis of asthma, but they can be helpful to confirm sensitivity to suspected allergic triggers of respiratory symptoms and to guide ongoing management of asthma.
- Imaging: Chest radiographs are not routinely recommended unless the diagnosis is in doubt e.g. - evaluating severe or “difficult-to-control” asthma and when co-morbid conditions (e.g., allergic bronchopulmonary aspergillosis, eosinophilic pneumonia, or atelectasis due to mucus plugging) are suspected.
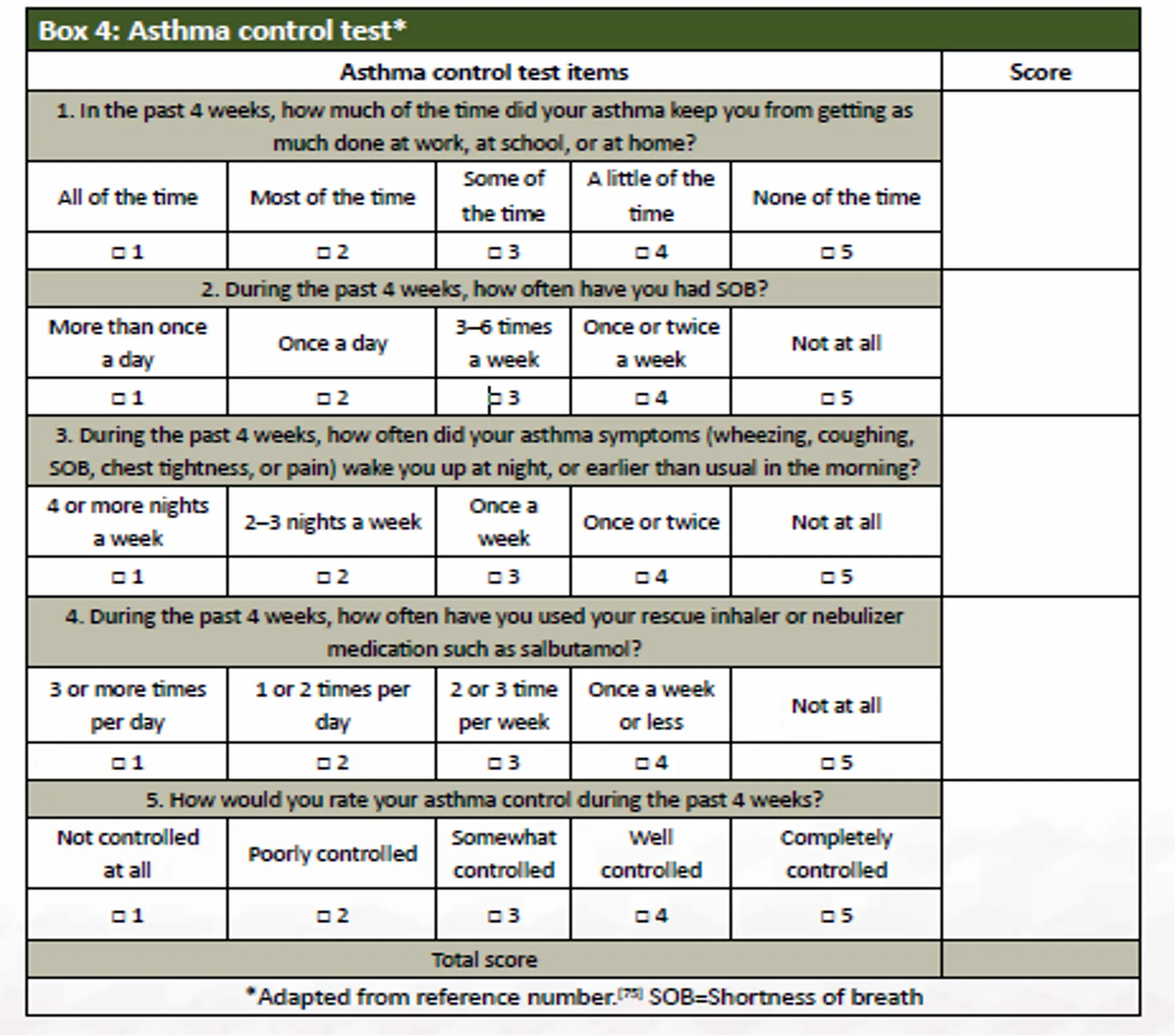
