MOA
Static drug
inhibit folic acid formation of bacteria ((dihydro…)); human are not affected as they don’t possess the enzyme.
Pharmacokinetics
Absorption and distribution:
-
After oral administration, most sulfa drugs are well absorbed (the best is sulphadiazine) but an exception is sulfasalazine. It is not absorbed when administered orally or as a suppository and, therefore, *Sulfasalazine is reserved for treatment of chronic inflammatory bowel disease (IBD) (for example, ulcerative colitis).
-
In burn units, creams ((local/topically)) of silver sulfadiazine or sulfamylon have been effective in reducing burn-associated sepsis because they prevent colonization of bacteria.
Distribution: Sulfa drugs are high bounding to serum albumin in the circulation, Sulfa drugs distribute throughout the bodily fluids and penetrate well into cerebrospinal fluid even in the absence of inflammation. They can also pass the placental barrier and enter fetal tissues. significance in drug interactions, competes with same plasma proteins; causing severe side effects in neonates
Metabolism: The sulfa drugs are acetylated and conjugated primarily in the liver. The acetylated product is devoid of antimicrobial activity but retains the toxic potential to precipitate (insoluble ) in renal tubules at neutral or acidic pH. This causes crystalluria (stone formation due to perticipation of metabolite) and, therefore potential damage to the kidney. Both parent compounds and metabolites are excreted in the urine (so, it is useful for the urinary tract infection).
Excretion: = Sulfa drugs are eliminated by glomerular filtration and secretion and require dose adjustments for renal dysfunction. Sulfonamides may be eliminated in breast milk.
Therapeutic Uses
Systemic uses: shrinking uses due to……………………? Resistance is generally irreversible
But its combinations is used ……………see below
Local uses:
- Prevention of infections in burned patients e.g silver sulfadiazine.
- Sulfacetamide is used topically for treatment of ocular infections.
Adverse Effects
Mild e.g. nausea, vomiting, headache, cyanosis and arthritis.
Serious:
-
crystalluria due participated of sulfonamide Prevention by: Give excess fluids (at least 2 liters urine/day) Give alkalinizing agent e.g. citrate, bicarbonate to prevent precipitation (i.e. increase solubility of sulfonamide and its acetylated form).
-
Allergic reactions: ( Stephen-Jhonson-Syndrome ) Hypersensitivity: Hypersensitivity reactions, such as rashes, angioedema or Stevens-Johnson syndrome, may occur. Stevens-Johnson syndrome is a rare, serious disorder of skin and mucous membranes. It’s usually a reaction to a medication or an infection. Often, it begins with flu-like symptoms, followed by a painful red or purplish rash that spreads and blisters. Then the top layer of the affected skin dies, sheds and then heals.
-
Hematopoietic disturbances: Hemolytic anemia is encountered in patients with glucose-6-phosphate dehydrogenase ( G6PD) deficiency. Granulocytopenia and thrombocytopenia can also occur.
-
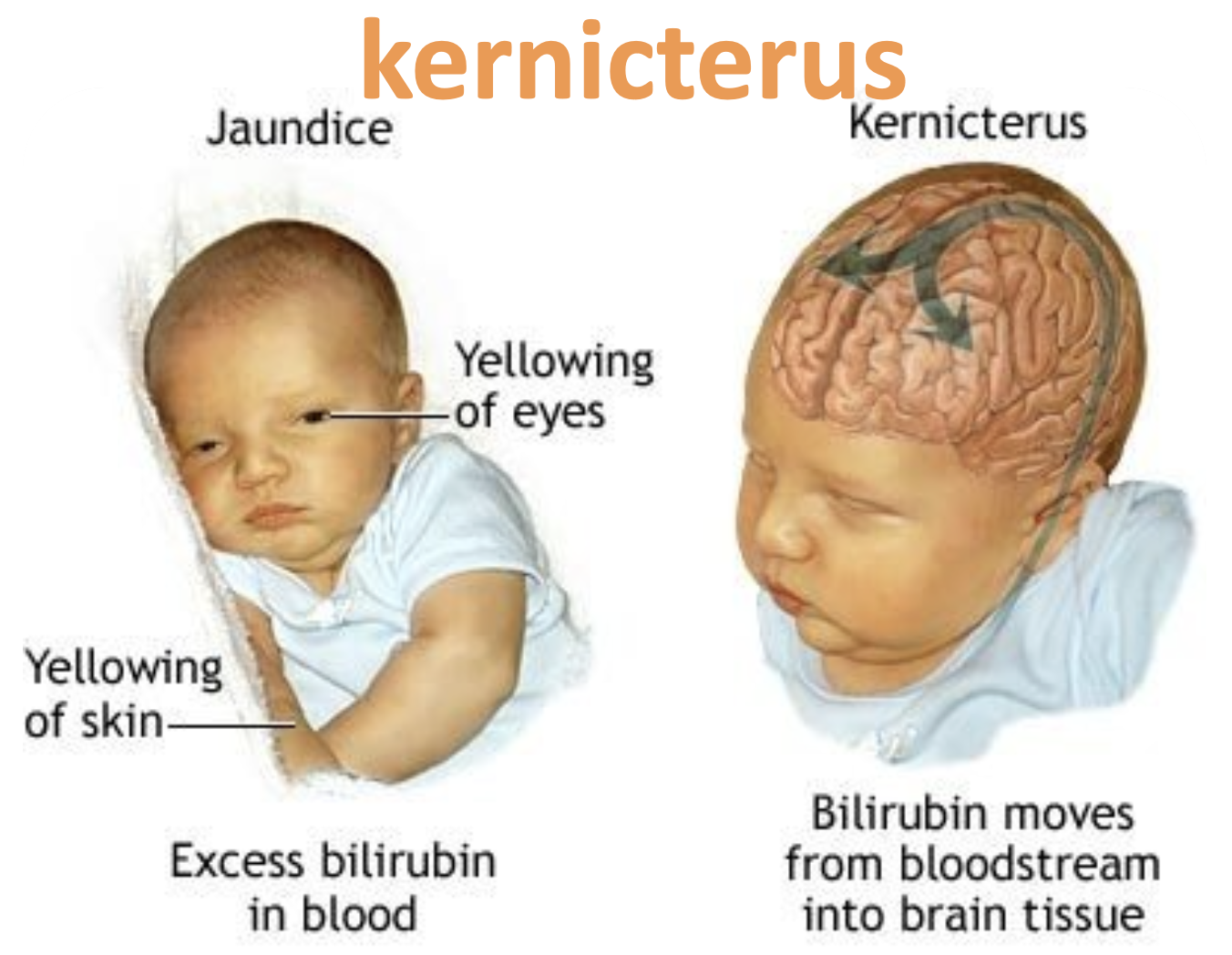
Kernicterus: This disorder may occur when given in last 2 weeks of pregnancy or in newborns and infants, because sulfa drugs displace bilirubin from binding sites on serum albumin. The bilirubin is then free to pass into the CNS, because the blood– brain barrier is not fully developed.. It occurs with long acting sulfonamides if used for long time because sulfonamides compete with bilirubin for albumin leading to high free bilirubin concentration in blood.
-
Drug potentiation: Transient potentiation of the anticoagulant effect of warfarin results from the displacement from binding sites on serum albumin. Serum methotrexate levels may also rise through its displacement.
-
Superinfection with poorly absorbed sulfa).