Neoplasms of endocrine pancreas
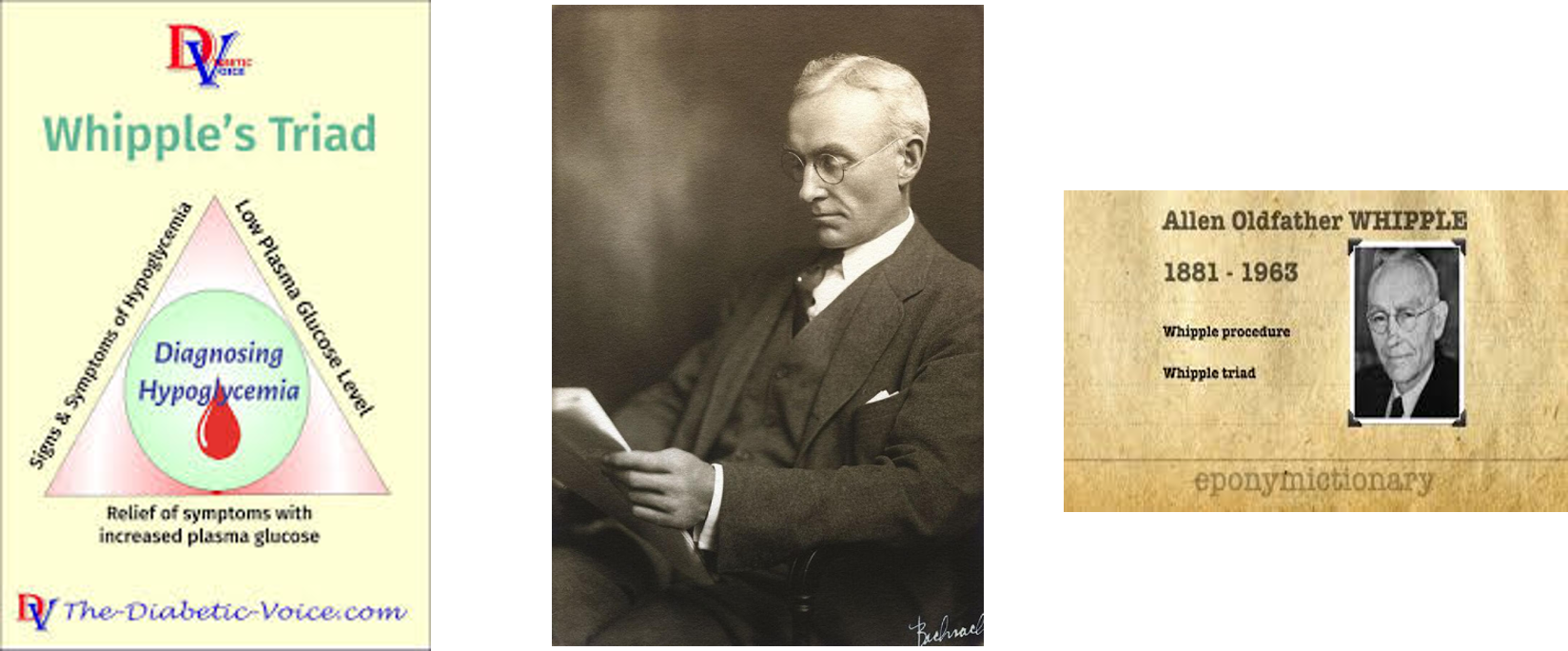
- Insulinoma ((too much insulin = hypoglycemia = high risk death))
- Glucagonoma
- Gastronome
- VIPoma
Neoplasms of exocrine pancreas
Benign tumors Z
- Serous cystadenoma (100% benign - removed if large)
- Mucinous cystadenoma (Pre-malignant if >3cm - must be removed)
- Intraductal papillary mucinous neoplasm (IPMN) (Pre-malignant >3cm removed - screen)
Malignant tumors
- Ductal adenocarcinoma (the commonest)
- Acinar adenocarcinoma
- Mucinous cystadenocarcinoma
- Intraductal papillary mucinous neoplasm (IPMN)
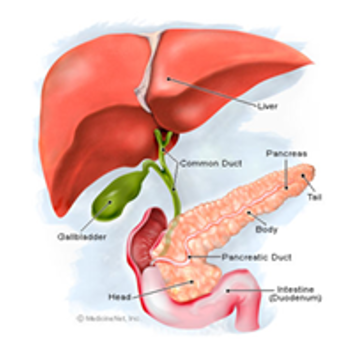
Note: Periampullary tumors could originate from the head of the pancreas, distal CBD, or from the Ampullary mucosa of the duodenum and commonly the patient presents early with jaundice due to the early obstruction of the CBD.