Box 4: Asthma Control Test*
Box 3: Assessing Asthma Control in Adults
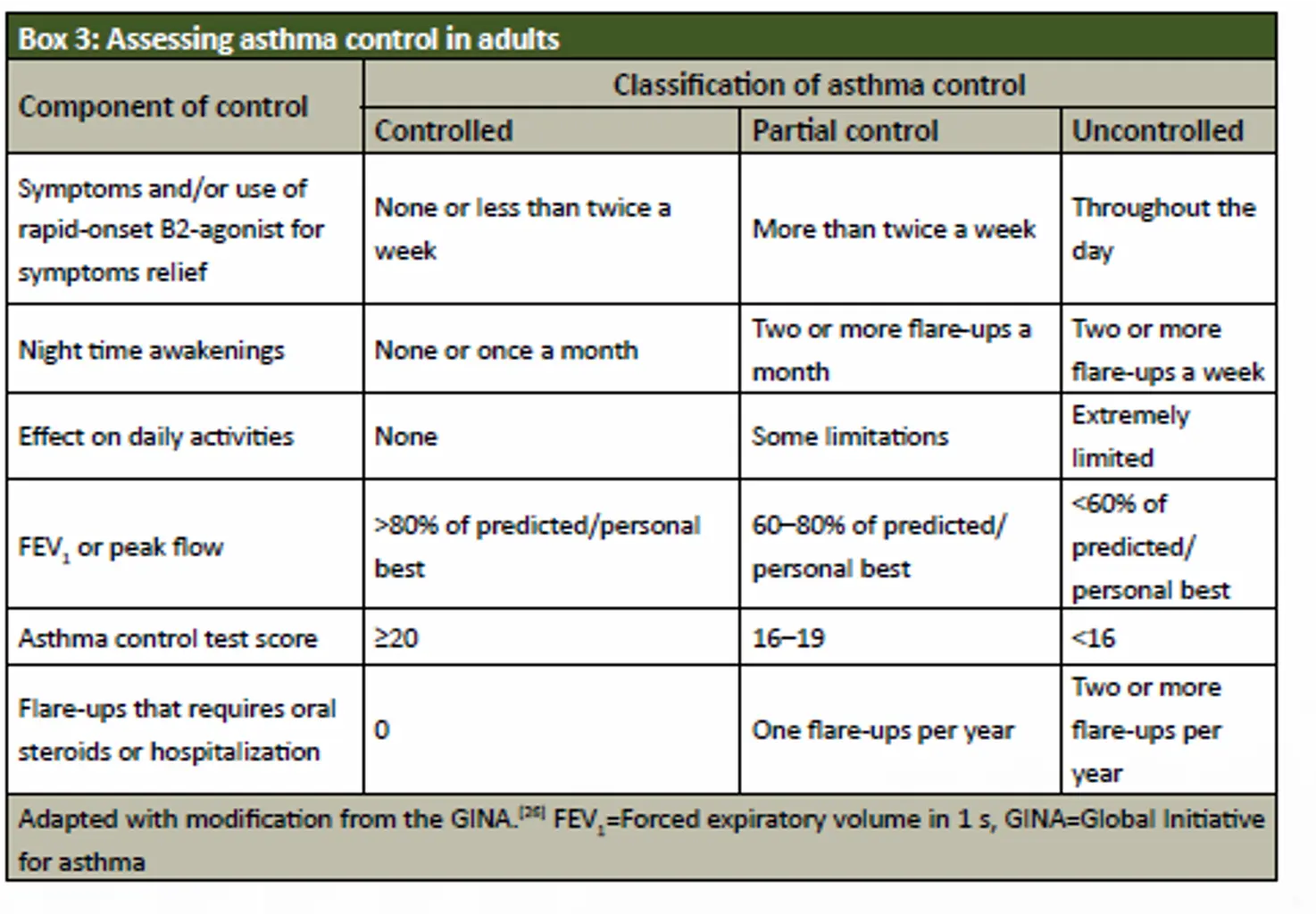
- Component of Control
-
Symptoms and/or use of rapid-onset B2-agonist for symptoms relief
- Controlled: None or less than twice a week
- Partial control: More than twice a week
- Uncontrolled: Throughout the day
-
Night Time Awakenings
- Controlled: None or once a month
- Partial control: Two or more flare-ups a month
- Uncontrolled: Two or more flare-ups a week
-
Effect on Daily Activities