Benign Tumors
- Serous Cystadenoma (Microcystic)
- Mucinous Cystic Tumor

-
3cm
- Intraductal Papillary Mucinous Neoplasms. (IPMN) Y
- Older males.
- Arise in the head and uncinate process of the pancreas, and they are typically connected to the ductal system of the pancreas.
- IPMNs comprise lesions of the main pancreatic duct, side branches, or a combination.
- The prevalence of malignancy:
- lesions of the main-duct: 57–92%
- lesions of side-branch: 6–46%
- Mixed features of microcystic and macrocystic lesions.
- The main pancreatic duct is often dilated.
- Contain mucinous fluid which is sometimes extruding from the ampulla of Vater.
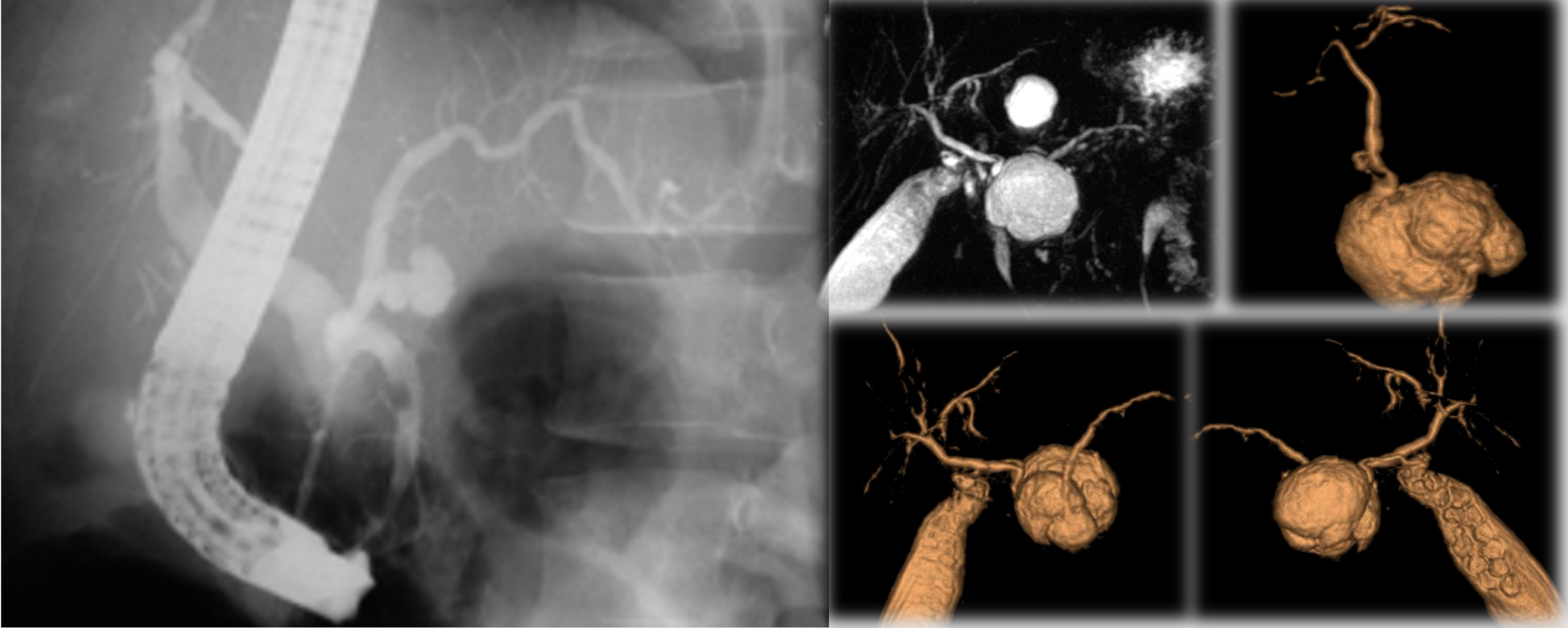
Intraductal Papillary Mucinous Tumor (IPMT)
Occurs in four forms: Y
- Main pancreatic duct: (1) Segmental (NS) |(2) Diffuse.