- Controlled: None
- Partial control: Some limitations
- Uncontrolled: Extremely limited
-
FEV₁ or Peak Flow
- Controlled: >80% of predicted/personal best
- Partial control: 60-80% of predicted/personal best
- Uncontrolled: <50% of predicted/personal best
-
Asthma Control Test Score
- Controlled: ≥20
- Partial control: 16-19
- Uncontrolled: <16
-
Flare-ups that require oral steroids or hospitalization
- Controlled: 0
- Partial control: One flare-up per year
- Uncontrolled: Two or more flare-ups per year
-
Adapted with modification from the GINA. FEV₁=Forced expiratory volume in 1 s, GINA=Global Initiative for asthma
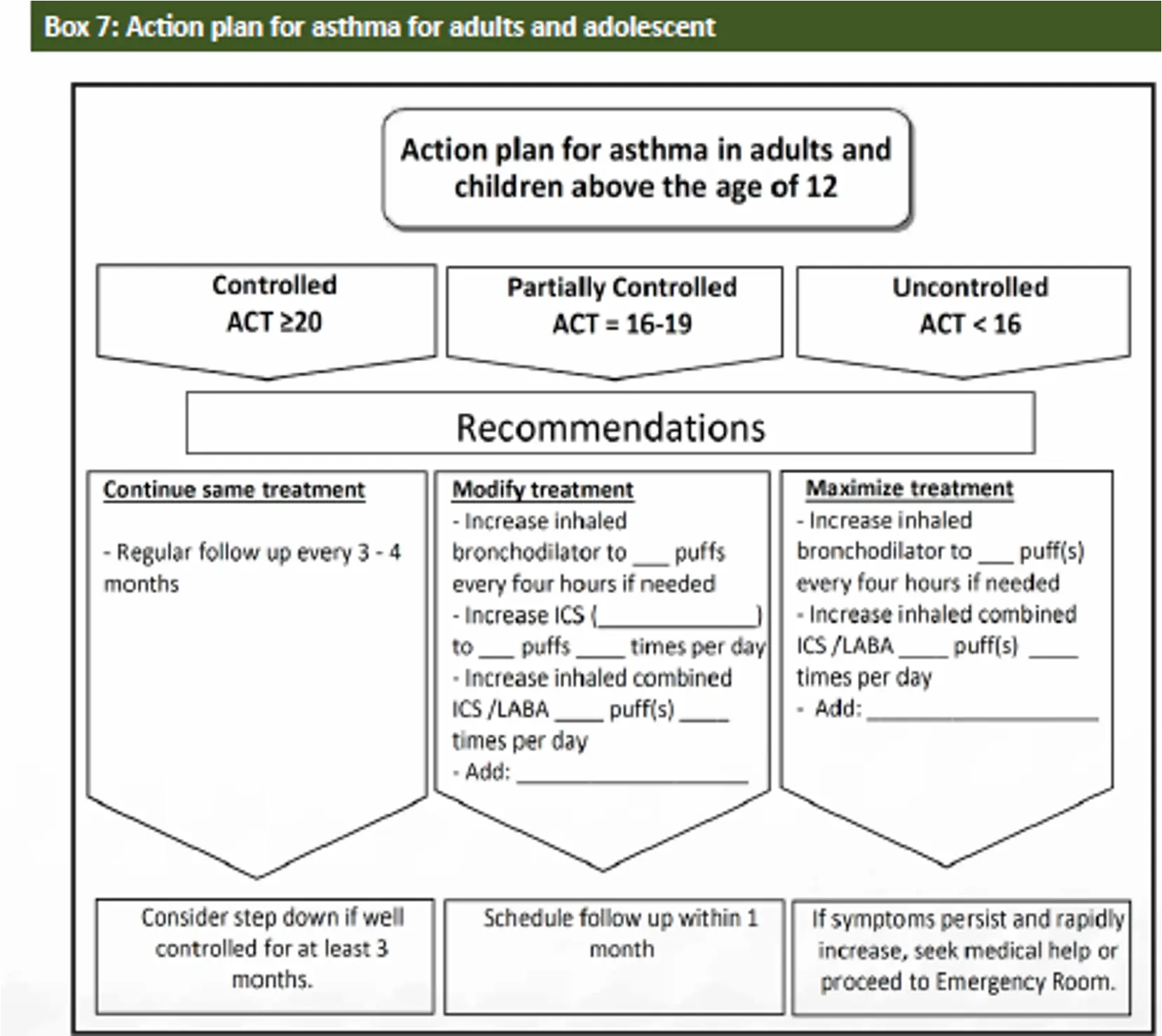
Box 7: Action Plan for Asthma for Adults and Adolescents
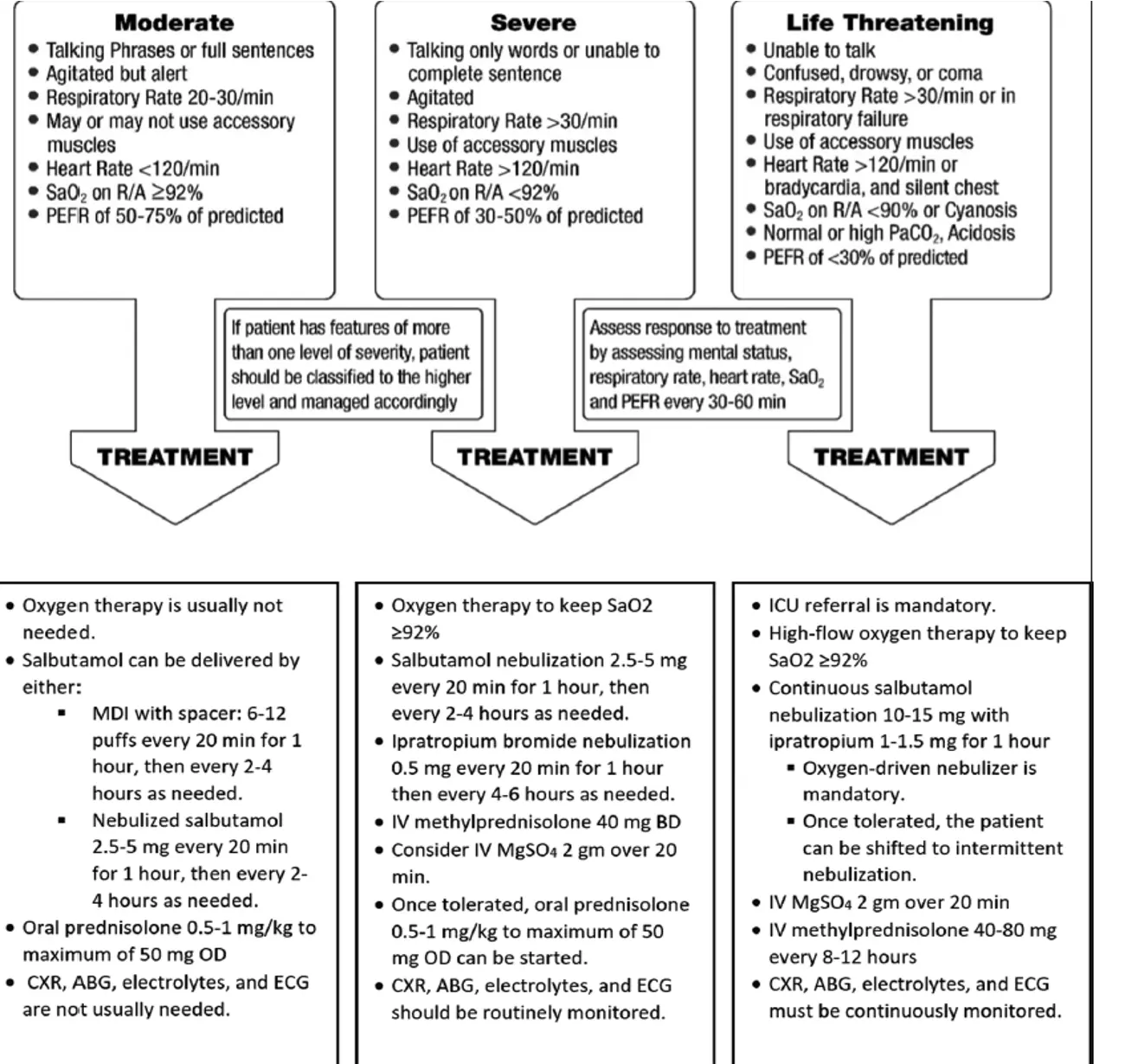
Clinical Assessment of Acute Asthma
- The presence of the following features should be sought:
- Previous history of near-fatal asthma
- Whether the patient is taking three or more medications
- Heavy use of SABA
- Repeated visits to the ED
- Brittle asthma.
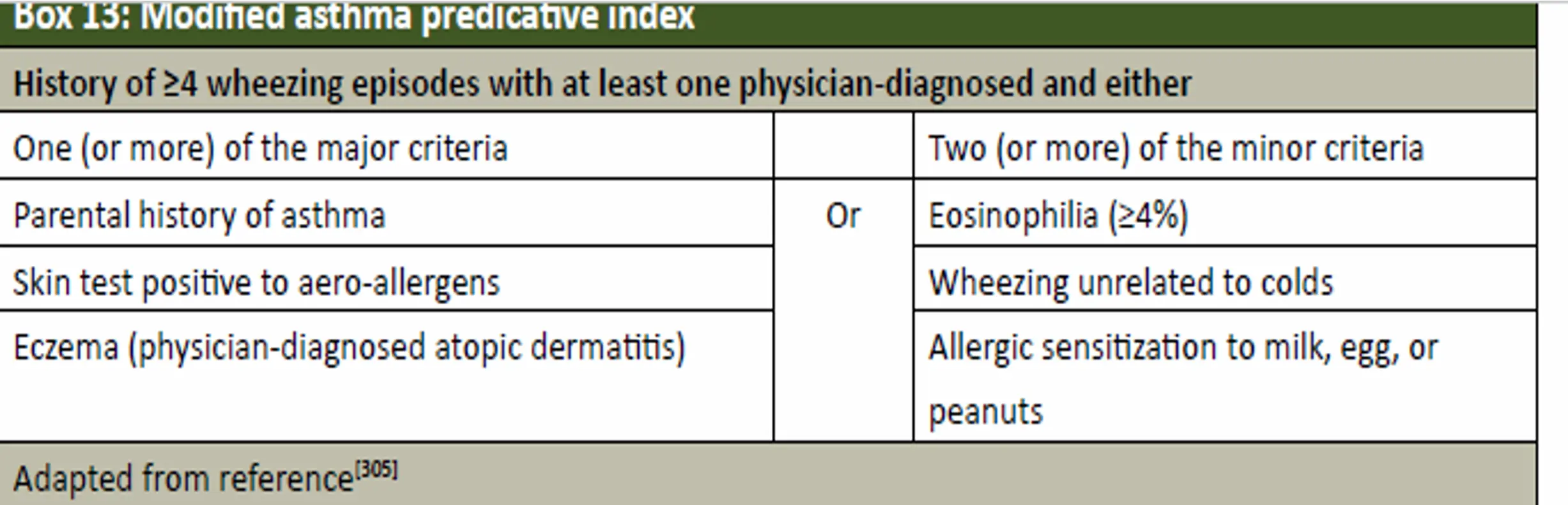
Prediction of Asthma in Preschool Children
Box 13: Modified Asthma Predictive Index
-
History of ≥4 wheezing episodes with at least one physician-diagnosed and either
- One (or more) of the major criteria
- Parental history of asthma
- Skin test positive to aero-allergens
- Eczema (physician-diagnosed atopic dermatitis)
- Two (or more) of the minor criteria
- Eosinophilia (≥4%)
- Wheezing unrelated to colds
- Allergic sensitization to milk, egg, or peanuts
- One (or more) of the major criteria
-
Adapted from reference[305] #Z
Asthma Mimics
- Should be suspected when any of the following is present:
- Failure to thrive,
- Onset of symptoms during infancy,
- Vomiting associated with respiratory symptoms,
- Continuous wheezing,
- Failure to respond to asthma controller medication,
- Clubbing or focal auscultation signs.