- Branch duct: (3) Macrocystic | (4) Microcystic.

IPMT of the MPD
- Segmental or diffuse.
- Incidence M=F, Age: 6th decade.
- Radiologic features mimic chronic pancreatitis or chronic obstructive pancreatitis.
- ERCP remains the imaging modality of choice for diagnosis.
Management: Guidelines
The most recent guideline for the management of pancreatic cysts was published in 2007 (#).
- Incidental cysts to be evaluated (MCN and IPMN premalignant).
- The initial imaging test proposed is a CT scan, which may be followed by EUS-FNA in particular cases when FNA is needed for CEA level or to puncture a solid component.
- Resection is recommended in all MCNs and main-duct IPMNS.
- Firm recommendations for the management of branch-duct IPMNs are not provided.
- Serous Cystadenomas should only be resected if symptomatic or if the diagnosis remains in doubt.
- All pseudopapillary neoplasms should be considered for resection.
- Interval follow-up ??? No guidelines
A. Khalid and W. Brugge, “ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cysts,” American Journal of Gastroenterology, vol. 102, no. 10, pp. 2339–2349, 2007.
Pancreatic carcinoma
Tumor Staging according to the TNM System
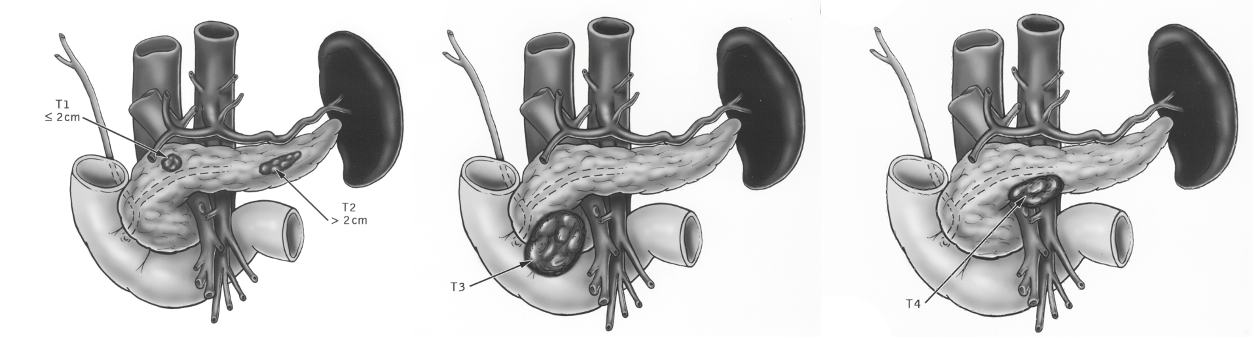 T1 = <2cm
T2 = 2-5 cm
T3 = >5 cm
T4 = Invasion of adjacent tissue
T1 = <2cm
T2 = 2-5 cm
T3 = >5 cm
T4 = Invasion of adjacent tissue
n1 peripancreatic ln n2 far from origin
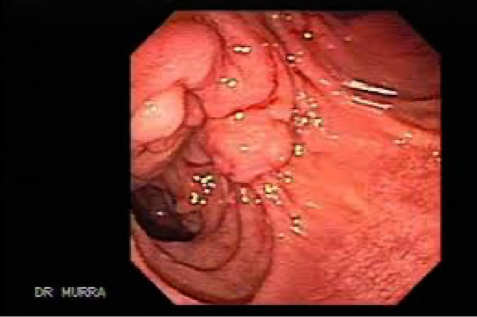
Periampullary tumor (endoscopic view)
Clinical features of pancreatic neoplasms
Presenting symptoms depend on the site of the tumor within the pancreas.