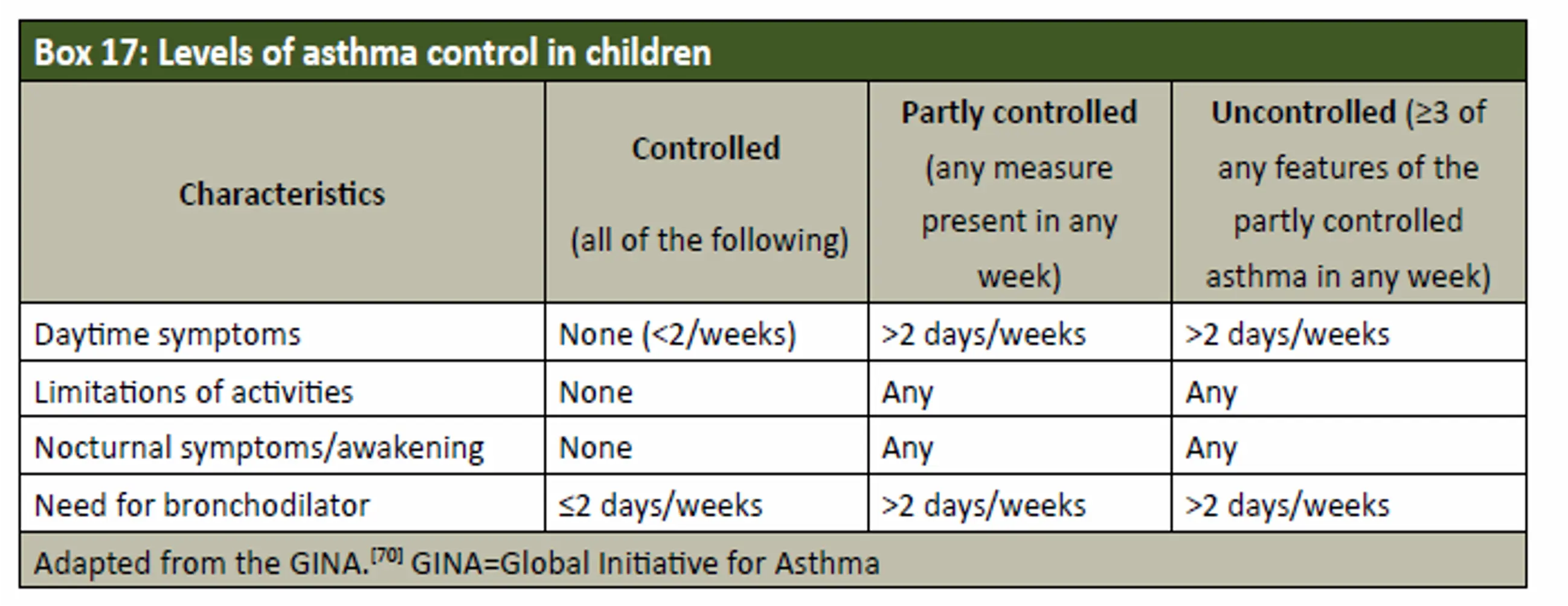
Box 17: Levels of Asthma Control in Children
Characteristics
| Controlled (all of the following) | Partly Controlled (any measure present in any week) | Uncontrolled (≥3 of any features of the partly controlled asthma in any week) |
|---|---|---|
| Daytime symptoms | None (<2/week) | >2 days/week |
| Limitations of activities | None | Any |
| Nocturnal symptoms/awakening | None | Any |
| Need for bronchodilator | ≤2 days/week | >2 days/week |
The Childhood-ACT (C-ACT)
- The C-ACT is a validated test for 4–12 years old children.
- Is a two-part questionnaire with a total of seven questions. The first part is to be answered by the patient and the second part by the caregiver.
- The final C-ACT score is made up of the sum of the scores of the two parts, ranging from 0 (poorest asthma control) to 27 (optimal asthma control).
- A score of ≤19 points suggests that a child’s asthma is not adequately controlled.
❖ See box 18
Age Group <5 Years: The Test for Respiratory and Asthma Control in Kids (TRACK)
- This is a validated test for children <5 years.
- It is a 5-item standardized questionnaire.
- Four questions that address the impairment domain and one question that addresses the risk domain of asthma control.
- Each item is scored from 0 to 20 points on a 5-point Likert-type scale.
- For a total score ranging from 0 to 100. Higher scores would indicate better respiratory and asthma control.
- A score of <80 points suggests that a child’s asthma is not controlled.