-
Tumor in the head of pancreas: painless obstructive jaundice associated with weight loss is the classical presentation due to obstruction of the CBD. Obstruction of the flow of bile to the intestine will disrupt the enterohepatic circulation which results in dark urine and pale stool. The patient may also have intense itching. The gallbladder may become dilated and palpable (Courvoisier’s sign or law).
-
Tumor in the body and tail of pancreas: Biliary obstruction occurs late, and symptoms are vague, with anorexia, weight loss, and with subsequent involvement of the retroperitoneum, the development of back pain. New-onset diabetes may predate the diagnosis. A late manifestation is a malignant-associated hypercoagulable state, resulting in intravascular clots with vasculitis, named thrombophlebitis migrans (Trousseau’s sign)
Investigations of pancreatic tumors
Laboratory tests: Liver function tests to confirm the cholestasis, tumor markers especially CA19-9 to help in the diagnosis of malignant tumors of the pancreas - alpha feto protein
Imaging
-
Ultrasound abdomen is the initial imaging which will show intra and extrahepatic biliary dilatation in jaundiced patients and will assess for gallstones.
-
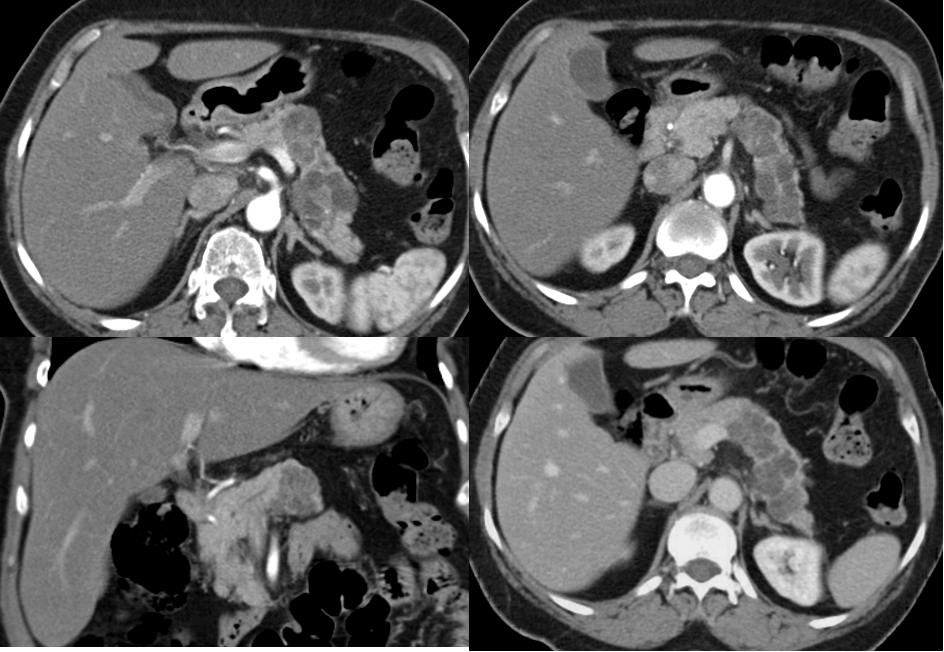
CT scan and MRI can assess the site of the tumor in the pancreas and the evidence of metastases or local invasion by the tumor (staging)
-
Upper gastrointestinal endoscopy and endoscopic ultrasound guidance can help in taking a biopsy from the tumor
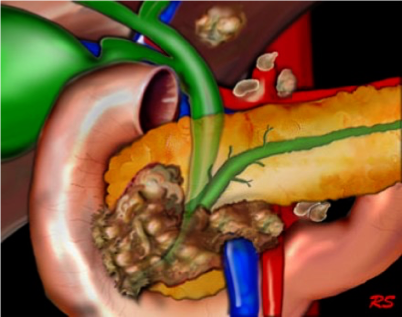
Tumor in the head of pancreas
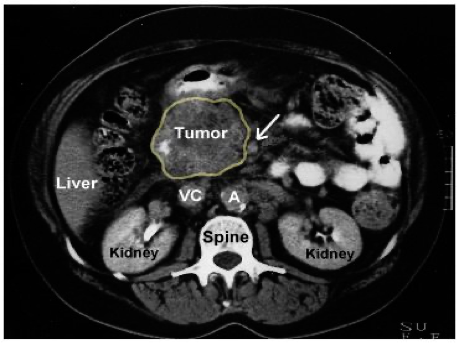 SMA - Small bowel supply from arrow -
SMA - Small bowel supply from arrow -
Treatment