Outpatient Management of Asthma in Children Aged 5–12 Years
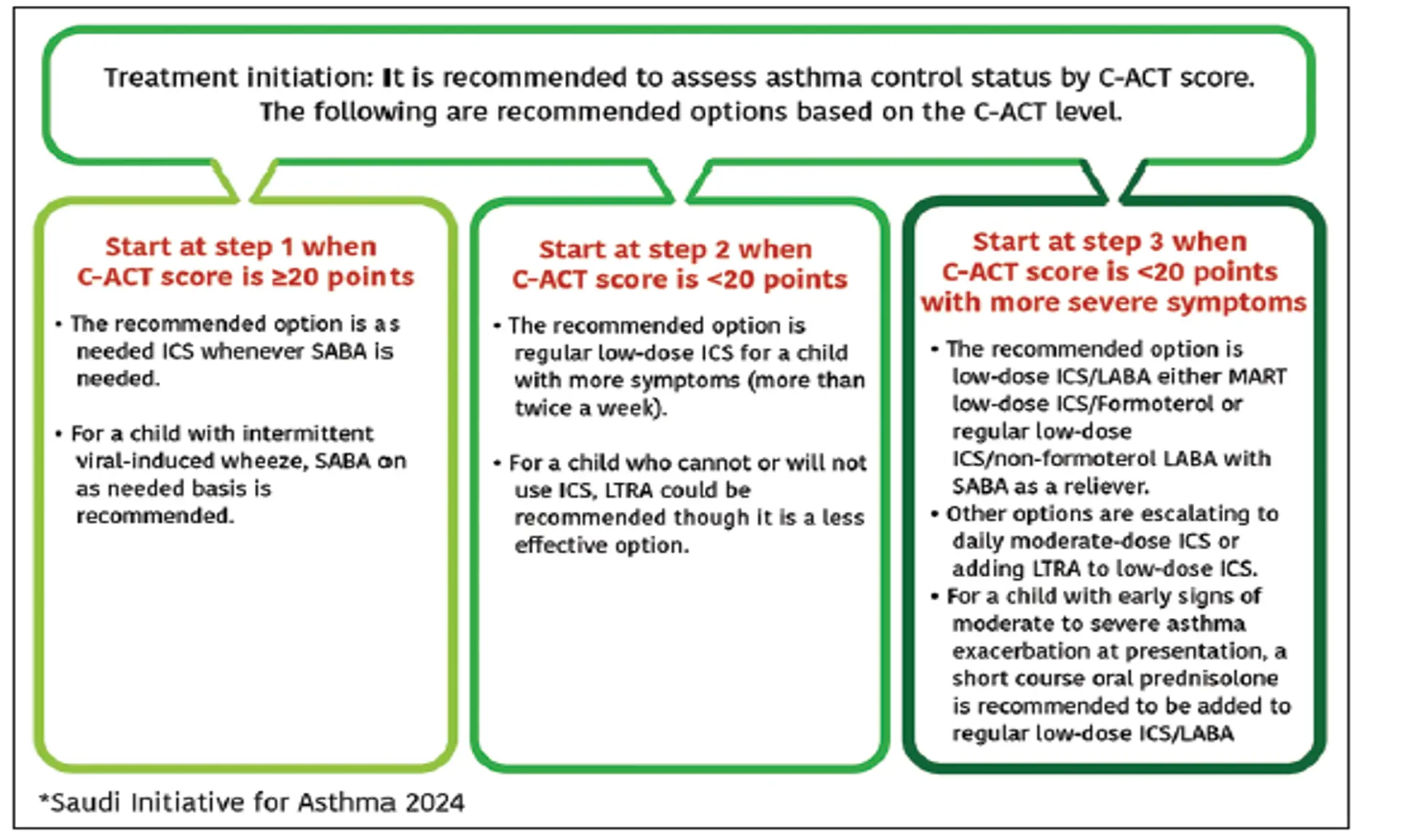
Treatment Initiation: It is recommended to assess asthma control status by C-ACT score. The following are recommended options based on the C-ACT level.
-
Start at Step 1 when C-ACT score is ≥20 points
- The recommended option is a needed ICS whenever SABA is needed.
- For a child with intermittent viral-induced wheeze, SABA on an as-needed basis is recommended.
-
Start at Step 2 when C-ACT score is <20 points
- The recommended option is regular low-dose ICS for a child with more symptoms (more than twice a week).
- For a child who cannot or will not use ICS, LTRA could be recommended though it is a less effective option.
-
Start at Step 3 when C-ACT score is <20 points with more severe symptoms
- The recommended option is low-dose ICS/LABA either MART low-dose ICS/Formoterol or regular low-dose ICS/non-formoterol LABA with SABA as a reliever.
- Other options are escalating to daily moderate-dose ICS or adding LTRA to low-dose ICS.
- For a child with early signs of moderate to severe asthma exacerbation at presentation, a short course oral prednisolone is recommended to be added to regular low-dose ICS/LABA.
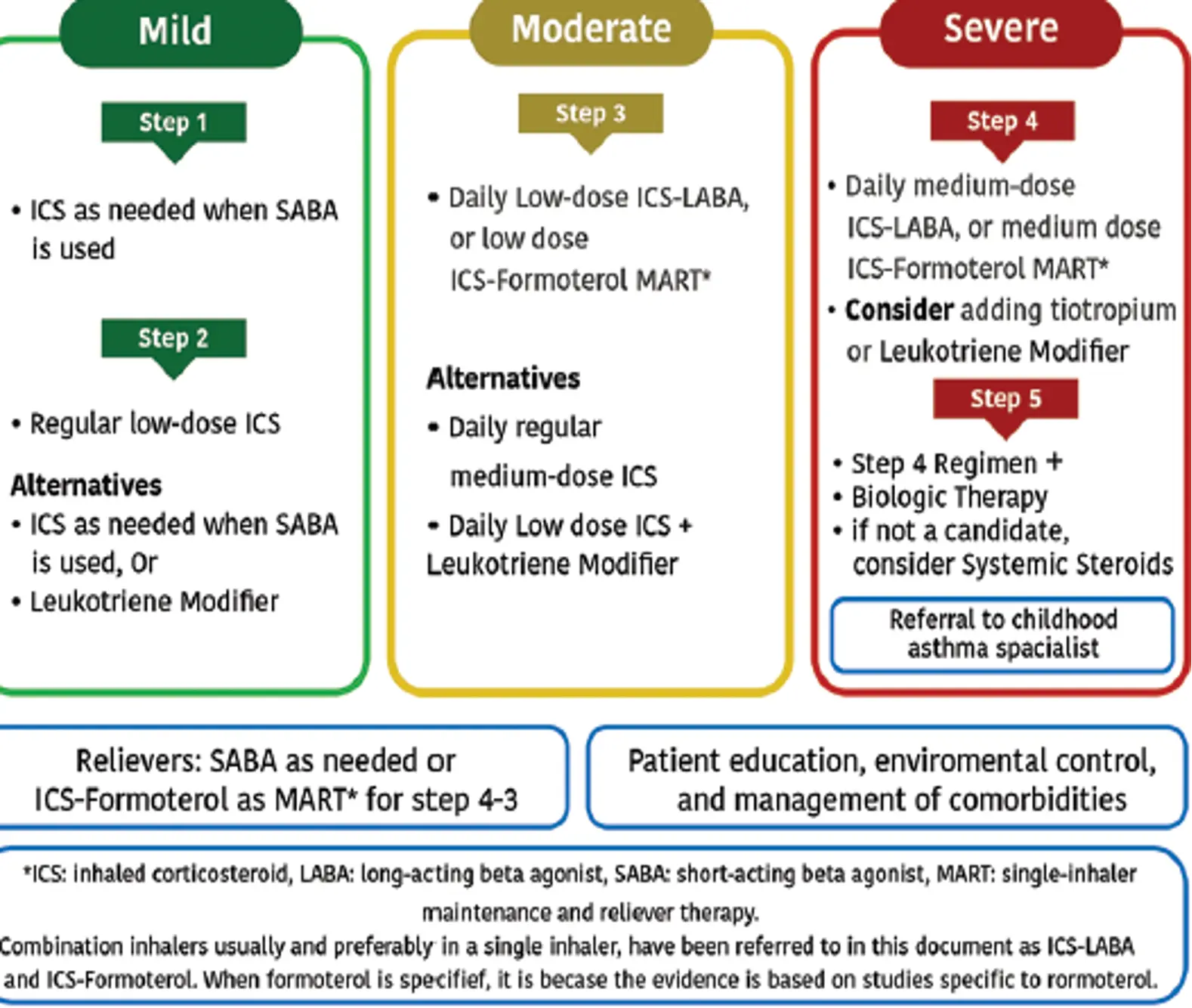
Saudi Initiative for Asthma 2024
Step 1
- The recommended option is as needed ICS whenever SABA is required.
Step 2
-
The recommended option is low dose-ICS (step 2).
-
Alternatively, either use of ICS whenever SABA is required, or daily LTRA that are less effective option at this step
-
For a child with intermittent viral-induced wheeze daily low-dose ICS is recommended.
Step 3
-
The recommended option is low dose ICS/LABA either MART of ICS/Formoterol or regular ICS/non-formoterol LABA with SABA as a reliever.
-
Other options are escalating to daily moderate-dose ICS or adding LTRA to low-dose ICS
Step 4
-
The recommended option is medium-dose ICS/LABA either MART of ICS/Formoterol or daily of ICS/non-formoterol LABA inhaler with SABA as a reliever.
-
Tiotropium or LTRA may be added to this combination if control is not achieved
Step 5
-
It is recommended to refer the child to a physician specialized in asthma as there are growing evidence to support biologics for children with uncontrolled asthma at Step 4. The following are SINA expert panel recommendations for biological therapy at step 5 for this age group:
-
Anti-IgE therapy is a well-established therapy in children aged ≥6 years with uncontrolled asthma at Step 4 who fulfil the following criteria: severe persistent allergic asthma with frequent daytime symptoms or night-time awakenings, and who have multiple documented severe asthma attacks despite treatment at Step 4
Outpatient management of Asthma for children age 5-12