A. Curative treatment Surgical resection currently offers the only potential for cure in pancreatic tumors. Tumors localized to the pancreatic parenchyma, or with limited involvement of peripancreatic fat or lymph nodes may be considered for resection
-
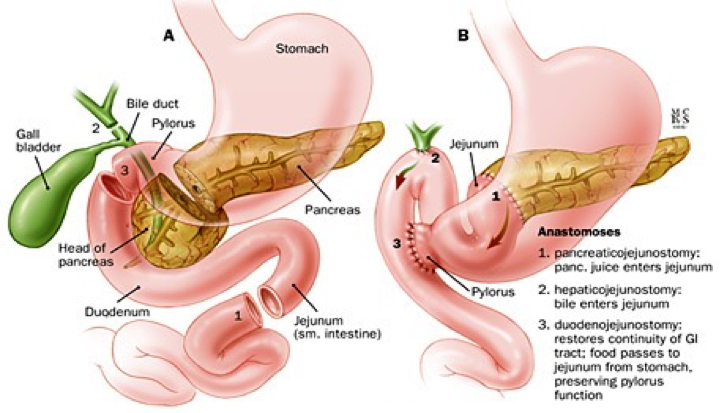
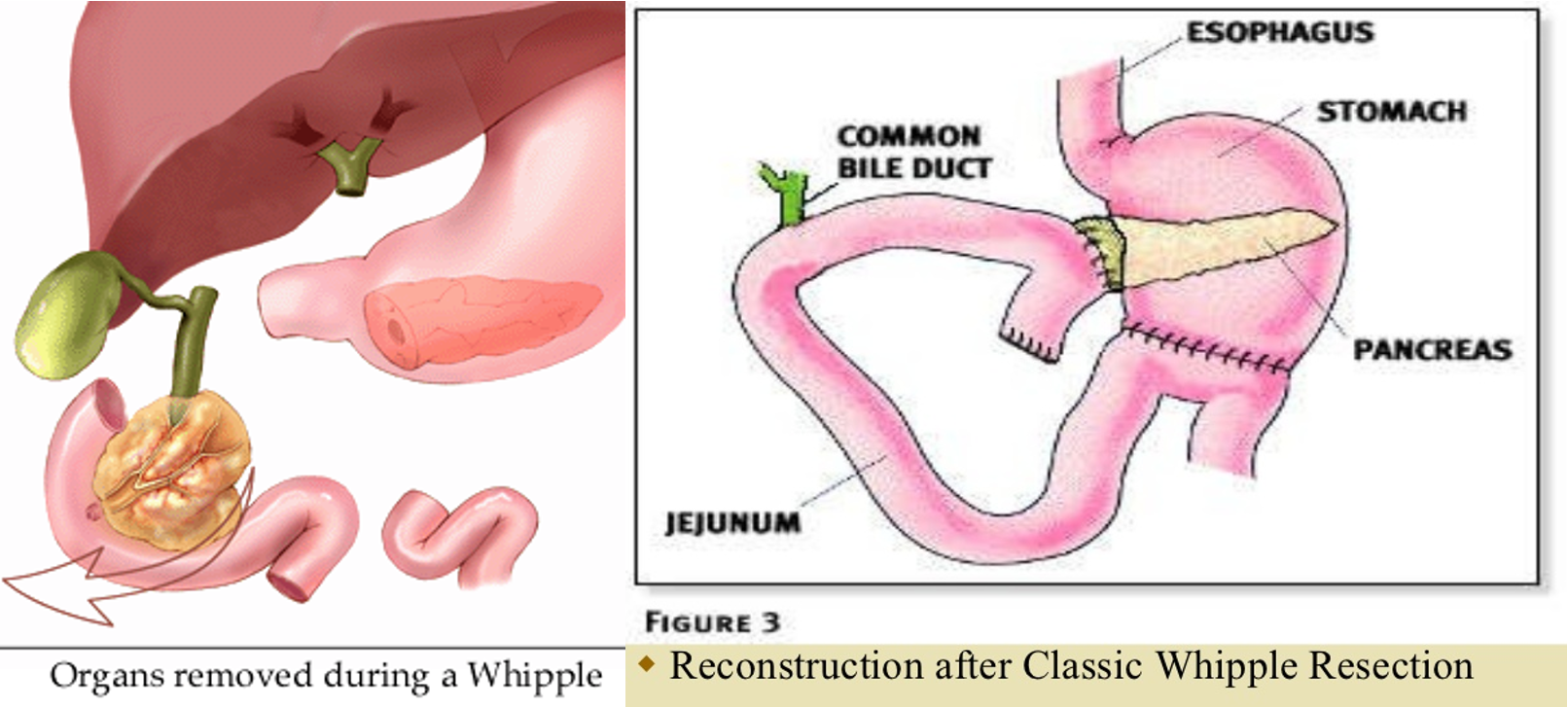
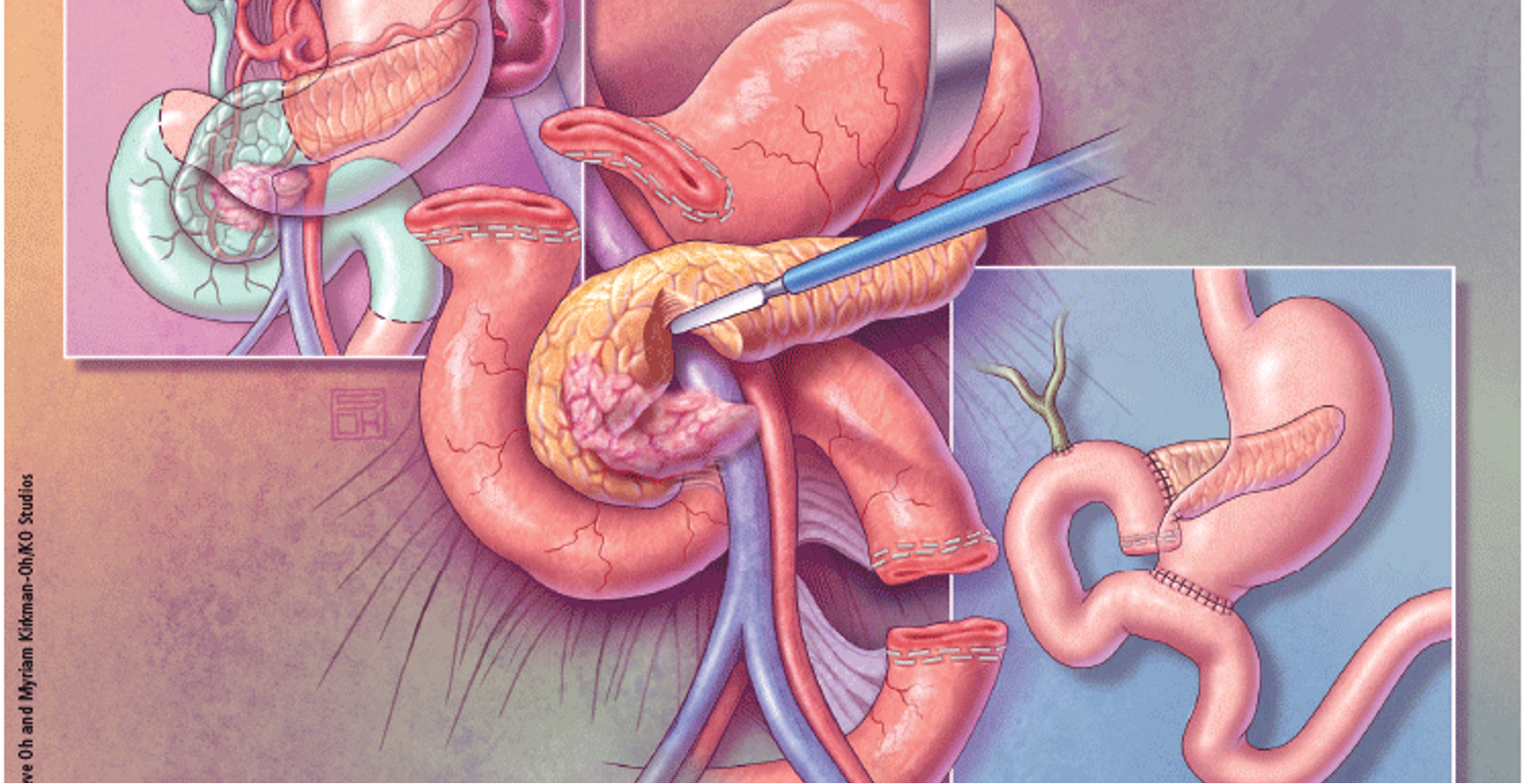
Tumors involving the head of the pancreas are treated by pancreaticoduodenectomy (Whipple’s procedure), which entails block resection of the head of the pancreas, the distal half of the stomach, the duodenum, gallbladder, and common bile duct.
-
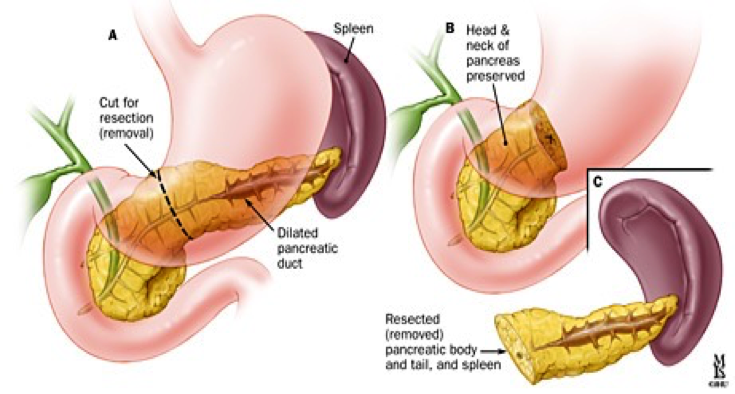
Tumors involving the body or tail of the pancreas are removed by distal pancreatectomy and splenectomy.
-
Pruritus treatment with cholestyramine
-
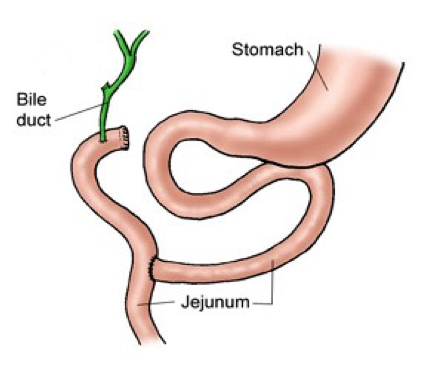
Good operative risk patients may undergo triple bypass to relieve the obstructive jaundice and duodenal obstruction
Whipple’s procedure
Distal pancreatectomy
B. Palliative treatment The aim is optimization of life in patients with non-resectable tumors. Such patients require a histological diagnosis before starting any chemotherapy.
- Obstructive jaundice: can be relieved by ERCP with biliary stenting
- Pain relief with analgesia or splanchnic nerve block (percutaneous, surgical, or endoscopic ultrasound guidance).
- Pruritus treatment with cholestyramine
- Good operative risk patients may undergo triple bypass to relieve the obstructive jaundice and duodenal obstruction
Triple bypass procedure
Prognosis of Ca head of Pancrease
Based on people diagnosed with pancreatic cancer between 2009 and 2015.
| SEER Stage | 5-year Relative Survival Rate |
|---|---|
| Localized | 37% |
| Regional (L) | 12% |
| Distant (M) | 3% |
| All SEER stages combined | 9% |
Neoadjuvant Surgery Neoadjuvant FOLFIRINOX